Translate this page into:
Clinical Characteristics and Outcomes of COVID-Positive Maintenance Hemodialysis Patients: A Study from India
Corresponding author: Manjusha Yadla, Department of Nephrology, Gandhi Medical College, Hyderabad, Telangana - 500 071, India. E-mail: manjuyadla@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Yadla M, Vadakkeveetil AK. Clinical Characteristics and Outcomes of COVID-Positive Maintenance Hemodialysis Patients: A Study from India. Indian J Nephrol. 2024;34:448-52. doi: 10.25259/ijn_288_21
Abstract
Background
This study describes to the clinical features and outcomes of patients on maintenance hemodialysis infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) delta variant.
Materials and Methods
This was a retrospective analysis of case records of patients on maintenance hemodialysis admitted for management of coronavirus disease (COVID) infection. Our teaching hospital, being a state-designated referral center, had COVID admissions from March 2020 till December 2020. Epidemiological and clinical data were collected and analyzed. Factors influencing survival and the survival curve analysis were assessed.
Results
Of a total of 21,228 admissions during the period, 400 patients were referred for nephrology services. Of the 400 referrals, 226 were maintenance hemodialysis patients. Mean age of the group was 50 years, and fever was the most common presenting symptom. On multivariate analysis, factors influencing mortality were found to be older age, presence of diabetes, leukopenia, thrombocytopenia, hypoxemia, need for support, and a higher qSOFA score. The probability of survival of dialysis patients at the end of 19 days was 60%.
Conclusion
During the pandemic by SARS-CoV-2 delta variant, majority of the nephrology referrals were for maintenance hemodialysis patients. Mortality was 38% in the study group, and the factors associated with mortality with a significant hazard ratio were older age and diabetes.
Keywords
COVID
India
Maintenance hemodialysis
Introduction
Maintenance hemodialysis (MHD) patients are vulnerable to infections. With the recent pandemic of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), it was reported that coronavirus disease (COVID)-positive MHD patients have higher mortality compared to COVID-positive general population. It is indeed challenging to run dialysis units during the pandemic as it is difficult to ensure social distancing, and maintain sanitation measures. Also, for the patients, it is even more difficult as they are forced to use dedicated transport, leaving a heavy burden of out-of-pocket expenditure.
Being the designated nodal center for all COVID patients of the state of 3.5 crore population, we developed a dedicated COVID-positive dialysis center in our hospital. During the first wave, all those patients, detected COVID positive on reverse transcription-polymerase chain reaction (RT-PCR), were referred to our center, irrespective of the severity of infection. Of a total of 10,000 plus dialysis population of our state, 2484 patients were undergoing free services under the government cashless scheme and the remaining were in private dedicated centers. During the COVID pandemic, all the COVID-positive dialysis patients were referred to our hospital for dialysis services.
The aim of this study was to analyze the clinical characteristics and outcomes of COVID-positive MHD patients.
Materials and Methods
This was a retrospective study of case records of COVID-positive MHD patients admitted during April 2020–November 2020. Institutional review board approval has been obtained.
Our hospital served as a nodal center for the entire dialysis population of the state. A dedicated unit with 20 hemodialysis machines was dedicated to COVID-positive patients. Dialysis was given as per the indication or as per schedule. Single-use dialyzer, tubings, and transducer, disinfection of the dialysis drain, disinfection of machine, and other sanitizing measures were taken apart from bed distancing. Patients were admitted to the ward or critical care unit depending on their clinical condition.
Those MHD patients with RT-PCR positive for SARS-CoV-2 and those with complete case records were included in the analysis. We determined the clinical characteristics and outcomes of those admitted and analyzed the factors influencing mortality.
Results were analyzed using Statistical Package for the Social Sciences (SPSS) 17. Factors with P < 0.05 were considered significant on univariate and multivariate analyses. Survival analysis curve was estimated.
Results
Of a total of 21228 admissions in the hospital, 400 were nephrology referrals, of whom 226 patients were MHD patients, accounting for 53% of the total referrals [Figure 1]. Patients consents were obtained.

- Referral pattern of nephrology patients. AKI: acute kidney injury, MHD: maintenance hemodialysis, CKD: chronic kidney disease.
Though the initial number of referrals was less, there was a rise between April and July–August, followed by a fall by September [Figure 2]. The increasing and decreasing number of referrals was proportional to the number of admissions in the hospital. All those dialysis patients admitted with SARS-CoV-2 infection were categorized into mild/moderate/severe infection based on history and clinical symptoms [Figure 3].
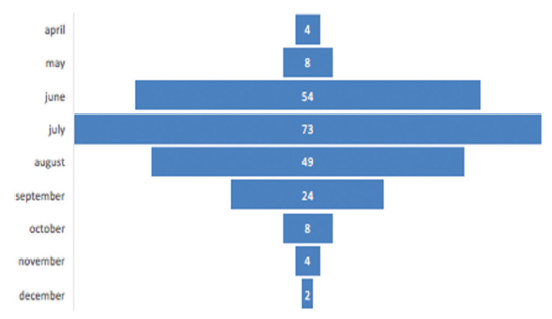
- Frequency of admissions during the pandemic.
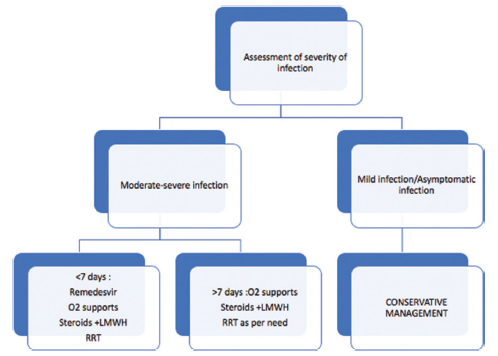
- Management strategy of the hospital. RRT: renal replacement therapy, LMWH: low molecular weight heparin.
Baseline characteristics of the patients are presented in Table 1. The mean age of our group was 50.7 years, and the mean vintage of dialysis was 2.41 years. Men were and women were. Among the clinical manifestations, majority (89%) had fever and breatlessness was present in about 54%. Among the comorbidities, hypertension was present in 73% and diabetes in 30.9% of the patients. Majority of the patients had arteriovenous (AV) fistula as access, though a few patients were on temporary catheters (tunneled and non-tunneled). Mean duration of hospitalization was 11.54 + 4.6 days. All patients were discharged as per the central government guidelines of two sequential negative RT-PCR swabs. We assessed the duration of viral clearance in our study group.
| Mean age (years) | 50.7 |
| Male: female | 172:54 |
| DM | 70 |
| HTN | 167 |
| CAD | 14 |
| Mean duration of dialysis | 2.41 years |
| Fever | 202 |
| Cough | 72 |
| Breathlessness | 122 |
| Diarrhea | 2 |
| Chest pain | 2 |
| Anasarca | 2 |
| Altered sensorium | 7 |
| AVF | 157 |
| Femoral | 3 |
| Internal jugular access | 9 |
| Permcath | 3 |
| Steroids + heparin | 103 |
| Mean SBP | 132.5 |
| Mean DBP | 84.4 |
| Mean pO2 | 82.9 |
| Mean hemoglobin | 8.7 g/dl |
| No. of patients with leukopenia (<4000 cells) | 17 |
| Mean platelet count | 1.28 lakhs/mm3 |
| Mean S. bicarbonate (mEq/l) | 13.5 |
| O2 support | 126 |
| CPAP | 81 |
| Mechanical ventilation | 16 |
| Mean duration of hospitalization | 12.9 days |
| Mean duration of viral clearance | 24.2 days |
| Deaths | 86 |
DBP = diastolic blood pressure, DM = diabetes mellitus, HTN = hypertension, SBP = systolic blood pressure, CPAP = continuous positive airway pressure, AVF = arteriovenous fistula, CAD = coronary artery disease.
Our strategy for assessment of viral clearance was executed more frequently than suggested in the guidelines. [Figure 4]. Our results showed that the viral clearance in dialysis patients started by the third week and reached a peak at the fourth week, though a few patients continued to harbor the virus till the end of the sixth week [Figure 5] (range of time for viral clearance was 7–63 days).
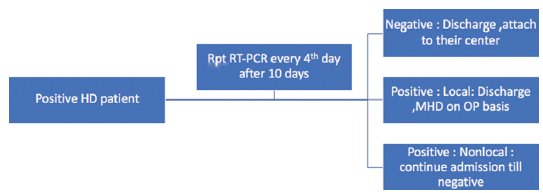
- Viral clearance check strategy. HD: hemodialysis, MHD: maintenance hemodialysis.
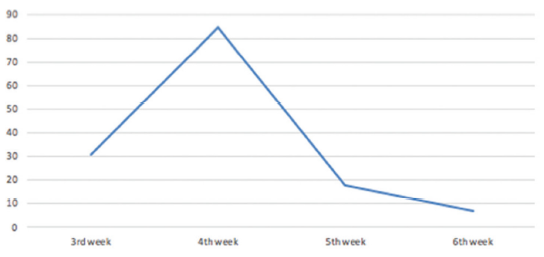
- Weekly viral clearance.
Among the 226 dialysis patients, 86 patients died during the hospital stay. On analysis of factors influencing survival, age, diabetes, presence of breathlessness, delayed presentation to referral center, fever, breathlessness, bicytopenia, higher Quick Sequential Organ Failure Assessment (qSOFA), and the need for mechanical ventilation or noninvasive ventilation were found to be associated with mortality [Table 2]. We attempted the estimation of survival analysis using Kaplan– Meyer curve, where it was observed that 60% of admitted patients survived till 19 days [Figure 6].
| MHD patients with COVID infection (n = 226) | P | ||
|---|---|---|---|
| Death (n = 86) | Discharged (n = 140) | ||
| Age (years) | 57.16 ± 10.66 | 48.29 ± 11.92 | 0.0001* |
| Gender | |||
| Male | 63 | 108 | NS |
| Female | 23 | 32 | NS |
| Smoker | 1 | 1 | NS |
| DM | 28 | 43 | 0.014* |
| HTN | 55 | 134 | NS |
| CAD | 6 | 8 | NS |
| CVD | 2 | 0 | NS |
| Access | |||
| AVF | 81 | 127 | 0.995 |
| Femoral | 1 | 2 | |
| IJV | 3 | 8 | |
| Permacath | 1 | 3 | |
| Fever | 81 (91.1%) | 129 (92.1%) | 0.779 |
| Cough | 19 (33.9%) | 40 (28.6%) | 0.493 |
| SOB | 56 (100.0%) | 53 (37.9%) | 0.0001* |
| MHD duration (years) | 1.99 ± 1.61 | 2.62 ± 2.39 | 0.035* |
| PR | 85.53 ± 6.03 | 83.43 ± 4.79 | 0.011* |
| SBP | 132.32 ± 13.21 | 132.57 ± 10.62 | 0.890 |
| DBP | 84.46 ± 8.51 | 84.57 ± 6.72 | 0.926 |
| Duration of symptoms | 6.62 ± 2.31 | 4.51 ± 1.71 | 0.0001* |
| Steroid + heparin | 79 | 40 | 0.0001* |
| Steroid only | 4 | 65 | 0.0001* |
| NIV | 69 | 5 | 0.0001* |
| Oxygen | 6 | 39 | 0.0001* |
| Mechanical ventilation | 11 | 0 | 0.0001* |
| Duration of hospital stay | 7.11 ± 2.86 | 15.93 ± 6.45 | |
| Inotropes | 1 | 1 | 0.491 |
| Viral clearance | Not applicable | 135 (96.4%) | |
| Days for viral clearance | Not applicable | 24.81 ± 5.61 | - |
| ICU | 84 | 33 | 0.0001* |
| qSOFA | |||
| 0 | 0 | 95 | 0.0001* |
| 1 | 48 | 43 | |
| 2 | 24 | 2 | |
| 3 | 14 | 0 | |
COVID = coronavirus disease, DBP = diastolic blood pressure, DM = diabetes mellitus, HTN = hypertension, ICU = intensive care unit, MHD = maintenance hemodialysis, SBP = systolic blood pressure, CAD = coronary artery disease, AVF = arteriovenous fistula, CVD = coronary vascular disease, IJV = internal jugular vein, qSOFA: Quick Sequential Organ Failure Assessment, SOB = shortness of breath, PR = pulse rate, Significance of * is p < 0.05
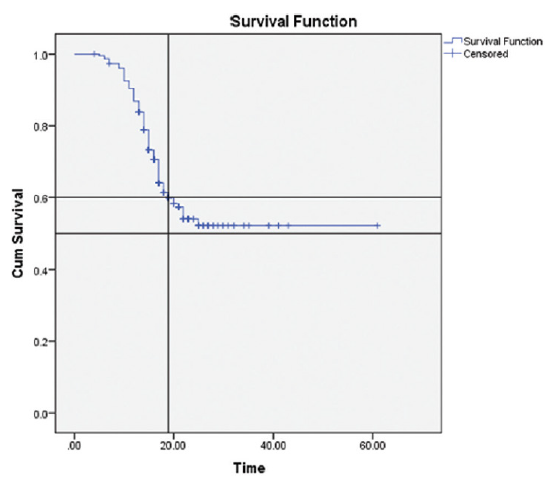
- Survival analysis curve of the MHD group. MHD = maintenance hemodialysis.
Discussion
Patients on MHD are vulnerable for infections due to underlying uremia-induced dysregulated immune mechanisms. Changes in innate immunity along with variability in the functions of natural killer (NK) cells, T lymphocytes, B lymphocytes, and persistent dialysis-induced inflammatory status predispose these patients to various bacterial and viral infections, in which SARS-CoV-2 is no exception.1,2 Hence, in the background of ongoing COVID pandemic, MHD patients are expected to have grave outcomes not only due to compromised immune status, but also due to the logistics of traveling to the center twice or thrice weekly, inability to maintain social distancing, and repeated exposure to health-care setting.3
A number of studies reported a high morbidity and mortality in this group compared to the general population. Yiqiong Ma et al. compared 37 MHD patients with healthy subjects and concluded that the MHD group had a higher mortality (6/37).4 In a study of 36 Spanish MHD patients by Goicoechea et al., a high mortality rate was observed.5 Variable mortality has been reported from the early days of pandemic, ranging widely between 13% and 42%.4,6-8
Our study data is from a unique model of MHD, that is, hub and spoke model. In this model, three government teaching hospitals with faculty are labeled as hub centers and the remaining district centers and community health dialysis centers are considered as spoke centers. A total of 2248 patients are dialysis beneficiaries under cashless government-funded scheme. In a state of 3 crore population with 46 centers of government-run hemodialysis centers and a good number of private hemodialysis centers, all the patients with RT-PCR positivity were referred to us.
During the pandemic period of April 2020–December 2020, MHD patients accounted for 1.06% of all admissions. Mean age of the group was 50 years, and males formed more than two-thirds of the referred MHD group. Prevalence of COVID in the general population was between 0.2% and 0.7%, and in the MHD group, it was approximately 2.26%. Our group may not represent the total prevalence as only sicker patients were referred to us for admission. Even though our hospital was a referral hospital, the numbers may not truly reflect the MHD group affected with COVID. Milder infections and asymptomatic infections in the MHD group were not identified in all the centers due to logistics in resource-poor settings.
Mortality was 38% in our group, which is higher compared to that reported in other studies. The European Renal Association-European Dialysis and Transplantation Association (ERA-EDTA) registry of COVID-positive Kidney Replacement Therapy (KRT) patients from seven countries reported a mortality rate of 20%–21%, which is higher compared to KRT patients without COVID infection.9 In a study of a French dialysis cohort, Renal Epidemiology Information Network (REIN) registry, the mortality rate in COVID-positive MHD patients was 20%10 and the factors associated with high mortality rate were found to be higher age, hypoalbuminemia, and presence of ischemic heart disease. In another study by Ng et al.,11 in 419 MHD patients, the mortality was reported to be 32%–37% and the authors identified age, lymphopenia, mechanical ventilation, high blood urea nitrogen, and high ferritin levels to be associated with mortality. A higher mortality of 52% was reported in an early study of 23 COVID-positive MHD patients from China.12
In our study, we found age, presence of diabetes, delayed presentation to hospital, breathlessness at admission, thrombocytopenia, high creatinine levels, hypoxemia, metabolic acidosis, hypoalbuminemia, need for ventilation support systems, and higher qSOFA to be associated with mortality [Tables 2 and 3]. On assessment of the survival analysis curve, it was observed that the probability of survival till 19 days was 60%.
| MHD patients with COVID infection (n = 226) | P | ||
|---|---|---|---|
| Death (n = 86) | Discharged (n = 140) | ||
| Hemoglobin | 8.59 ± 0.79 | 8.81 ± 0.66 | 0.055 |
| TLC | 8941.81 ± 4880.03 | 7344.85 ± 2481.62 | 0.024* |
| Platelets | 0.97 ± 0.28 | 1.42 ± 0.38 | 0.0001* |
| Blood urea | 92.35 ± 25.06 | 86.14 ± 21.31 | 0.082 |
| Blood creatinine | 11.50 ± 2.57 | 9.84 ± 2.09 | 0.0001* |
| pH | 7.30 ± 0.04 | 7.33 ± 0.04 | 0.0001* |
| pO2 | 71.27 ± 4.33 | 85.90 ± 6.68 | 0.0001* |
| pCO2 | 22.30 ± 4.36 | 23.97 ± 2.40 | 0.001* |
| HCO3 | 11.81 ± 2.12 | 14.20 ± 2.42 | 0.0001* |
| Serum potassium | 4.73 ± 0.57 | 4.43 ± 0.64 | 0.002* |
| Total protein | 6.06 ± 0.16 | 6.12 ± 0.20 | 0.057 |
| Serum albumin | 2.86 ± 0.15 | 2.94 ± 0.14 | 0.002* |
| Total bilirubin | 0.93 ± 0.31 | 0.88 ± 0.20 | 0.174 |
| Direct bilirubin | 0.23 ± 0.23 | 0.21 ± 0.17 | 0.342 |
| SGOT | 25.00 ± 11.11 | 22.77 ± 4.78 | 0.152 |
| SGPT | 25.92 ± 13.04 | 23.92 ± 5.4 | 0.287 |
| PT INR | 1.11 ± 0.13 | 1.06 ± 0.19 | 0.080 |
| APTT | 30.46 ± 1.57 | 29.38 ± 4.62 | 0.089 |
COVID = coronavirus disease, MHD = maintenance hemodialysis, SGOT = serum glutamate oxaloacetate transaminase, SGPT = serum glutamate pyruvate transaminase, TLC = total leukocyte count, APTT = activated partial thromboplastin time, PT = prothrombin time, INR = international normalised ratio. Significance of * is p < 0.05
Viral clearance of SARS-CoV-2 in majority of the patients was observed at the fourth week, though the clearance started by the third week, unlike the general population in whom viral clearance is achieved by the 10th day of illness. All patients who had viral shedding were asymptomatic, but were continued in hospital due to positive RT-PCR test. But it is not known whether the shed virus is a dead virus/inactive virus without replicative capacity or a live replication virus. In a study by Shaikh et al., it was observed that 32% continued to test positive even after 40 days of infection.13 It is yet to be understood why there was a prolonged viral shedding in asymptomatic dialysis patients who have altered immune responses.14
Conclusion
Prevalence of COVID-positive MHD patients with severe infection was 1.06% of all COVID admissions and accounted for 53% of total nephrology referrals. Mortality was 38% in our study group, and the risk factors of mortality in MHD group are older age, presence of diabetes, higher qSOFA score, and hypoxemia.
Conflicts of interest
There are no conflicts of interest.
References
- Clinical characteristics of and medical interventions for COVID-19 in hemodialysis patients in Wuhan, China. J Am Soc Nephrol.. 2020;31(7):1387-97.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Infectious disease risk in dialysis patients: A transdisciplinary approach. Can J Kidney Health Dis.. 2019;6:2054358119839080.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Epidemiology of COVID-19 in an urban dialysis center. J Am Soc Nephrol.. 2020;31(8):1815-23.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- 2019 novel coronavirus disease in hemodialysis (HD) patients: Report from one HD center in Wuhan, China. medRxiv doi: 10.1101/2020.02.24.20027201
- [Google Scholar]
- COVID-19: Clinical course and outcomes of 36 maintenance hemodialysis patients from a single center in Spain. Kidney Int.. 2020;98(1):27-34.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- An analysis on the clinical features of MHD patients with coronavirus disease 2019: A single center study. Available from 10.21203/rs.3.rs-18043/v1https://www.researchsquare.com/article/rs-18043/v1 [Last accessed 2021 July 3]
- [Google Scholar]
- Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int.. 2020;97(5):829-38.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A report from the Brescia Renal COVID Task Force on the clinical characteristics and short-term outcome of hemodialysis patients with SARS-CoV-2 infection. Kidney Int.. 2020;98(1):20-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Results from the ERA-EDTA Registry indicate a high mortality due to COVID-19 in dialysis patients and kidney transplant recipients across Europe. Kidney Int. 2020;98(6):1540-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Low incidence of SARS-CoV-2, risk factors of mortality and the course of illness in the French national cohort of dialysis patients. Kidney Int.. 2020;98(6):1519-29.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Outcomes of patients with end-stage kidney disease hospitalized with COVID-19. Kidney Int.. 2020;98(6):1530-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- COVID-19 outbreak in a large hemodialysis centre in Lombardy, Italy. Kidney Int Rep.. 2020;5(7):1095-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prolonged SARS CoV-2 viral shedding and IgG antibody response to SARSCoV-2 in patients on hemodialysis. Clin J Am Soc Nephrol.. 2021;16(2):290-2.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Virological assessment of hospitalised patients with COVID 2019. Nature. 2020;581:465-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







