Translate this page into:
Bioimpedance Spectroscopy-Guided Ultrafiltration Normalizes Hydration and Reduces Intradialytic Adverse Events in Hemodialysis Patients
Address for correspondence: Dr. R. A. Annigeri, Apollo Hospital, Gream's Lane, Chennai - 600 006, Tamil Nadu, India. E-mail: drrajeevannigeri@hotmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Chronic fluid overload as well as excessive fluid removal are associated with increased morbidity and mortality in hemodialysis (HD) patients. The clinical method to probe the dry weight is often inaccurate and the bioimpedance spectroscopy (BIS) is shown to improve the accuracy. We compared the impact of BIS and clinical methods to guide ultrafiltration (UF) in a randomized controlled study on the intradialytic complications and blood pressure control in prevalent HD patients. Fifty patients on maintenance HD were randomized to BIS method (BIS-group) and clinical method (CL-group) to guide UF. The body composition monitor (BCM) was done post-HD in all patients at baseline and 2-weeks interval during the study period of 6 months to determine the hydration status, but the result was revealed only to the nephrologist managing the patients in BIS-group to probe the dry weight. The endpoints of the study were blood pressure control, intradialytic complications and anti-hypertensive drug burden. The mean age was 56.0 ± 12.0 years and 70% were male. There was significant increase in patients with normal hydration in BIS-group (20% vs. 88%, p = 0.0001), but remained similar to baseline in CL-group (40% vs. 48%, p = 0.3) at 6 months. The incidence of intradialytic hypotension was significantly reduced in BIS-group (4.84 ± 3.0 vs. 2.8 ± 3.13 events/patient/6 months, p = 0.003). There was 35% reduction in hypertensive pill burden in BIS-group with similar blood pressure, compared to CL-group. Post-dialysis underhydration was more common than over or normal hydration at baseline in our population, indicating that clinical method to probe dry weight often resulted in hypovolemia. BIS method to determine dry weight resulted in normalization in volume status and consequently resulted in significant reduction in intradialytic hypotension and anti-hypertensive pill burden over 6-month period.
Keywords
Bioimpedance
chronic hemodialysis
dry weight
intradialytic hypotension
Introduction
The correction of fluid overload and control of hypertension has been a priority since hemodialysis (HD) became a viable therapy for end-stage renal disease (ESRD) patients in 1960's.[1] To achieve this goal, the concept of “dry weight” evolved to guide ultrafiltration (UF) to achieve normal hydration at the end of each HD session.[234] In its basic definition, dry weight is clinically established and generally reflects the lowest post-dialysis weight that a patient can tolerate without hypotension and intradialytic symptoms such as dizziness, cramps, without evidence of fluid overload and a reasonable control of blood pressure.[24] Probing the dry weight by clinical method has evolved over several decades and has been shown to improve surrogates of cardiovascular outcomes, which is the major contributor to mortality in this population.[56] Overhydration (OH) is common in HD population and is associated with increased mortality[78] and the efforts to correct OH have been shown to improve survival in HD population.[79] On the other hand, aggressive pursuit of probing the dry weigh clinically has several drawbacks. Hypovolemia, resulting from overzealous UF may cause intradialytic hypotension,[10] which is a risk factor for myocardial dysfunction and ischemia,[1112] endotoxemia due to gut ischemia,[13] clotting of vascular access[14] and long-term mortality.[151617] Recurrent intradialytic hypotension can cause myocardial fibrosis leading to cardiac dysfunction in the long term, potentially contributing to cardiovascular morbidity and mortality[18] and neurological dysfunction by inducing white matter changes in the brain.[19] The ability to achieve normal volume status by probing the dry weight clinically is not satisfactory, often resulting in either over or underhydration.
Advances in bioimpedance technology have provided an opportunity to improve our ability to probe the dry weight more accurately to achieve normal volume status in HD patients.[20] In recent years, bioimpedance spectroscopy (BIS) technique has gained popularity in assessing the body composition due to its simplicity and low cost. The body composition model describes the intra- and extracellular water content of lean tissue mass (LTM), adipose tissue mass (ATM) and excess fluid OH.[21] The LTM, ATM and OH are obtained from measurements of body weight, height and whole body intracellular water (ICW) and extracellular water (ECW) determined by BIS.[22] Each of these compartments has a specific composition and contains a known quantity of water per mass of tissue. The OH is almost 100% ECW, whereas the water of LTM and ATM consist of differing proportion of ECW and ICW in addition to solid components. The BIS has been validated to accurately determine body composition and hydration status in health and disease[2023] and in HD populations.[24] Several studies have shown an improvement in surrogates of cardiovascular outcomes[72526] and mortality in HD population,[727] when BIS was used to guide determination of dry weight. However, its use in HD patients has not gained widespread clinical acceptance yet, since there is a paucity of quality studies and most reported studies originate from few select centers.
We assessed the utility of BIS-guided UF in HD patients on the intradialytic complications and blood pressure control in prevalent HD patients in a prospective randomized controlled (RCT) study.
Subjects and Methods
Fifty patients of ESRD undergoing maintenance HD twice or thrice a week in two HD units, who consented to participate in the prospective study were randomly assigned to one of the two groups: 1) BIS-group and 2) clinical method group (CL-group). The hospital-based ethics committee approved the study and written informed consent was taken from the participants. The patients with following attributes were excluded from the study: age <15 years, on HD for <3 months, acute kidney injury, malignancy, pregnancy, major surgical procedure within 3 months, planned to undergo renal transplantation within 6 months, amputees, pace maker insertion and metals other than coronary stents.
Clinical, demographic and laboratory data
The demographic data such as age, gender, duration and frequency of HD, cause of ESRD, presence of diabetes and hypertension were collected. The comorbidity was assessed and quantified using the Charlson's comorbidity index.[28] The pre-HD laboratory tests were performed mid-week and included blood urea, serum creatinine, serum potassium, hemoglobin and serum albumin. Dialysis adequacy was assessed by Kt/V urea and was calculated from the pre-dialysis and post-dialysis blood urea concentration at the time of enrollment.
Assessment of blood pressure control
Blood pressure (BP) was measured in the non-fistula arm before and after each session of HD and every 15 min during HD. Number and dose of antihypertensive drugs was noted. The post-HD blood pressure was used to assess the control of blood pressure. The antihypertensive medications were assigned a score to quantify the burden of antihypertensive drugs; the maximum dose was assigned a score of 1 and the dose of antihypertensive was calculated in fraction thereof if patient was not taking the maximum dose of the given medications. Maximum dosage of each antihypertensive drug was determined based on the published drug dose guidelines.[29]
Monitoring during hemodialysis
All patients were closely monitored for intradialytic hypotension and muscle cramps. Intradialytic hypotension was defined as systolic BP <100 mmHg or requiring minimum 100 ml saline to reverse hypotension and symptoms. Assessment of dizziness and cramps during or after dialysis was based on the subjective symptoms.
Assessment of quality of life
Quality of life (QoL) was assessed by the Short Form-36 (SF-36) score[30] at enrolment and at the end of the study. The linguistic translation of the SF-36 questionnaire was done when necessary.
Bioimpedance spectroscopy
The hydration status was assessed half an hour after the HD session in all patients by body composition monitor (BCM) machine which uses BIS technology, at the beginning of the study and at an interval of 15 days during the entire study period. A portable multi-frequency whole-body BCM machine (Fresenius medical care, Germany) was used to assess the body composition and the electrodes were placed opposite to the side of location of vascular access. The hydration status was determined using computer software integrated into the BCM machine and was expressed as liters (L) over or under the normal value. BCM determines total body water (TBW), ECW volume, ICW and OH automatically. Absolute OH is defined as the difference between the patient's expected ECW under normal physiologic conditions and actual ECW, whereas relative OH is defined as the ratio of OH/ECW. Normal hydration is defined when hydration is between the 10th and 90th percentiles for healthy age- and gender-matched individuals from the reference population, that is, −1.1 to 1.1 L, with volumes below and above this range defining underhydration and OH, respectively.[24]
Intervention
All patients were seen by a nephrology resident as well as the nephrologist during each HD session during the entire study period. The information of BCM results was revealed to the nephrologist managing the patients in BIS-group to probe the dry weight, but was not compelled to fix dry weight based on BCM results. BCM results in the CL-group were not revealed to the attending nephrologist and hence dry weight was determined in this group solely based on clinical method.
Endpoints
The study period was 6 months. The primary endpoints of the study were blood pressure control and intradialytic complications. The secondary endpoint of the study was antihypertensive drug burden.
Statistical methods
The continuous data are presented as mean with standard deviation (SD) and the categorical data are expressed either as percentage or proportion. A comparison between the two groups was performed using Student's t-test (two-tailed) for normally distributed continuous variables, whereas the Mann–Whitney's U test was used for non-normal distributed variables. Comparisons of all the categorical variables are done by Chi-square (χ2) or Fisher's exact test. A p value <0.05 was considered statistically significant. The statistical analysis was performed by the statistical package for social sciences (SPSS) software version 17.0 (IL, Chicago, USA).
Results
The mean age was 56.0 ± 12.0 years and 70% were male. The baseline demographic data between the two groups are shown in Table 1. The hydration parameters at baseline and at 6 months and their comparison between the two groups are shown in Table 2. Figure 1 shows the distribution of underhydration, normal hydration and OH at baseline and at 6 months between the two groups. The distribution of relative OH (OH/ECW >15%) was 3 (12%) in both CL-group and BIS-group at baseline and none in CL-group and 1 (4%) in BIS-group at 6 months. Figure 2 shows the change in the absolute OH from baseline to 3 and 6 months in two groups. The absolute hydration (L) at baseline was −0.42 ± 1.8 and −0.084 ± 3.0 (0.63) in CL and BIS groups, respectively, at 3 months was −0.08 ± 1.5 and 0.47 ± 1.3 (0.17) in CL and BIS groups, respectively and was −0.44 ± 1.2 and 0.16 ± 0.8 (p = 0.04) in CL and BIS groups, respectively. Figure 3 shows details of change in hydration status over a period of 3 and 6 months in patients who were overhydrated and underhydrated at baseline in CL and BIS groups. Table 3 shows the intradialytic adverse events between the two groups during the study period of 6 months. The comparison of BP measurements and antihypertensive medications at baseline and at 6 months is shown in Table 4. The SF-36 scores were similar between two groups at 6 months.
| All patients (n=50), n (%) | CL-group (n=25), n (%) | BIS-group (n=25), n (%) | P | |
|---|---|---|---|---|
| Age (years) | 56.0±12.0 | 55.24±10.62 | 56.76±13.46 | 0.484 |
| Sex: Male (%) | 35 (70) | 17 (68) | 18 (72) | 0.758 |
| Charlson’s co-morbidity score | 5.86±2.1 | 6±2.12 | 5.72±2.03 | 0.161 |
| Kt/V per session | 1.6±0.19 | 1.56±0.17 | 1.64±0.19 | 0.107 |
| Frequency of HD (thrice a week) | 40 (80) | 19 (76) | 21 (88) | 0.73 |
| HD vintage (months) | 29.2±25.8 | 27.0±16.1 | 31.5±32.9 | 0.53 |
| BMI | 23.9±4.4 | 24.69±4.17 | 23.08±4.56 | 0.112 |
| Post-HD systolic BP (mm Hg) | 133.8±15.6 | 132±15 | 135.6±16.35 | 0.421 |
| Post-HD diastolic BP (mm Hg) | 79.8±4.7 | 79.2±4.93 | 80.4±4.54 | 0.369 |
| Antihypertensive drug score | 0.91±0.73 | 0.87±0.84 | 0.92±0.62 | 0.525 |
| Serum albumin (g/dl) | 3.77±0.23 | 3.80±0.24 | 3.73±0.21 | 0.304 |
| SGA score | 14.08±4.78 | 14.64±5.99 | 13.52±3.19 | 0.884 |
CKD: Chronic kidney disease, CIN: Chronic interstitial nephritis, HD: Hemodialysis, BP: Blood pressure, BMI: Body mass index, SGA: Subjective global assessment, BIS: Bioimpedance spectroscopy, CL: Clinical
| All patients (n=50) | CL-group (n=25) | BIS-group (n=25) | P | |
|---|---|---|---|---|
| Weight (kg) | ||||
| Baseline | 62.4±12.2 | 64.47±13.66 | 60.26±10.39 | 0.23 |
| At 6 months | 62.26±11.95 | 64.17±13.1 | 60.34±10.6 | 0.26 |
| TBW (L) | ||||
| Baseline | 28.45±5.57 | 28.28±6.03 | 28.62±5.18 | 0.83 |
| At 6 months | 26.8±5.7 | 27.3±6.1 | 25.94±5.3 | 0.31 |
| ECW (L) | ||||
| Baseline | 13.42±3.04 | 13.23±3.40 | 13.60±2.68 | 0.67 |
| At 6 months | 12.9±2.6 | 13.1±2.7 | 12.64±2.6 | 0.55 |
| Absolute OH (L) | ||||
| Baseline | −0.25±2.47 | −0.42±1.80 | −0.08±3.02 | 0.63 |
| At 6 months | −0.282±1.2 | −0.72±1.4 | +0.16±0.79 | 0.01 |
| Relative OH/ECW (%) | ||||
| Baseline | −2.89±18.6 | −4.31±14.56 | −1.46±22.15 | 0.59 |
| At 6 months | −2.38±8.92 | −5.63±9.65 | +0.88±6.87 | 0.008 |
TBW: Total body water, ECW: Extracellular water, OH: Overhydration, BIS: Bioimpedance spectroscopy, CL: Clinical
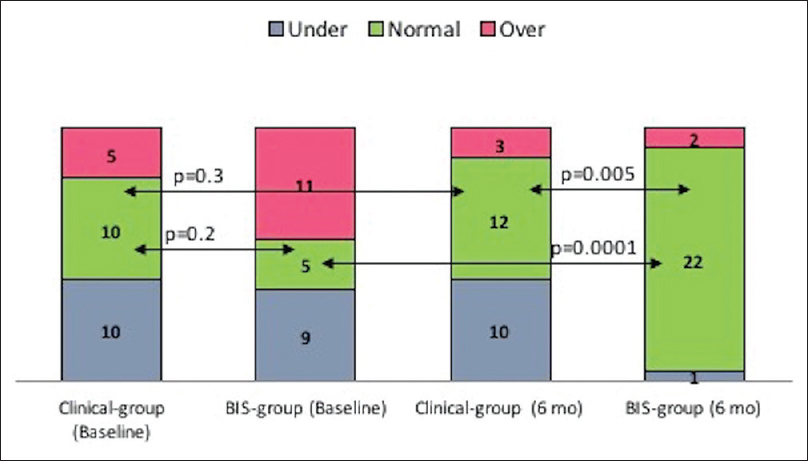
- Comparison of hydration status between BIS and CL groups. (BIS: Bioimpedance spectroscopy, CL: Clinical)
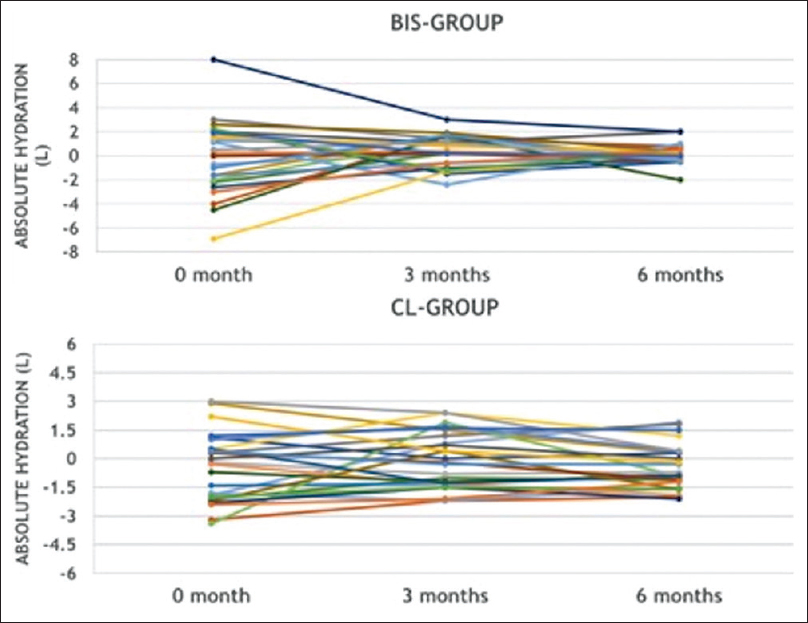
- Change in hydration status from baseline to 3 and 6 months in BIS and CL groups. (BIS: Bioimpedance spectroscopy, CL: Clinical)
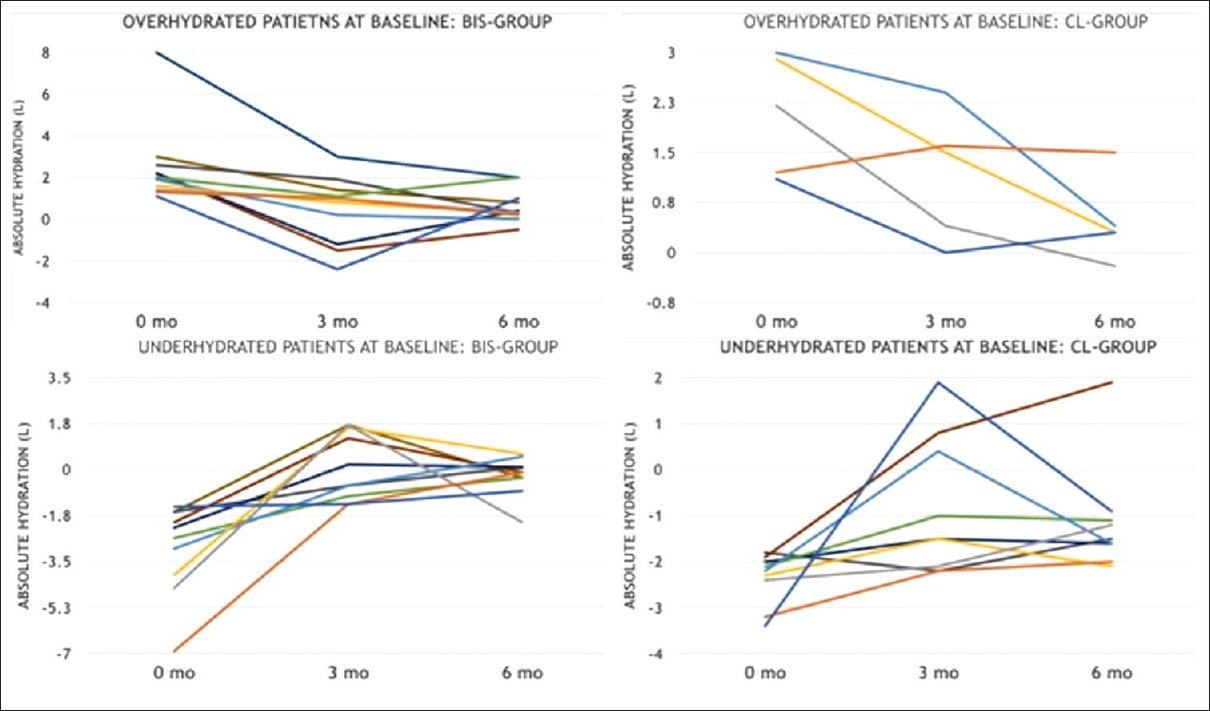
- Change in hydration status from baseline to 3 and 6 months in patients in BIS and CL groups, who were overhydrated and underhydrated at baseline. (BIS: Bioimpedance spectroscopy, CL: Clinical)
| Variable | All patients (n=50) | CL-group (n=25) | BIS-group (n=25) | P |
|---|---|---|---|---|
| Intradialytic hypotension (events/patient/6 months) | 3.82±3.2 | 4.84±3.00 | 2.80±3.13 | 0.003 |
| Dyspnea (events/patient/6 months) | 1.84±1.89 | 2.20±1.93 | 1.48±1.80 | 0.152 |
| Cramps (events/patient/6 months) | 4.54±2.53 | 5.16±2.59 | 3.92±2.34 | 0.048 |
| Dizziness (events/patient/6 months) | 2.06±2.27 | 2.68±2.17 | 1.44±2.23 | 0.012 |
CL: Clinical, BIS: Bioimpedance spectroscopy
| All patients (n=50) | CL-group (n=25) | BIS-group (n=25) | P | |
|---|---|---|---|---|
| Systolic blood pressure | 125±10.9 | 126±11.9 | 124.0±10.0 | 0.52 |
| Diastolic blood pressure | 78.2±4.8 | 79.2±4.9 | 77.2±4.6 | 0.14 |
| Mean arterial pressure | 93.6±5.9 | 94.6±6.4 | 92.6±5.2 | 0.23 |
| Change in systolic blood pressure | -8.8±10.8 | -6.0±11.1 | -11.6±9.8 | 0.066 |
| Change in diastolic blood pressure | -1.6±5.84 | 0±5.8 | -3.2±5.7 | 0.052 |
| Change in mean arterial pressure | -4.0±6.3 | -1.98±6.4 | -5.97±5.6 | 0.024 |
| Antihypertensive drug score | 0.72±0.82 | 0.87±1.0 | 0.57±0.58 | 0.189 |
| Change in the antihypertensive drug score | -0.19±0.46 | -0.02±0.67 | -0.36±0.4 | 0.008 |
All blood pressure measures were done post hemodialysis. CL: Clinical, BIS: Bioimpedance spectroscopy
Discussion
Several studies have shown that both underhydration[78] and OH[151617] are associated with increased morbidity and mortality. The clinical method to probe dry weight is not accurate and often results in OH and underhydration in HD patients. Hence, the aid of technology such as BIS helps the clinician to probe the dry weight to achieve normal hydration more accurately. Indeed, the use of BIS has been shown to improve the hydration status and in turn improves surrogates of poor cardiovascular outcomes[7252631] as well as mortality[2527] in HD population. We studied the impact of BIS-guided probing of dry weight on the short-term outcomes of blood pressure control and intradialytic complications in a prospective randomized study and our results are summarized below.
Effect of bioimpedance spectroscopy-guided dry weight on hydration status
The number of patients with normal hydration (absolute OH within ±1.1 L of normal) was similar between the two groups at baseline [Figure 1], but significantly improved in BIS-group compared to CL-group after 6 months (88% vs. 48%, p = 0.005). Nineteen (38%) of patients were underhydrated (absolute OH < −1.1 L) at baseline, which remained the same in CL-group (40% vs. 40%, p = 1.0), whereas was markedly reduced in the BIS-group (4% vs. 40%, p = 0.005) at 6 months. The OH (absolute OH >1.1 L) was seen in 32% of study population at baseline, which was reduced to 20% at the end of study period. This reduction in absolute OH at 6 months was mainly contributed by the effect of BIS-guided dry weight. Compared to baseline, OH was similar at the end of 6 months in CL-group (20% vs. 12%, p = 0.7), whereas was significantly reduced in BIS-group (44% vs. 8%, p = 0.008). Our results indicate that probing the dry weight by clinical method resulted in underhydration more frequently that OH, thereby exposing our patients to increased risk of intradialytic complications which have potential for long-term adverse outcomes. BIS helped the clinician to guide most of these patients to achieve normal hydration. OH was less common at baseline and BIS-guided probing of dry weight resulted in guiding these patients to normal hydration. Indeed, the incidence of normal hydration was 88% when dry weight was guided by BIS, and it remained largely unchanged (48%) when clinical method was continued to guide dry weight [Figure 1].
OH determined by BIS is reported to be common in HD patients, with a reported incidence of approximately 22–35%.[2432] However, BIS measurements in these studies were done pre-dialysis, whereas we measured hydration status post-HD. We believe that the dry weight is essentially a post-dialysis weight, which represents normal hydration and hence measuring pre-dialysis BCM to measure hydration status is irrational. It is desirable to wait for half an hour post-HD to measure BCM to allow the fluid shifts to equilibrate. Though this is not formally studied, it is accepted that the fluid shift occurs much more rapidly than small solutes and the equilibration of small solutes occurs within half an hour after HD.[33] The studies to assess hydration status using BIS have not given much attention to underhydration and our study is the first to quantify the underhydration status after HD session. The high incidence of underhydration at the end of HD in our study at baseline which remained unchanged in CL-group is likely to be the result of aggressive application of probing dry weight in our study population, which is likely to cause more harm. We caution against the aggressive pursuit of probing dry weight, which could result in chronic underhydration as seen in study population. Wabel et al. reported underhydration (OH <−1.1 L) in 5.4% of patients, but their assessment was done pre-HD.[24]
Several authors have reported their experience with hydration status assessed by BIS to manage HD patients. Wizemann et al. used BIS to assess hydration in 269 patients on HD and reported that OH determined by BCM was a strong and independent risk factor of mortality at 3.5 years.[32] Onofriescu et al. assessed hydration status by BCM at baseline in 221 HD patients and showed that OH was associated with increased cardiovascular events [hazard ratio (HR): 2.31] and mortality (HR: 1.87), over a median period of 83 months.[34] Kim et al. performed BCM within the first week of initiation on maintenance HD and classified them as OH (OH/ECW >15%, n = 160) and non-OH (OH/ECW <15%, n = 80) groups and analyzed outcomes at a median period of 24 months. All-cause mortality was significantly increased in patients with OH at the time of initiation of HD (odds ratio: 2.6; p = 0.033).[35]
Impact of bioimpedance spectroscopy-guided dry weight on outcomes
There was no significant difference in the systolic, diastolic and mean arterial BP between the two groups at the end of study period. However, there was significant difference in the change (Δ) in the mean arterial pressure at 6 months compared to baseline in BIS-group (−5.97 ± 5.6 vs. −1.98 ± 6.4 mmHg, p = 0.024), but not in CL-group. In addition, there was 38% reduction in the antihypertensive drug burden at 6 months in BIS-group, whereas it remained unchanged in CL-group, indicating modest benefits in terms of blood pressure control and antihypertensive drug burden over a short period of time in patients with BIS-guided UF. There was no significant impact of BIS-guided UF on the quality of life scores in the short term. However, long-term studies are needed to confirm the benefits of BIS-guided UF on QoL.
Hypotension is known to occur in up to 15–20% of HD sessions.[17] Intradialytic hypotension is associated with increased mortality and hospitalization and hence efforts should be made to minimize hypotensive episodes during HD. In our study, intradialytic hypotensive episodes were significantly lower in BIS-group than in CL-group (2.8 ± 3.13 vs. 4.84 ± 3.0 episodes per patient during entire 6 months, p = 0.008), with an absolute reduction of 42%. In addition, there was a significant reduction in minor complications during HD, such as dizziness and cramps in BIS-group, compared to CL-group [Table 3].
Machek et al. studied 52 HD patients for 1 year and identified 13 (25%) as overhydrated at baseline using BCM.[25] Using BCM to probe the dry weight, they reported a reduction of fluid overload by a mean of 2 L, without increasing intradialytic adverse events and reduction in systolic blood pressure by 25 mmHg and 35% reduction in antihypertensive pill burden. In 12 (23%) patients who experienced repeated intradialytic events during HD, BIS-guided dry weight resulted in an increase in fluid status by 1.3 L and 73% reduction in intradialytic events and with no significant increase in blood pressure, suggesting that BIS improved outcomes in patients who were apparently underhydrated.
Till date two RCTs have compared BCM and clinical-guided probing of dry weight in HD populations. Hu et al. reported in a randomized study of 156 patients showed that BIS-guided dry weight determination resulted in significant reduction in left ventricular mass index over a period of 1 year.[26] In addition, they reported improvement in blood pressure control and arterial stiffness parameter in BIS group compared to CL-group. Onofriescu et al. studied 151 patients on HD in a randomized study and compared dry weight guided by BIS and clinical method.[27] They reported a reduction in all-cause mortality over 3.5 years in patients managed by BIS [unadjusted hazard ratio = 0.1, 95% confidence interval (CI): 0.013–0.8, p = 0.03]. In addition, they reported significant reduction in arterial stiffness, blood pressure and relative fluid overload in patients with BIS-guided dry weight.
We provide an evidence of better hydration status after HD and improved BP control and significant reduction in intradialytic complications in patients with bioimpedance-guided UF. Our results strongly support the notion that use of BCM to probe dry weight helps to reduce the incidence of surrogates of poor cardiovascular outcomes in HD populations, which may improve morbidity and mortality in the long term. BCM machine is expensive and hence cost benefit analysis may be needed before its general acceptance in smaller HD units. However, it is likely to be cost effective in larger HD units.
Strengths and limitations
First, our study is only the third RCT to compare the impact of bioimpedance-guided UF on the blood pressure and intradialytic complications. We provide further evidence that the bioimpedance-guided UF improves hydration status, surrogates of cardiovascular outcomes and intradialytic hypotension, all of which are known to have long-term benefits on mortality. Second, ours is the first such study done in south Asian population and hence validate the use of BCM-guided UF in this population. Third, our study is the first to quantify underhydration and utility of BIS to correct it in HD population, whereas most studies emphasized OH.
Our study has several limitations. First, the number of patients studied was low and was confined to a single center and the duration of study was short. Second, the outcomes studied were surrogates of poor outcomes and not the hard outcomes such as cardiovascular events or death. Third, we did not measure ambulatory blood pressure which is the ideal method to quantify blood pressure control. Fourth, the volume management was not protocol-driven and the clinician was not forced to modify the dry weight to that determined by BIS.
Conclusion
The results of our RCT show that over 6-month period, the BIS-guided UF normalizes hydration status in most of the patients, significantly reduces the incidence of intradialytic hypotension and other symptoms and reduces hypertensive pill burden, compared to those managed by clinical method. Our results show that BIS-guided UF improves patient outcomes and hence suitable for routine clinical application in HD patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Extracellular volume in patients with chronic renal disease treated for hypertension by sodium restriction. Lancet. 1967;2:69-73.
- [Google Scholar]
- Blood pressure control in dialysis patients: Importance of the lag phenomenon. Am J Kidney Dis. 1998;32:720-4.
- [Google Scholar]
- Assessment of dry weight in hemodialysis: An overview. J Am Soc Nephrol. 1999;10:392-403.
- [Google Scholar]
- Probing dry-weight improves left ventricular mass index. Am J Nephrol. 2011;33:373-80.
- [Google Scholar]
- Dry-weight reduction in hypertensive hemodialysis patients (DRIP): A randomized, controlled trial. Hypertension. 2009;53:500-7.
- [Google Scholar]
- Importance of normohydration for the long-term survival of haemodialysis patients. Nephrol Dial Transplant. 2012;27:2404-10.
- [Google Scholar]
- Fluid retention is associated with cardiovascular mortality in patients undergoing long-term hemodialysis. Circulation. 2009;119:671-9.
- [Google Scholar]
- Long-term survival rates in haemodialysis patients treated with strict volume control. Nephrol Dial Transplant. 2006;21:3506-13.
- [Google Scholar]
- Achieving blood pressure targets during dialysis improves control but increases intradialytic hypotension. Kidney Int. 2008;73:759-64.
- [Google Scholar]
- Myocardial contractile function and intradialytic hypotension. Hemodial Int. 2009;13:293-300.
- [Google Scholar]
- Haemodialysis is associated with a pronounced fall in myocardial perfusion. Nephrol Dial Transplant. 2009;24:604-10.
- [Google Scholar]
- Circulating endotoxemia: A novel factor in systemic inflammation and cardiovascular disease in chronic kidney disease. Clin J Am Soc Nephrol. 2011;6:133-41.
- [Google Scholar]
- Intradialytic hypotension and vascular access thrombosis. J Am Soc Nephrol. 2011;22:1526-33.
- [Google Scholar]
- Hemodialysis-associated hypotension as an independent risk factor for two-year mortality in hemodialysis patients. Kidney Int. 2004;66:1212-20.
- [Google Scholar]
- Intradialytic hypotension and risk of cardiovascular disease. Clin J Am Soc Nephrol. 2014;9:2124-32.
- [Google Scholar]
- Intradialytic hypotension: Frequency, sources of variation and correlation with clinical outcome. Hemodial Int. 2014;18:415-22.
- [Google Scholar]
- Hemodialysis-induced repetitive myocardial injury results in global and segmental reduction in systolic cardiac function. Clin J Am Soc Nephrol. 2009;4:1925-31.
- [Google Scholar]
- Are there neurological consequences of recurrent intradialytic hypotension? Semin Dial. 2012;25:253-6.
- [Google Scholar]
- Body fluid volume determination via body composition spectroscopy in health and disease. Physiol Meas. 2006;27:921-33.
- [Google Scholar]
- Importance of whole-body bioimpedance spectroscopy for the management of fluid balance. Blood Purif. 2009;27:75-80.
- [Google Scholar]
- A new technique for establishing dry weight in hemodialysis patients via whole body bioimpedance. Kidney Int. 2002;61:2250-8.
- [Google Scholar]
- A whole-body model to distinguish excess fluid from the hydration of major body tissues. Am J Clin Nutr. 2007;85:80-9.
- [Google Scholar]
- Towards improved cardiovascular management: The necessity of combining blood pressure and fluid overload. Nephrol Dial Transplant. 2008;23:2965-71.
- [Google Scholar]
- Guided optimization of fluid status in haemodialysis patients. Nephrol Dial Transplant. 2010;25:538-44.
- [Google Scholar]
- Effect of fluid management guided by bioimpedance spectroscopy on cardiovascular parameters in hemodialysis patients: A randomized controlled trial. Am J Kidney Dis. 2013;61:957-65.
- [Google Scholar]
- Bioimpedance-guided fluid management in maintenance hemodialysis: A pilot randomized controlled trial. Am J Kidney Dis. 2014;64:111-8.
- [Google Scholar]
- A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40:373-83.
- [Google Scholar]
- Association of Physicians of India. Indian guidelines on hypertension (I.G.H.) – III 2013. J Assoc Physicians India. 2013;61:6-36.
- [Google Scholar]
- The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473-83.
- [Google Scholar]
- Optimal fluid control can normalize cardiovascular risk markers and limit left ventricular hypertrophy in thrice weekly dialysis patients. Hemodial Int. 2012;16:465-72.
- [Google Scholar]
- The mortality risk of overhydration in haemodialysis patients. Nephrol Dial Transplant. 2009;24:1574-9.
- [Google Scholar]
- The post-hemodialysis rebound: Predicting and quantifying its effect on Kt/V. Kidney Int. 1996;50:2094-102.
- [Google Scholar]
- Overhydration, cardiac function and survival in hemodialysis patients. PLoS One. 2015;10:e0135691.
- [Google Scholar]
- Overhydration measured by bioimpedance analysis and the survival of patients on maintenance hemodialysis: A single-center study. Kidney Res Clin Pract. 2015;34:212-8.
- [Google Scholar]







