Translate this page into:
Beyond the Initial Episode, Recurrent Hemolytic Uremic Syndrome Unveiled
Corresponding author: Nitish Kumar, Division of Pediatric Nephrology and Department of Pediatrics, Institute of Medical Sciences, Banaras Hindu University, Varanasi, India. E-mail: doctornitishkumar@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Abhinay A, Vijayakumar V, Kumar N, Panda S. Beyond the Initial Episode, Recurrent Hemolytic Uremic Syndrome Unveiled. Indian J Nephrol. 2024;34:675. doi: 10.25259/IJN_235_2024
Dear Editor,
Atypical hemolytic uremic syndrome (aHUS) is characterized by hemolytic anemia, thrombocytopenia, and acute kidney injury (AKI). It occurs due to an underlying complement pathway dysregulation with a genetic predisposition.1,2 We report a case of aHUS with CD46 mutation.
A 4-year-old female had fever, vomiting, lethargy, and reduced urine output. She had shock with respiratory failure. A written informed consent was obtained from the father. Investigations revealed severe metabolic acidosis, hyperkalemia, hyponatremia, urea, and creatinine levels of 275 and 9.5 mg/dl, respectively. ECG revealed tall T waves. She was given respiratory support and peritoneal dialysis. Hemogram showed anemia with thrombocytopenia and schistocytes (5%). Urinalysis revealed nephritic range proteinuria and microscopic hematuria. The serum lactate dehydrogenase was highly elevated. Septicemia, malaria, leptospirosis, dengue, and DIC were ruled out. Her renal function slowly improved. Enalapril was started for hypertension. Serum complement levels were normal, and anti-factor H (FH) antibodies were nonreactive. After 2 months, she had a similar presentation with AKI, hyperkalemia, and microangiopathic hemolytic anemia. Whole exome sequencing revealed a novel mutation (p.Asn235Lysfs*21) in exon 6 in CD46 gene, which was later confirmed with Sanger sequencing [Figure 1]. Sibling screening turned out to be normal. The child is currently normotensive and achieving age-appropriate growth parameters.
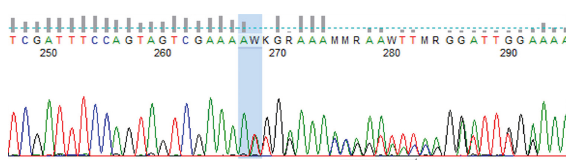
- Sanger sequencing data (electropherogram) showing nucleotide change at c.704dupA (p.Asn235Lysfs*21) in the CD46 gene. Red, green, black, and blue color peaks show thymine, adenine, guanine, and cytosine bases, respectively.
Heterozygous loss-of-function human CD46 mutations account for 5–20% of all aHUS cases with high rates of recurrence after the first flare.3 Plasma exchange, or plasma infusions, remains the chief option for patients with aHUS without anti-FH antibodies in India.1 Patients with aHUS due to the CD46 mutation show a low risk of posttransplant recurrence.4
Acknowledgement
We thank all the residents and staff who were involved in the care of this patient.
Conflicts of interest
There are no conflicts of interest.
References
- Hemolytic uremic syndrome in a developing country: Consensus guidelines. Pediatr Nephrol. 2019;34:1465-82.
- [CrossRef] [PubMed] [Google Scholar]
- Relative role of genetic complement abnormalities in sporadic and familial aHUS and their impact on clinical phenotype. Clin J Am Soc Nephrol. 2010;5:1844-59.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The genetics of atypical hemolytic uremic syndrome. Med Genet. 2018;30:400-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Complement genes strongly predict recurrence and graft outcome in adult renal transplant recipients with atypical hemolytic and uremic syndrome. Am J Transplant. 2013;13:663-75.
- [CrossRef] [PubMed] [Google Scholar]







