Translate this page into:
Tunneled Dialysis Catheter Insertion in External Jugular Vein by Nephrologists
Corresponding author: Vineet Behera, Department of Nephrology, INHS Asvini, Mumbai, Maharashtra, India, E-mail: beheravineet@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Behera V, Ahmad S, Sinha S, Reddy G G, Srikanth K, Ghosh I, et al. Tunneled Dialysis Catheters Insertion in External Jugular Vein by Nephrologists. Indian J Nephrol. doi: 10.25259/ijn_511_23
Abstract
Background
External jugular vein (EJV) is used to insert tunneled dialysis catheter (TDC) in patients with no AVF and exhausted right internal jugular veins (IJV). There is scarce data on TDC insertion in EJV by nephrologists with fluoroscopy guidance.
Materials and Methods
This was a prospective observational study that included hemodialysis patients with exhausted right IJV access who underwent EJV TDC insertion, and excluded occluded ipsilateral brachiocephalic vein or superior vena cava, EJV < 5 mm diameter, or patients with existing EJV TDC. All patients underwent evaluation of central veins. TDC insertions were performed by a nephrologist using ultrasound and fluoroscopic guidance. The primary outcome was the successful insertion of EJV TDC and catheter removal within 6 months due to major catheter dysfunction or complications.
Results
EJV TDC was successfully inserted in 23/23 cases (100% success), of which 17 (73.9%) were in right side, and 21 (91.3%) were denovo insertions. Catheter dysfunction needing removal occurred in seven cases (30.4%) with subclavian vein thrombosis in five cases (21.7%) and infectious complications in two cases (8.6%). The censored catheter survival was 23/23 (100%) at 1 month, 22/23 (95.6%) at 3 months, and 13/20 (65%) at 6 months. Cases of EJV catheter removal had a significant association with drainage of EJV into subclavian vein as compared to other anatomical variants (p = 0.005).
Conclusion
EJV TDC insertion has a good technical success rate when performed under fluoroscopy. It is associated with an acceptable rate of catheter dysfunction, especially thrombosis, which is more common in EJV opening into subclavian veins.
Keywords
Hemodialysis
Tunneled dialysis catheters
External jugular vein
Subclavian vein
Thrombosis
Introduction
Vascular access is the lifeline as well as the Achilles heel for end-stage renal dialysis (ESRD) patients on hemodialysis (HD).1 AV fistula (AVF) remains the gold standard vascular access in patients with HD.2 Despite advances in the understanding of AVF creation and maturation, many patients still land on dialysis without any AVF. HD catheters come to the rescue in this scenario, acting as a bridge to AVF use. Catheters especially tunneled dialysis catheters (TDC) are increasingly being used in patients with failed AVF or with unfavorable anatomy for AVF creation.3
The veins commonly used for TDC include internal jugular veins (IJV) or femoral veins followed by other veins like external jugular veins (EJV), subclavian veins, and translumbar or transhepatic inferior vena cava (IVC).4 The KDIGO guidelines accord high importance to EJV and recommend the use of EJV before using veins like the femoral vein or the subclavian vein.5
The EJV is a superficial vein located in the neck, formed by the joining of the posterior division of the retromandibular vein with the posterior auricular vein.6 EJV is preferred for venous access, as it is superficial, easily approachable, and dilated due to its attachment with the investing layer of deep cervical fascia, which prevents it from collapsing. There is wide variation in termination of the EJV, and it may open into the subclavian vein (36%), into the IJV (4%), or the confluence of subclavian and IJV (60%),7,8 as depicted in Figure 1.
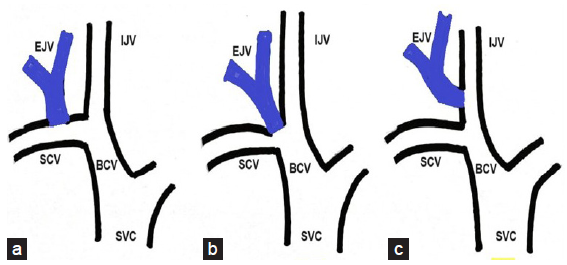
- Variations in the drainage of external jugular vein This depiction of right-sided external jugular vein shows the variations with regards to its opening into proximal veins. It may open into (a) sublavian vein, into (b) the confluence of subclavian vein and internal jugular vein, or (c) directly into the internal jugular vein. (IJV: Internal jugular vein; EJV: External jugular vein; SCV: Subclavian vein; BCV: Brachiocephalic vein; SVC: Superior vena cava)
The attempt to use EJV for TDC was done by Forauer et al. in 1999,9 and subsequently, small case series10 or case reports11 have been published where the EJV TDC insertion was done by an interventional radiologist,12 by a vascular surgeon,13 or without the use of fluoroscopy.14,15 There is scarce data of EJV TDC insertion by nephrologists using fluoroscopy and ultrasound guidance. Therefore, we designed this study to evaluate the insertion of EJV TDC by nephrologists for technical success and complications.
Materials and Methods
This was a prospective observational study conducted at three nephrology centers in India, over 2 years. The study population included all cases of ESRD in whom the EJV was considered as access for TDC.
All adult (>18 years) ESRD cases in whom EJV TDC was attempted, as a de novo insertion or TDCs exchanged over the guidewire and those with exhausted right IJV access were included.
Patients with occlusion of central veins like the ipsilateral brachiocephalic vein (BCV) (as that of EJV) or superior vena cava (SVC), those with prior EJV TDC, EJV diameter <5 mm on ultrasound despite Valsalva or other maneuvers and those unwilling to follow up were excluded.
The patient was evaluated for any thrombosis or stenosis of the central veins. The chest, face, neck, and arms were examined for dilated collateral veins and edema, ultrasound/doppler screening of central veins was done, and a CT venography was done in doubtful cases. The right-sided EJV was the preferred side while the left EJV was considered in patients with occluded right EJV or BCV.
All catheter insertions were attempted by an interventional nephrologist. Symmetric tip single cuff TDCs (Palindrome, Covidien or Glidepath, Bard), with an outer diameter of 14.5 F, were used. The decision to use EJV was based on the decision of the nephrologist.
All patients underwent baseline hematological, biochemical, and coagulation evaluation. The baseline data including details of ESRD and vascular access were recorded. The patients were reassessed for the prospect of having permanent vascular access like AVF or switching to peritoneal dialysis (PD). Written and informed consent was obtained from all patients participating in the study. Ethical approval was obtained from Institutional Ethics Committee.
Steps of EJV TDC Insertion
-
1.
The procedure was done under fluoroscopy and ultrasound guidance. Appropriate sized TDC was used (19 cm, 23 cm, or 28 cm).
-
2.
To make the EJV prominent, the patient was placed in a Trendelenburg head low position with the head turned to the contralateral side. The puncture site of EJV was planned low in the neck about 1 cm cranial to the clavicle, as shown in Figure 2.
-
3.
Local anesthesia was administered using 2% lignocaine injection. EJV was punctured using an 18 g introducer needle or a micro-puncture needle. This was followed by the insertion of a 5 F radial sheath into the vein.
-
4.
Five milliliters of diluted (1:1) nonionic contrast was injected through the sheath to define the anatomy of the venous system, the opening of EJV, or any other abnormality. In case of any thrombus or stenosis, the necessary therapeutic intervention was done, and the patient was excluded from the study.
-
5.
A J tip 0.035’ 150 cm hydrophilic glidewire was passed through the sheath, and positioned in the IVC.
-
6.
The requisite length of the tunnel and appropriate exit site were planned. A 3–5 mm incision was given lateral to the insertion site, and blunt dissection was done at the venotomy site. A 5 mm incision was given at the exit site.
-
7.
A subcutaneous tunnel of the required length was created using the stylet. Catheter was tunneled through it to keep the Dacron cuff 2 cm deep to the exit site.
-
8.
Sequential dilatation of the venotomy site was done using sequential dilators. The final trocar with a peel-away sheath was inserted into the vein. The catheter was inserted through the sheath, with the tip located in the mid-right atrium.
-
9.
The blood flow was checked and tip position was confirmed using fluoroscopy. Catheter ports were locked with 1:5000 heparin.
-
10.
The venotomy site was sutured and hemostasis was achieved, followed by dressing of the catheter and exit site.
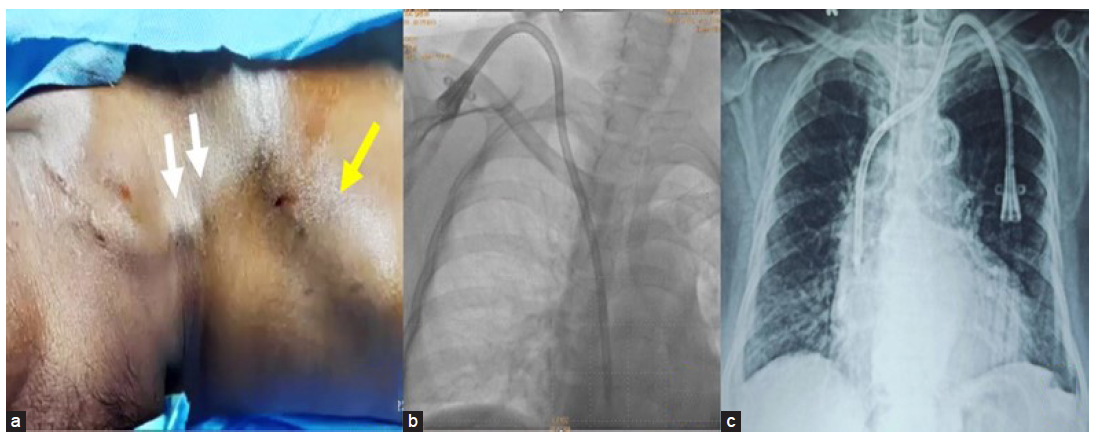
- (a) Dilated prominent external jugular vein (white arrows) draining into subclavian vein below the clavicle (yellow arrow), with the patient in a supine position. (b) Fluoroscopic image of the inserted right external jugular tunneled catheter with the catheter tip in the right atrium. (c) X-ray chest showing a left-sided external jugular vein tunneled catheter.
Outcome measures
Primary outcome measures were successful insertion of EJV TDC and catheter removal within 6 months due to major catheter dysfunction or complications. Successful insertion was defined as TDC insertion with the tip positioned in mid-right atrium and catheter blood flow >300 mL/min. Major catheter dysfunction was defined as complications that did not respond to conservative measures and needed catheter removal.
The patients were followed up for any complications, blood flow rates, new onset fever, and limb swelling. Primary catheter patency was defined as the time from catheter insertion to any catheter dysfunction needing removal at 30, 90, and 180 days. The individuals in whom a functioning EJV TDC was removed because of functional AVF, PD, or kidney transplant were excluded.
Statistical analysis
Statistical analysis of the data was carried out using SPSS version 19. Descriptive data are presented as mean ± SD or median with interquartile range for continuous variables, and frequency (%) for categorical variables. For comparison, frequency, percentage, and chi-square test were used. P value less than 0.05 was considered statistically significant.
Results
Demographic and clinical characteristics
Thirty cases of ESRD were considered between March 2021 and February 2023, of which seven were excluded as shown in Figure 3. EJV TDC was inserted in 23 individuals, amongst which 17 (73.9%) were in the right EJV, and 06 (26%) in the left side; 21 (91.3%) insertions were done de novo, while 02 (8.6%) insertions were done by exchanging the existing temporary EJV catheter over a guidewire. The baseline demographic parameters of the study population are given in Table 1.
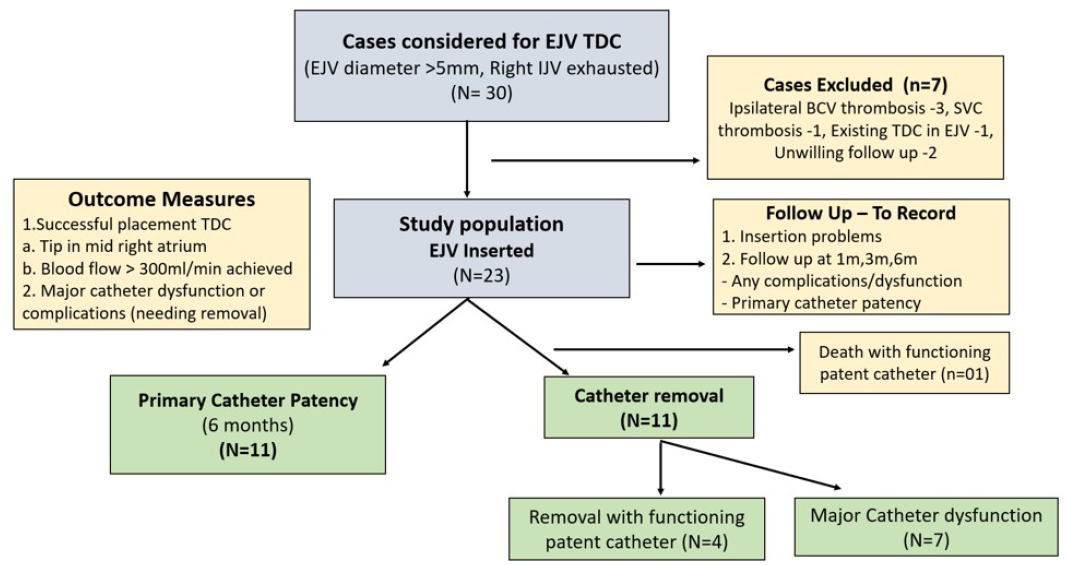
- Flow diagram of the study (EJV: External jugular vein; TDC: Tunneled dialysis catheter; BCV: Brachiocephalic vein; SVC: Superior vena cava; IJV: Internal jugular vein). N- study population considered and included in study, n- patients excluded from study
| Variable | Total (N = 23), n (% of N) |
|---|---|
| Males | 10 (43.4%) |
| Mean age (in years) | 55.7 ± 10.9 (range 38–76) |
| Diabetes mellitus | 10 (43.4%) |
| Obese (BMI ≥ 30 kg/m2) | 05 (21.7%) |
| On antiplatelet or oral anticoagulants | 05 (21.7%) |
| Dialysis vintage (in months) | 18.3 ± 16.3 |
| Native kidney disease | |
| Diabetic kidney disease | 08 (34.7%) |
| Tubulo-interstitial disease | 06 (26.0%) |
| Chronic glomerulonephritis | 05 (21.7%) |
| Polycystic kidney disease | 02 (8.6%) |
| Others | 02 (8.6%) |
| Prior dialysis access | |
| AV fistula | 04 (17.3%) |
| Tunneled dialysis catheters | 11 (47.8%) |
| Temporary dialysis catheters | 08 (34.7%) |
| Side of external jugular vein | |
| Right sided | 17 (73.9%) |
| Left sided | 06 (26%) |
| Catheter type used | |
| Palindrome | 15 (65.2%) |
| Glidepath | 08 (34.7%) |
| Exhaustion of other major central neck veins by thrombus or stenosis | |
| Right IJV | 23 (100%) |
| Left IJV | 13 (56.5%) |
| Right or left BCV | 04 (17.3%) |
| SVC | Nil |
| Opening of EJV into | |
| Confluence of IJV and subclavian vein | 15 (65.2%) |
| Subclavian vein | 07 (30.4%) |
| IJV | 01 (4.3%) |
BMI: Body mass index; IJV: Internal jugular vein; EJV: External jugular vein; BCV: Brachiocephalic vein; SVC: Superior vena cava; N: Total sample size, n: sub group sample size
All cases had exhausted right IJV, while 13 (56.5%) had exhausted left IJV, with 04 (17.3%) having contralateral BCV thrombosis. In the subgroup with right EJV TDC, 17 (100%) of right IJV, 8 (47%) of left IJV, and 3 (17.6%) of left BCV were thrombosed, and all right BCV were patent; while in patients with left EJC TDC, 6 (100%) of right IJV, 5 (83.3%) of left IJV, and 1 (16.6%) of right BCV were thrombosed. We studied the draining vessel for EJV and found that it drained into the confluence of IJV-subclavian vein in 15 (65.2%), into subclavian vein in 07 (30.4%), and into the IJV in 01 (4.3%) case.
Outcomes
Successful insertion
All cases (n = 23, 100%) had a successful TDC insertion with no major complications. Minor complications like kink occurred in two cases (8.6%), which were corrected. Local hematoma or blood ooze at insertion site occurred in five (21.7%) cases.
Catheter dysfunction
All cases were followed up for 6 months. Catheter dysfunction needing removal was seen in 07 (30.4%) of which 04/17 were on right side (23.5%) and 03/06 were on left side (50%), as shown in Table 2. The major cause was thrombosis of subclavian vein in 05 (21.7%), with an extension of thrombus to BCV seen in three of these cases. All five patients presented with unilateral arm swelling with features of central vein occlusion like facial swelling or prominent venous collaterals. The onset of symptoms was at 2 months of insertion in one patient, while in others, it manifested between 3 and 6 months. Infectious complications causing catheter removal included one each of refractory catheter-related bloodstream infection (CRBSI) and refractory tunnel infection, respectively. Other causes of minor catheter dysfunction included 02 (8.6%) episodes of intra-catheter thrombus managed with thrombolysis using alteplase, and CRBSI in 02 (8.6%) which was managed with intravenous antibiotics.
| Outcome | Right EJV(n = 17) | Left EJV(n = 6) | All cases(n = 23) | P value |
|---|---|---|---|---|
| Primary outcomes | ||||
| Successful insertion | 17 (100%) | 06 (100%) | 23 (100%) | |
| Catheter dysfunction causing removal | 04 (23.5%) | 03 (50%) | 07 (30.4%) | P = 0.23 |
| Thrombus SCV/BCV | 03 (17.6%) | 02 (33.3%) | 05 (21.7%) | P = 0.44 |
| CRBSI/TI | 01 (5.8%) | 01 (16.6%) | 02 (8.6%) | P = 0.42 |
| Other outcomes | ||||
| Removal with functioning TDC (PD/AVF) | 03 (17.6%) | 0 | 03 (13%) | P = 0.28 |
| Death with functioning catheter | 01 (5.8%) | 0 | 01 (4.3%) | P = 0.55 |
| Minor complications managed successfully | ||||
| During insertion | ||||
| Kink | 01 (5.8%) | 01 (16.6%) | 02 (8.6%) | P = 0.42 |
| Ooze/hematoma | 04 (23.5%) | 01 (16.6%) | 05 (21.7%) | P = 0.73 |
| Delayed complications | ||||
| CRBSI | 02 (11.7%) | 0 | 02 (8.6%) | P = 0.39 |
| Intra-catheter thrombus | 02 (11.7%) | 0 | 02 (8.6%) | P = 0.39 |
by chi square test, SCV: Subclavian vein; BCV: Brachiocephalic vein; CRBSI: Catheter-related blood stream infection; TI: Tunnel infection; TDC: Tunneled dialysis catheter; PD: Peritoneal dialysis; AVF: AV fistula.
One death recorded in the study population, was a 67-year-old diabetic, with coronary artery disease (triple vessel disease post angioplasty), moderate left ventricular dysfunction. He expired 69 days after TDC insertion, due to a myocardial infarction with acute decompensated heart failure, but had a functional EJV TDC. The patency of EJV TDC was measured by censoring unrelated patient deaths and TDC removal with a functional TDC, which occurred in three (13%) cases. The censored catheter survival was 23/23 (100%) at 1 month, 22/23 (95.6%) at 3 months, and 13/20 (65%) at 6 months.
Factors predisposing to TDC dysfunction
The study population was divided into two groups as those with major catheter dysfunction needing catheter removal, and those with patent functional catheter. The individuals in whom the catheter was removed despite a functioning TDC were included in the second group. The possible contributing factors were compared as shown in Table 3. It was seen that the EJV anatomy with regards to the vein into which EJV drains had a significant association, with EJVs draining into the subclavian vein having higher TDC dysfunction (p = 0.005) as compared to those draining into confluence or IJV.
| Parameter | Catheter dysfunction needing removalN = 7n (%N) | Functioning EJV catheterN = 16n (%N) | P value |
|---|---|---|---|
| Gender | |||
| Females | 05 (71.4%) | 08 (50%) | p = 0.35 |
| Males | 02 (28.5%) | 08 (50%) | |
| Age of patient (in years) | |||
| Age > 50 | 04 (57.1%) | 10 (62.5%) | p = 0.81 |
| Age ≤50 | 03 (42.8%) | 06 (37.5%) | |
| Diabetes mellitus | |||
| Present | 03 (42.8%) | 06 (37.5%) | p = 0.81 |
| Absent | 04 (57.1%) | 10 (62.5%) | |
| Obese | 02 (28.5%) | 3 (18.7%) | p = 0.59 |
| Nonobese | 05 (71.4%) | 13 (81.2%) | |
| Other thrombosis of BCV | |||
| Present | 00 (0%) | 04 (25%) | p = 0.15 |
| Absent | 07 (100%) | 12 (75%) | |
| Opening EJV into SVC | |||
| Opens SCV | 05 (71.4%) | 02 (12.5%) | p = 0.005 |
| Opens confluence or IJV | 02 (28.5%) | 14 (87.5%) | |
| Side of EJV catheter | |||
| Left | 03 (42.8%) | 03 (18.7%) | p = 0.23 |
| Right | 04 (57.1%) | 13 (81.2%) |
BCV: Brachicephalic vein; EJV: External jugular vein; SCV: Subclavian vein; IJV: Internal jugular vein; SVC: Superior Vena Cava; N: Total sample size, n: sub group sample size. Statistically significant p values given in bold
Discussion
We studied 23 EJV TDC catheter insertions performed by nephrologists under fluoroscopy and ultrasound support, done after evaluating the anatomy of EJV and central veins. There was 100% success without any major insertion-related complications. This was made possible by excluding any central vein occlusion along TDC course, by positioning the guidewire in the IVC (which avoided any anomalous vein), and performing the procedure under fluoroscopy to avoid malposition.
There were minor complications like ooze or hematoma in five (21.7%) cases, which are common with EJV as it is superficial, and unlike other veins, it cannot be compressed against any bony prominence.6 Kinks are common in EJV TDC, as the catheter has to traverse through multiple zig-zag paths from a superficial plane to a deep plane. Kinking was easily corrected by proper dissection of the subcutaneous tissue, breaking any fibrous bands around the entry site, and by gentle pullback of the catheter.12
Catheter dysfunction needing removal of the catheter was seen in seven cases (30.4%) in our study with the predominant cause being subclavian/central vein thrombosis in five (21.7%) cases. Park et al.12 discussed 41 cases of right-sided EJV TDC insertion by an interventional radiologist, of which 26 (63.4%) were removed. Natario et al.14 had 6 (30%) catheter removals because of mechanical, thrombotic, or infectious complications in their 20 cases of EJV TDC done by a nephrologist without fluoroscopy. Interestingly, Moini et al.16 have reported 34 cases of temporary dialysis catheters inserted into EJV, with no major complications and median catheter survival being for 20–30 dialysis sessions. Our study assessed the factors associated with catheter dysfunction and found that the EJV draining into subclavian vein had a significant association with thrombosis, with four out of five events occurring in EJVs draining into the subclavian vein. Subclavian veins are known to have a higher incidence of thrombosis compared to other central veins.5,17 The likely reason for higher thrombosis in these EJVs may be due to the catheter course involving the subclavian vein and its opening into BCV, making it more likely to thrombose. However, further studies will be needed to prove this hypothesis. If proven, the insertion of EJV TDC may be avoided in this subset of patients.
There is often a debate between using the right EJV and left IJV in patients with exhausted right IJV. The concept of avoiding the use of left IJV is to use one side of neck veins, and preserve the left side for later use of IJV and EJV.13 A few studies have directly compared these veins and found that there was better cumulative patency and lesser catheter removal in the right EJV group (n=21) as compared to the left IJV group (n=28).18 The blood flow in the EJV TDC was also found to be comparable to the left IJV in a study.19
EJV TDC insertion should be done under ultrasound and fluoroscopic guidance, to minimize complications, define the venous anatomy, and ensure correct position. If the EJV is found to be collapsed, it may be made more prominent by performing Valsalva maneuver or creating a humming sound.14 It may sometimes be difficult to maneuver the guidewire through the zig-zag EJV track, especially at its opening into the subclavian vein. This can be managed by raising the ipsilateral shoulder.20
Our study is one of the few reports of EJV TDCs performed under fluoroscopic guidance by nephrologists. This study defined the venous anatomy pre-procedure, which helped to attain 100% success rate, and discussed the factors that may be associated with EJV catheter dysfunction. The finding of a significant association of EJV thrombosis with its opening into the subclavian vein is interesting and needs further research. This association and its clinical relevance have not been discussed in the literature. The study has few limitations, being an observational study, having a small sample size, and being short of follow-up for 6 months.
Nephrologists less commonly use the EJV for TDC despite it being given high importance by KDIGO guidelines. This may be because of a lack of technical expertise needed in inserting EJV TDC, especially while maneuvering the guidewire, lack of fluoroscopy availability, and lack of awareness amongst interventionists.
Conclusion
This article aims to encourage nephrologists to consider EJV access as a safe and good option for TDC placement. The nephrologist should be sensitized to acquire the skills of TDC insertion, as they are the primary stakeholders for good vascular access. Our study shows that TDC insertion in EJV is associated with good technical success when performed under fluoroscopy. EJV TDC is associated with an acceptable rate of catheter dysfunction, especially thrombosis which is more common in EJV opening into subclavian veins.
Conflicts of interest
There are no conflicts of interest.
References
- Vascular access in haemodialysis: strengthening the Achilles’ heel. Nat Rev Nephrol. 2013;9:348-57.
- [CrossRef] [PubMed] [Google Scholar]
- Arteriovenous fistula creation by nephrologist and its outcomes: A prospective cohort study from Vietnam. BMC Nephrol. 2023;24:88.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Hemodialysis catheters: Update on types, outcomes, designs and complications. Semin Intervent Radiol. 2022;39:90-102.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Placing an appropriate tunneled dialysis catheter in an appropriate patient including the nonconventional sites. Cardiovasc Diagn Ther. 2023;13:281-90.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- KDOQI clinical practice guideline for vascular access: 2019 Update. Am J Kidney Dis. 2020;75:S1-S164.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomical variations of the external jugular vein: A pictorial and critical review. Medicina (Kaunas). 2023;59:622.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Contribution to the study of the tributaries and the termination of the external jugular vein. Surg Radiol Anat. 1994;16:173-7.
- [CrossRef] [PubMed] [Google Scholar]
- Review of the variations of the superficial veins of the neck. Cureus. 2018;10:e2826.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Placement of hemodialysis catheters through dilated external jugular and collateral veins in patients with internal jugular vein occlusions. AJR Am J Roentgenol. 2000;174:361-2.
- [CrossRef] [PubMed] [Google Scholar]
- [Catheterization of the external jugular vein for hemodialysis] Khirurgiia (Mosk) 2005:47-50.
- [PubMed] [Google Scholar]
- Percutaneous, non-surgical placement of tunneled, cuffed, external jugular hemodialysis catheters: A case report. J Vasc Access. 2007;8:126-8.
- [PubMed] [Google Scholar]
- Placement of a hemodialysis catheter using the dilated right external jugular vein as a primary route. J Korean Soc Radiol. 2010;63:351-7.
- [Google Scholar]
- Placement of long-term hemodialysis catheter (permcath) in patients with end-stage renal disease through external jugular vein. Adv Biomed Res. 2014;3:252.
- [CrossRef] [PubMed] [Google Scholar]
- Haemodialysis tunneled catheters in the external jugular vein. A single-centre experience of an alternative approach. Port J Nephrol Hypert. 2010;24:279-86.
- [Google Scholar]
- Insertion of long-term tunneled cuffed hemodialysis catheters via the external jugular vein by using a simple, safe and reliable surgical technique. J Vasc Access. 2007;8:12-6.
- [PubMed] [Google Scholar]
- Non-cuffed dual lumen catheters in the external jugular veins versus other central veins for hemodialysis patients. Saudi J Kidney Dis Transpl. 2009;20:44-8.
- [PubMed] [Google Scholar]
- Central venous obstruction management. Semin Intervent Radiol. 2009;26:115-21.
- [CrossRef] [PubMed] [Google Scholar]
- A retrospective study of preferable alternative route to right internal jugular vein for placing tunneled dialysis catheters: Right external jugular vein versus left internal jugular vein. PLoS One. 2016;11:e0146411.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A comparison between blood flow outcomes of tunneled external jugular and internal jugular hemodialysis catheters. J Vasc Access. 2012;13:51-4.
- [CrossRef] [PubMed] [Google Scholar]
- Shoulder manipulation to facilitate central vein catheterization from the external jugular vein. Anaesth Intensive Care. 1991;119:567-8.
- [CrossRef] [PubMed] [Google Scholar]








