Anti-Phospholipase A2 Receptor Antibody Testing to the Rescue
Corresponding author: A.S. Nath, Department of Nephrology, Nizams Institute of Medical Sciences, Punjagutta, Hyderabad - 500 082, Telangana, India. E-mail: dr.a.s.nath@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Nath AS, Herur S, Taduri G, Guditi S, Kalidindi RK, Murugan P, et al. Anti-Phospholipase A2 Receptor Antibody Testing to the Rescue. Indian J Nephrol. 2025;35:301-3. doi: 10.25259/ijn_413_23
Abstract
Serological testing for M-type anti-phospholipase A2 receptor antibodies (antiPLA2R Ab) has abrogated the need for kidney biopsy to diagnose membranous nephropathy in the appropriate clinical setting. We report a case of a 63-year-old hypertensive male who presented with nephrotic syndrome associated with autosomal dominant polycystic kidney disease which was effectively diagnosed with the use of antiPLA2R Ab test. He achieved complete remission upon treatment with Rituximab. Hitherto, all anecdotal case reports of this uncommon association were diagnosed only by kidney biopsy. We highlight the usefulness of PLA2RAb especially in such cases of difficult-to-biopsy kidneys.
Keywords
Membranous nephropathy
Nephrotic syndrome
PLA2R
Polycystic kidneys
Rituximab
Introduction
Serological testing for M-type antiphospholipase A2 receptor antibodies (antiPLA2R Ab) has abrogated the need for kidney biopsy to diagnose membranous nephropathy in appropriate clinical settings.1 The use of enzyme-linked immunosorbent assay testing for antiPLA2R Ab to diagnose and monitor response to treatment has been endorsed in the 2021 guideline by the Kidney Diseases Improving Global Outcomes.2 We report a case of nephrotic syndrome associated with autosomal dominant polycystic kidney disease, which was effectively diagnosed and managed using an antiPLA2R Ab test.
Case Report
A 63-year-old man with a history of well-controlled hypertension for the past 5 years presented to the Nephrology services of our hospital with complaints of progressive pedal edema over 1 month. There were no other symptoms. On examination, the patient had bilateral pedal edema and blood pressure was 130/80 mmHg. The rest of the systemic examination was normal except for a ballotable kidney on the left side.
Investigations showed Hemoglobin of 14.2 g/dL, serum creatinine of 1.2 mg/dL, HbA1c 5.9%, fasting total cholesterol of 362 mg/dl, total protein of 5.9 g/dL, and serum albumin of 2.7 g/dL. A urine examination showed 4+ albumin, nil RBC, and 1-2 pus cells. A spot urine protein-creatinine-ratio was 7.71 and 24-hour urinary proteins were 6,200 mg/day. Hepatitis B surface antigen, anti-Hepatitis C antibodies, and HIV antibodies were negative. Anti-nuclear factor antibodies were negative.
Ultrasonography revealed bilateral polycystic kidneys with a complex cyst in the lower pole of the left kidney. A contrast-enhanced computed tomography of the abdomen showed the right kidney at 15.0 × 7.7 cm and the left kidney at 23.4 × 10.6 cm. The lower pole of the left kidney showed a Bosniak IIF cyst of 12.2 × 13.0 × 13.0 cm [Figure 1]. There were few simple hepatic cysts. Other age-appropriate cancer screening (serum total PSA, chest X-Ray, stool occult blood testing was done; the patient was not willing for a colonoscopy) were also negative. An FDG-PET computed tomography scan was done which did not show any significant tracer uptake.
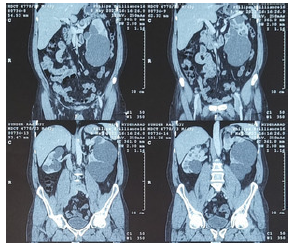
- Contrast-enhanced computed tomography scan showing bilateral asymmetrical polycystic kidneys.
Serum PLA2R ab level was 78 IU/mL and a diagnosis of primary membranous nephropathy associated with Autosomal dominant polycystic kidney disease (ADPKD) was made. He had no known family history of ADPKD or renal failure and his immediate kin were advised to undergo screening ultrasound. His only daughter, 31 years old, was found to have bilateral kidney cysts and liver cysts.
He was treated with Rituximab at a dose of 1 g, 2 weeks apart, and followed up. At 3 months, his PLA2R was 23 IU/mL, serum albumin 3.2 g/dL, and spot urine PCR 2.8. At 6 months, the PLA2R was negative and serum albumin 3.7 g/dL and spot urine PCR 0.5—a complete remission was achieved [Table 1]. The patient is asymptomatic and is on angiotensin receptor blocker telmisartan for his hypertension and febuxostat for hyperuricemia and is on follow-up.
| Parameter | At diagnosis | At 3 months | At 6 months |
|---|---|---|---|
| Serum PLA2R* | 78 IU/mL | 23 IU/mL | 5 IU/mL |
| Proteinuria (UPCR)# | 7.71 | 2.80 | 0.51 |
| Serum Albumin | 2.7 g/dL | 3.2 g/dL | 3.7 g/dL |
*Antiphospholipase A2 Receptor antibody. #Urine Protein-Creatinine-Ratio
Discussion
Although anecdotal case reports of nephrotic syndrome in patients with ADPKD are documented,3 with various histologies like focal segmental glomerulosclerosis, IgA nephropathy, diffuse proliferative glomerulonephritis, and membranous nephropathy,4 all the cases had undergone an open/laparoscopic kidney biopsy and carried a tissue diagnosis. This is probably because all such case reports were reported prior to 2009—before the diagnosis of the target antigen in membranous nephropathy.5
To our knowledge, this is the first case of this uncommon association diagnosed and managed without the need for a kidney biopsy. We highlight the usefulness of PLA2RAb especially in such cases of difficult-to-biopsy kidneys so that the patient care can be delivered uncompromised without the need and risks of an invasive procedure.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
References
- The Anti-PLA2R antibody in membranous nephropathy: what we know and what remains a decade after its discovery. Kidney Int. 2019;96:1292-302.
- [CrossRef] [PubMed] [Google Scholar]
- KDIGO 2021 Clinical practice guideline for the management of glomerular diseases. Kidney Int. 2021;100:S1-276.
- [CrossRef] [PubMed] [Google Scholar]
- Autosomal dominant polycystic kidney disease with diffuse proliferative glomerulonephritis-an unusual association: A case report and review of the Literature. J Med Case Rep. 2010;4:125.
- [CrossRef] [PubMed] [Google Scholar]
- Membranous glomerulonephritis associated with autosomal dominant polycystic kidney disease. Nephron. 1993;65:316-7.
- [CrossRef] [PubMed] [Google Scholar]
- Profile of indian patients with membranous nephropathy. kidney Int Rep. 2020;5:1551-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







