Translate this page into:
Bile Cast Nephropathy, An Often-Missed Diagnosis
Address for correspondence: Dr. Sashi Kiran Annavarajula, Consultant Nephrologist, Yashoda Hospital, Malakpet, Hyderabad-500 036, Telangana, India. E-mail: sashikiran_a@yahoo.co.in
-
Received: ,
Accepted: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor,
Bile cast nephropathy (BCN), also known as cholemic nephropathy (CN), refers to acute kidney injury (AKI) in a patient with jaundice. BCN rarely finds a mention in the current medical literature, making it one of the rarely thought of and, more importantly, a diagnosis often missed antemortem.[1] Here we report a patient who presented with AKI along with very high bilirubin.
A 50 years old diabetic for the past 5 years, and an alcohol consumer for the past 15 years, developed an acute deterioration of his liver function following an increase in alcohol consumption. He self-medicated with some herbal preparation for a couple of days, following which he developed decreased urine output and breathlessness. At the time of his presentation to us, he had jaundice, was anuric, and had fluid overload. Laboratory evaluation revealed his serum bilirubin to be 23 mg/dL; prothrombin time was prolonged (INR~2); AST and ALT were 76 U/L and 84 U/L, respectively; and serum creatinine was 9.2 mg/dL. His urine had a bland sediment. ANA and ANCA (P and C) were negative, and his complement (C3 and 4) levels were normal. Evaluation for hepatotropic viruses and autoimmune hepatitis were not contributory. Ultrasound examination of the abdomen revealed coarse echo texture of the liver along with splenomegaly. The kidneys were normal in size but had increased echo texture, with no ascites. Upper GI endoscopy revealed esophageal varices. He was started on hemodialysis, and fresh frozen plasma (FFP) was transfused to correct coagulopathy. Hence, it was apparent that he had acute hepatitis superimposed on alcohol-induced cirrhosis of liver with portal hypertension, but the cause of renal failure was not evident. Because coagulopathy was difficult to correct, renal biopsy was performed by a transjugular approach. The renal biopsy was suggestive of BCN [Figures 1, 2, and 3]. Hence, he was taken up for plasmapheresis, and in each session, one plasma volume was exchanged with an equal amount of FFP. His renal function started to improve following ten sessions of hemodialysis and five sessions of plasmapheresis.

- Reddish-brown pigmented casts in medullary collecting ducts
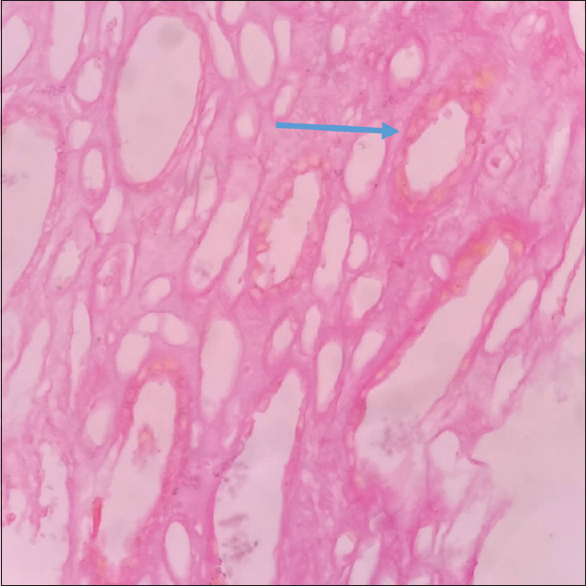
- Hall’s/Fouchet’s test: Greenish-yellow pigment observed within tubular epithelial cells (blue arrow)

- Hall’s/Fouchet’s test: Greenish-yellow pigment observed within the tubular lumen as a cast (red arrow). Acute tubular injury manifested by dilated tubules and attenuated epithelium
Our patient presented with very high bilirubin and AKI. He did not have any signs of decompensated liver failure, and his urine sediment was bland. This made us consider diseases other than hepatorenal syndrome (HRS). As his urine sediment was bland with no RBCs and had insignificant proteinuria, two possibilities were considered. The first was acute interstitial nephritis due to the consumption of indigenous herbal preparation, and the second was acute tubular necrosis (ATN) of unknown etiology. Performing renal biopsy by using the transjugular approach was a crucial step in the diagnosis of his disorder.
Once the diagnosis of BCN was made, the next step for us was to reduce the level of serum bilirubin and correct his coagulopathy. We felt that the best way to achieve this was to perform plasmapheresis with fresh frozen plasma as a replacement along with hemodialysis as hemodialysis alone did not show any benefit. Because various medical therapies such as steroids, cholestyramine, ursodeoxycholic acid, and lactulose have shown little benefit, they were not relied upon. Our treatment (plasmapheresis along with hemodialysis) resulted in improvement of his condition, and his renal function continues to be normal at 6 months.
Bile cast nephropathy is a rare disorder and is often missed for two reasons. The first being a clinical bias to label a patient with jaundice and AKI to have “hepatorenal syndrome” (HRS), and the second is the hesitation to perform a kidney biopsy in a patient who has coagulopathy. Most of the case series on BCN are post-mortem studies,[23] and only a few prospective studies have looked into this entity.[4]
The role of bile acids and bilirubin in causing BCN in liver diseases is incompletely understood. The bile may be directly toxic to the renal tubular cells. Excessive bilirubin tends to cause oxidative damage to the cell membrane along with the uncoupling of oxidative phosphorylation in the mitochondria.[5]
There are currently no accepted treatment guidelines for this condition. The emphasis in all treatment strategies is to correct the cause of hyperbilirubinemia if it is present. This strategy is helpful in the initial course of the disease but becomes less effective in established disease. Some of the extracorporeal treatment options that have been tried include plasmapheresis, molecular adsorbents recycling system (MARS), and coupled plasma filtration adsorption (CPFA). These extracorporeal therapies help in allowing liver regeneration after an acute injury and also help correct bleeding diathesis. Many of these therapies need to be tested in appropriate clinical trials for this condition.
In conclusion, BCN is an underdiagnosed entity that results from various insults to the kidney. Early diagnosis with a low threshold for performing a renal biopsy is essential in establishing a diagnosis, and judicious use of extracorporeal therapies may be helpful in the management of this condition.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Bile cast nephropathy:A case report and review of the literature. World J Gastroenterol. 2016;22:6328-34.
- [Google Scholar]
- Bile cast nephropathy in patients with acute kidney injury due to hepatorenal syndrome:A postmortem kidney biopsy study. J Clin Transl Hepatol. 2017;5:92-100.
- [Google Scholar]
- Bile cast nephropathy is a common pathologic finding for kidney injury associated with severe liver dysfunction. Kidney Int. 2013;84:192-7.
- [Google Scholar]
- Urinary bile casts in bile cast nephropathy secondary to severe falciparum malaria. Clin Kidney J. 2016;9:644-8.
- [Google Scholar]
- Bile acids trigger cholemic nephropathy in common bile-duct-ligated mice. Hepatology. 2013;58:2056-69.
- [Google Scholar]






