Translate this page into:
Comparison of Dialysis Catheter Insertion and Complications Under Ultrasound Guidance with or without Fluoroscopic Assistance: A Randomized Study
*Dr. Sushma Konnepati and Dr. Jasmine Sethi both serve as joint first authors.
Corresponding author: Manish Rathi, Department of Nephrology, Post Graduate Institute of Medical Education and Research, Chandigarh, India. E-mail: drmanishrathi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Konnepati S, Sethi J, Lal A, Ramachandran R, Rathi M. Comparison of Dialysis Catheter Insertion and Complications Under Ultrasound Guidance with or without Fluoroscopic Assistance: A Randomized Study. Indian J Nephrol. 2024;34:363-8. doi: 10.25259/ijn_414_23
Abstract
Background:
Fluoroscopy is considered to be the gold standard and an essential requirement for catheter insertion. However, there is a paucity of data regarding the outcomes in ultrasound (USG)-guided insertion with and without fluoroscopy. We compared the complications of USG-guided tunneled dialysis catheter (TDC) insertion with and without fluoroscopy assistance.
Materials and Methods:
This was a single-center randomized controlled trial (RCT) done in a tertiary hospital in North India. After screening 153 patients, 149 were enrolled: 87 were randomized into USG-guided insertion without fluoroscopy (group A) and 62 were randomized into USG-guided insertion with fluoroscopy (group B). All insertions were done in a dedicated procedure room by trained nephrologists. Outcomes were analyzed at baseline and at 1-month follow-up. Mechanical complications as well as infective and thrombotic complications were compared between both the groups.
Results:
TDC insertion was successful (100%) in all the study participants (N = 149). One hundred twenty-nine catheters (86.5%) were inserted in the first attempt, 19 (12.5%) in the second attempt, and one catheter insertion required three attempts for insertion. The mean age of study participants was 43 years (±16.5), and males constituted 63% of the study cohort. Baseline laboratory characteristics of the two groups were comparable. The mean time of catheter insertion was 41.26 min (standard deviation [SD] 11.8) in group A and 47.74 min (SD 17.2) in group B (P = 0.007). The mean score of ease of catheter insertion, exit site bleed, infective and mechanical complications were not different between the two groups.
Conclusion:
Our study concluded that fluoroscopy has no additional advantage in reducing mechanical, infective, or thrombotic complications. In experienced hands, USG-guided TDC insertion without fluoroscopy assistance is as good as the insertion done with fluoroscopy assistance, with a shorter procedure time.
Keywords
Complications
Ease of catheter insertion
Fluoroscopy
Insertion
Procedure time
Tunneled dialysis catheter
Introduction
Kidney replacement therapy, like hemodialysis, is lifesaving and decreases the mortality of patients affected with end-stage kidney disease (ESKD). To date, arteriovenous fistula (AVF) remains the gold standard among the available options for vascular access due to the lowest risk of complications and best long-term patency. However, central venous catheters (CVCs) are commonly being used when AVF cannot be placed due to various reasons. The National Kidney Foundation Kidney Disease Outcomes Quality Initiative (NKF-KDOQI) guidelines have recommended that when a catheter will be needed for more than 3 weeks, a tunneled dialysis catheter (TDC) should be used.1
TDCs are made of silicone or silastic elastomers and are more pliable than temporary catheters. They provide bigger lumens and a better blood flow for hemodialysis. Hence, TDCs are preferred over the nontunneled catheters when long-term vascular access is needed.1 It is undeniable that image-guided CVC insertion has fewer mechanical and infective complications and is better than the traditional landmark method, as emphasized by previous studies.2-4 Most of the previous studies have compared the outcomes of ultrasound (USG)-guided TDC insertions; only a few have assessed outcomes using fluoroscopy and emphasized that fluoroscopy-guided insertion is better than blind insertion.5 To the best of our knowledge, only a few have compared TDC insertion with and without fluoroscopy.6,7 The majority of data of bedside TDC insertion without fluoroscopic assistance came during the coronavirus disease 2019 (COVID-19) era, when retrospective analysis of cases had shown bedside catheter insertion to be safe.8 The present study was done to compare the complications of USG-guided TDC insertion with and without fluoroscopy assistance. To the best of our knowledge, this is the first prospective, randomized study comparing the outcomes of TDC insertions with and without fluoroscopy.
Materials and Methods
This was a single-center, prospective, randomized controlled study conducted at a tertiary care center in northern India. Consecutive patients (age > 12 years) planned for TDC insertion in the right-side internal jugular vein (IJV) and willing to give consent were included. Patients who had contraindications to fluoroscopy, such as pregnant/lactating mothers were excluded. Those with local infection over the insertion site, coagulopathy, thrombocytopenia, ipsilateral hemothorax/pneumothorax, target vein thrombosis/stenosis, catheter exchange over guide wire, and history of previous TDC catheter insertion in the right IJV were also excluded. The study was approved by the Institute Ethics Committee and was registered with Clinical Trial Registry – India (CTRI/2021/09/036204). The study was approved by the Institutional Review Board at Post Graduate Institute of Medical Education and Research, number INT/IEC/2021/SPL-1268, dated 24/08/2021. An informed consent was obtained from all study participants or their parents/legal guardians in accordance with the Declaration of Helsinki, and the procedures followed were in accordance with the ethical standards of the responsible committees on human experimentation (institutional and national) and with the Declaration of Helsinki Principles 1975, as revised in 2000. All the patients in the study received standard of care. The study was conducted without any delay in the management of the patient.
The sample size was calculated based on the complication rates of USG-guided insertion without fluoroscopy (group A) and USG-guided insertion with fluoroscopy (group B), assuming that the expected percentage of no complications is 85% in group A and 95% in group B. On a superiority basis, to achieve this difference with the power of study at 80% and a significance level of 5%, it was estimated that 70 subjects were required per group.
Study conduct
Patient demographics, comorbidities, site of TDC insertion, preprocedure use of antiplatelet or anticoagulation agent, and laboratory results were obtained from the hospital records. Patients were followed up from the period of catheter insertion up to 1 month postinsertion. The primary outcome was successful placement of catheter tip in the right atrium. The secondary outcomes included procedure time, number of attempts, ease of catheter insertion by the nephrologist, catheter-associated complications (bleeding, kinking, malposition, catheter-related bloodstream infection [CRBSI]), catheter dysfunction requiring further intervention, and catheter patency.
Study definitions
An attempt was considered successful if the catheter tip was successfully positioned in the mid-right atrium with a maximum of three attempts. Unsuccessful placement: An attempt was considered unsuccessful when there was no return of venous blood from the targeted vein after skin puncture. After three unsuccessful attempts, the procedure was declared unsuccessful. The procedure time was defined as the time that lapsed between the initial administration of local anesthesia and completion of suturing at the end that was required in catheter insertion procedure. Data on ease of insertion was collected by interviewing the nephrologists, and they were asked to grade the ease of insertion on a scale from 1 to 10 (1 being difficult and 10 being most easy). Catheter dysfunction was defined as failure to maintain the required blood flow for adequate hemodialysis without prolonging the treatment duration. The complications observed in this study were classified according to the reporting standards of the Society for Interventional Radiology.1
Statistical analysis
Analyses were performed using Statistical Package for the Social Sciences (SPSS) 25.0, with statistical significance set at P < 0.05. Descriptive statistics were presented as mean (standard deviation [SD]) for numerical variables and percentage for categorical data. Two-sample t-tests were performed to compare the numerical variables between the two groups when normality and homogeneity assumptions were satisfied; otherwise, Mann–Whitney U was used. Chi-square or Fisher’s exact was used to compare categorical variables, adjusted using logistic regression with odds ratios (OR) and 95% confidence interval (CI) presented.
Technique of TDC insertion without fluoroscopy (group A)
All our TDC insertions were performed under USG guidance in a dedicated procedure room located inside our dialysis unit. TDC insertion was done by a nephrology trainee who had previously done at least 50 successful independent catheter insertions. Patients had real-time monitoring of the blood pressure, pulse rate, and oxygen saturation throughout the procedure. The catheter tip position was positioned to be in the mid-right atrium and was inserted using the anatomic landmarks. The manubrial–sternal angle was taken as the topographical landmark that corresponded to the carina, and the insertion depth was estimated by measuring the distance between the skin venipuncture site, that is, 1–2 cm above the clavicle, and a point 5 cm below the manubrial–sternal angle. The catheter length was determined by adding the insertion depth to the tunnel length. Firstly, the right IJV was cannulated with the introducer needle under USG guidance and the guidewire was threaded into the vein. If there was any resistance, the wire was repositioned or adjusted and/or a new cannulation was attempted. Once the wire was in place, the catheter was tunneled subcutaneously and then introduced into the vein via the peel-away sheath. All the patients received a symmetrical tip catheter. All patients underwent a postprocedural chest radiogram to confirm the tip position in the mid-right atrium and to ensure that there were no kinks before use of the catheter for dialysis.
Technique of TDC insertion with fluoroscopic assistance (group B)
Technique of catheter insertion was similar, but the procedure was done with fluoroscopy in a dedicated fluoroscopy suite located in our dialysis unit. Real-time visualization of the guidewire and catheter was achieved. The tip of the catheter was confirmed to be in the mid-right atrium under fluoroscopic guidance.
Results
A total of 149 subjects were randomized into two groups by computed-generated random table number [Figure 1]. Eighty-seven TDC insertions were done under USG guidance without fluoroscopy (group A), and 62 insertions were done with USG guidance and fluoroscopy assistance (group B). TDC insertion was successful in all the study participants (100%), and the immediate catheter flow achieved was adequate in all subjects. One hundred twenty-nine catheters (86.5%) were inserted in the first attempt, 19 (12.5%) in the second attempt, and one catheter insertion required three attempts for insertion. The mean age of study participants was 43 years (±16.5), and males constituted 63% of the study cohort. The basic disease was not known in 89 (59.7%) participants, and presumed diabetic kidney disease (DKD) constituted 29.5% of the cohort. Nine patients (6%) had a previous AVF failure, and 48 patients (32%) had a previous nontunneled catheter. The remaining patients were starting dialysis with TDC as their first access. Baseline laboratory characteristics of the two groups were comparable with no significant difference [Table 1].
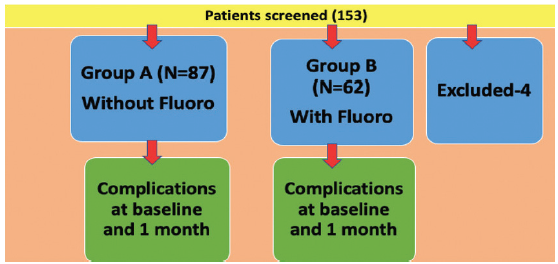
- Study design and patient enrollment.
| Variable | Group A (without fluoroscopy) | Group B (with fluoroscopy) | P |
|---|---|---|---|
| Males, n (%) | 52 (59.8%) | 42 (68%) | 0.32 |
| Age, mean (SD) | 44 years (SD 16.8) | 42.8 years (SD 16) | 0.52 |
| Diabetics | 25 (28.7%) | 19 (30.6%) | 0.80 |
| Hypertension | 63 (72.4%) | 46 (73.2%) | 0.80 |
| Cardiac disease | 4 (4.6%) | 6 (9.7%) | 0.32 |
| Previous fistula failure | 6 (6.9%) | 3 (4.8%) | 0.73 |
| Previous nontunneled catheter | 26 (29.9%) | 22 (45.8%) | 0.47 |
| Laboratory parameters (median±IQR) | |||
| Hemoglobin (g/dl) | 8.00 (5–11) | 8.15 (5.2–12.4) | 0.228 |
| Platelet counts (cells/mm3) | 194,000 (65,000–520,000) | 195,000 (38,000–608,000) | 0.754 |
| PTI (%) | 90 (66–100) | 88 (60–100) | 0.209 |
| INR (ratio) | 1 (0.96–1.37) | 1 (0.86–1.39) | 0.091 |
IQR: interquartile range; SD: standard deviation; INR: International normalized ratio; PTI: Prothrombin time index.
In group A, 76 catheters (87.3%) were inserted in the first attempt and 11 (12.6%) in the second attempt. In group B, 53 (85.4%) catheters were inserted in the first attempt, eight (12.9%) in the second attempt, and one catheter insertion required three attempts (P = 0.47). The procedure time was shorter in group A with a mean time of catheter insertion of 41.26 min (SD 11.8) compared to 47.74 min (SD 17.2) in group B (P = 0.007). The mean score of ease of catheter insertion was not different between the two groups. Out of 149 study participants, 13 (8.7%) participants developed exit site/tunnel bleed immediately after catheter insertion, of which nine were from group A (10.5%) and four were from group B (6.5%) (P = 0.40). However, all were minor bleeding episodes and resolved with compression banding or placement of sutures. In all 13 patients with exit site/tunnel bleed, catheters were salvaged, and no further complications were noted [Table 2].
| Variable | Group A (without fluoroscopy) | Group B (with fluoroscopy) | P |
|---|---|---|---|
| Successful insertion | 87 (100%) | 62 (100%) | |
| Number of attempts | 0.47 | ||
| 1 | 76 (87.3%) | 53 (85.4%) | |
| 2 | 11 (12.6%) | 8 (12.9%) | |
| 3 | 0 | 1 | |
| Ease of procedure | 7.62 (SD 0.82) | 7.58 (SD 0.65) | 0.60 |
| Hematoma formation | 9 (10.3%) | 4 (6.5%) | 0.40 |
| Procedure time (min) (Mean±SD) | 41.26 min (SD 11.8) | 47.74 min (SD 17.2) | 0.007 |
| Catheter dysfunction | 1 (1.1%) | 0 |
SD: standard deviation.
Catheter dysfunction: One patient had catheter malposition on postinsertion chest radiograph, with inadequate blood flow rate in dialysis (from group A), and successful catheter repositioning was done under fluoroscopic guidance. One patient from group B had catheter kinking, for which a successful repositioning was done. No episodes of fibrin sheath, thrombus formation or tip occlusion were encountered in any patient [Table 3].
| Variable | Group A (without fluoroscopy) | Group B (with fluoroscopy) | Total | P |
|---|---|---|---|---|
| CRBSI | 11 (12.6%) | 3 (4.8%) | 14 (9.4%) | 0.108 |
| Slippage | 5 (5.7%) | 0 (0%) | 5 (3.4%) | 0.081 |
| Malposition | 1 (1.1%) | 0 (0%) | 1 (0.7%) | 1.000 |
| Kinking | 0 (0%) | 1 (1.6%) | 1 (0.7%) | 0.416 |
| Total | 17 (19.5%) | 4 (6.4%) | 21 (14.1%) | 0.225 |
CRBSI: catheter-related bloodstream infection.
Outcome analysis at 1 month
At 1-month follow-up, overall, CRBSI was the single most complication noted in 14 study participants, contributing to 9.4% (11 patients from group A and three from group B, P = 0.10). In group A, two patients had CRBSI due to Klebsiella pneumonia, two patients had Enterobacter species, two patients had Escherichia coli, one patient had Pseudomonas aeruginosa, and four patients had culture-sterile CRBSI. In group B, all three patients had E. coli sepsis. Spontaneous catheter slippage was seen in five participants (3.6%), and all of them were from group A (P = 0.08).
Discussion
Our study is one of the first randomized trials that has compared mechanical and infective complications of USG-guided TDC insertion done with or without fluoroscopy. In the previous study from our center, nonimaging-guided insertion of nontunneled catheters had more complications when compared to USG-guided insertion.9 However, till date, few studies have compared USG-guided insertions with and without fluoroscopy.6,7 In our study, we found that TDC insertions were safe and outcomes were similar even in nonfluoroscopy group.
These results are consistent with those of previous studies. Earlier, Chang et al.6 had shown that TDC insertion in the right IJV without fluoroscopy was safe and had comparable outcomes to fluoroscopy-guided insertion. However, this study included both new insertions and exchanges over guidewire. Similarly, Yevzlin et al.7 compared the clinical outcomes and cost analysis of TDC and concluded that there were no differences in bleeding complications between the blind and fluoro-guided groups. Cost analysis revealed substantial reduction in total bills in the nonfluoroscopic technique, and it was more cost-effective. Sohail et al.,8 in a retrospective review of 25 patients, showed that bedside right internal jugular TDC placement in coronavirus disease 2019 (COVID-19) patients using USG and anatomic landmarks without fluoroscopic guidance is safe and effective and can potentially avoid the need of patient transfer to fluoro suite. However, all the studies mentioned were retrospective in nature and no follow-up data was available. Moreover, there could be inherent bias since they included patients with both right- and left-side catheter insertions and even patients with history of previous TDC insertions. Our study tried to eliminate this bias by including only right IJV insertions, that too in TDC-naïve patients.
The primary outcome of our study was the successful position of TDC tip in the right atrium, which was 100% in both groups. The parameters like the number of attempts for successful catheter placement, mean procedure time, and the subjective ease of catheter insertion were compared between both the groups, which is unique, and we believe this was a distinct contribution to the evidence needed to guide clinical practice. We found that fluoroscopy-guided TDC insertion took more time than the nonfluoro group. Fluoroscopy use is technically more time-consuming, which is attributed to the time taken to align the participant in the correct position for better imaging. Moreover, it requires a technical expertise to operate. Apart from the procedure time, other factors like operator’s ease of insertion, exit site bleeding, catheter slippage/malfunction, and CRBSI were not different between the two groups.
Exit site/tunnel bleed was found in 13 (8.7%) patients, which was not statistically significant between the groups. Our results are consistent with a South Indian study by Sampathkumar et al.,10 where they showed 8% of patients had exit site bleeding. The bleed may be due to the procedure itself as well as due to the uremic milieu of these patients. However, all the bleeds were minor and managed with compression/suturing and did not require removal of catheter.
Catheter-related infection was the commonest late complication reported in 14 participants (9.4%), and gram-negative infections constituted the majority (100% of culture-positive cases). The CRBSI rates reported in literature in patients with TDCs range from 10.1% to 13%, but the results are mostly from retrospective patient series.11–13 One of the reason for high incidence of CRBSI is that these patients were receiving their maintenance dialysis at a peripheral dialysis center post-TDC insertion. There is no maintenance dialysis facility at our institute, and hence, these patients were having dialysis performed from outside our hospital at a peripheral dialysis center, where the catheter care and protocols could be variable and not the most appropriate, resulting in high infection rate. Whereas a study from our center on TDC showed higher incidence of gram-negative infections than gram-positive infections.14 Hence, a higher incidence of gram-negative infection should be taken into account, and empirical gram-negative antibiotic should also be started along with gram-positive coverage for suspected CRBSI to salvage TDC. In our study, all the patients who developed CRBSI required catheter removal due to persistent fever even after they received appropriate antibiotics.
The third common complication noted in our study was catheter slippage, all from group A that were spontaneous, and the catheters were removed subsequently. However, there was no difference between the two groups. A total of 25 catheters (16.7%) were removed for various reasons at 1 month (18 in group A and seven in group B). In group A, nine (10.3%) catheters were removed due to CRBSI, four (4.49%) due to fistula maturation, and five (5.7%) due to catheter slippage. In group B, three (4.8%) catheters were removed due to CRBSI and four (6.45%) due to fistula maturation. CRBSI was the most common cause that resulted in catheter removal. Delayed complications like central venous stenosis were not studied in our study. However, we followed our participants only for 1 month, and it is too short a time for a patient to develop central venous stenosis.
The strength of our study includes its randomized, prospective design. We tried to eliminate the potential confounding factors like variations in the site of insertion and recurrent TDC insertions. Parameters like the ease of catheter insertion and procedure time were compared between the groups, which are unique and major strengths of our study. Our study findings are valuable as the availability of fluoroscopy may not be sufficient to meet the great demand for TDC exchanges or insertions in peripheral resource-constrained settings. In the current circumstances, such as the COVID-19 pandemic where resources are stretched, there is emphasis on striving for efficient, safe, and least resource-intensive processes. Hence, our study supports the practice of performing the USG-guided procedure without fluoroscopy, especially in institutions where fluoroscopy facilities are not readily available. However, the person performing the procedure should be a trained one, and all the catheter insertions in our study were done by trained nephrologists. Radiation exposure to the participant as well as the staff is another limitation of fluoroscopy-guided technique, which we have not taken into account. Another aspect which was not studied here is the financial implications of use of fluoroscopy for this procedure. Ours was a government-funded hospital, and we did not charge any extra money for use of this facility; however, the practice may be different in private or corporate hospitals.
This is a single-center study with relatively small sample size and a relatively short follow-up period of 1 month. So, the results of the study cannot be generalized, which is a major limitation of our study. The ease of catheter insertion and the procedure time are subjective and depend on the interventionist, and more objective methods of assessment need to be employed. Cost analysis was not assessed in our study, which is an important limitation. Moreover, we excluded patients with history of central vein stenosis, and left-sided insertions were not included; therefore, generalizing the results would be difficult.
Conclusion
The technique of inserting TDC in the right IJV without fluoroscopy performed by trained intervention nephrologists is a safe and effective method in patients with no previous history of central vein stenosis.
Conflicts of interest
There are no conflicts of interest.
References
- KDOQI clinical practice guideline for vascular access: 2019 Update. Am J Kidney Dis. 2020;75(4 Suppl 2):S1-S164.
- [CrossRef] [PubMed] [Google Scholar]
- Real-time ultrasound-guided catheterisation of the internal jugular vein: A prospective comparison with the landmark technique in critical care patients. Crit Care. 2006;10:R162.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Ultrasound guidance versus anatomical landmarks for internal jugular vein catheterization. Cochrane Database Syst Rev. 2015;1:CD006962.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A prospective randomized study to compare ultrasound-guided with nonultrasound-guided double lumen internal jugular catheter insertion as a temporary hemodialysis access. Ren Fail. 2005;27:561-4.
- [CrossRef] [PubMed] [Google Scholar]
- Combined ultrasound and fluoroscopy guided port catheter implantation--high success and low complication rate. Eur J Radiol. 2009;69:517-22.
- [CrossRef] [PubMed] [Google Scholar]
- Comparing outcomes of tunnelled dialysis catheter insertions and exchanges with or without fluoroscopy. J Vasc Access. 2022;23:443-9.
- [CrossRef] [PubMed] [Google Scholar]
- Fluoroscopically guided vs modified traditional placement of tunneled hemodialysis catheters: Clinical outcomes and cost analysis. J Vasc Access. 2007;8:245-51.
- [PubMed] [Google Scholar]
- Safety of bedside placement of tunneled hemodialysis catheters in the intensive care unit: Translating from the COVID-19 experience. J Clin Med. 2021;10:5766.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Non-imaging assisted insertion of un-cuffed, non-tunneled internal jugular venous catheters for hemodialysis: Safety and utility in modern day world. Biomed J. 2016;39:283-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Vascular access creation and care—Perspective from India. Adv Chronic Kidney Dis. 2015;22:466-70.
- [CrossRef] [PubMed] [Google Scholar]
- Time to revisit the use of nontunneled dialysis vascular catheters even in cost-limited setting. Indian J Nephrol. 2018;28:406-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Complications associated with permanent internal jugular hemodialysis catheter: A retrospective study. Cureus. 2019;11:e4521.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Outcomes of tunneled internal jugular venous catheters for chronic haemodialysis at the University College Hospital, Ibadan, Nigeria. Pan Afr Med J. 2018;31:218.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Hemodialysis tunneled catheter-related infection in a tertiary care center: A changing trend. Saudi J Kidney Dis Transpl. 2019;30:1187-9.
- [CrossRef] [PubMed] [Google Scholar]







