Translate this page into:
Study of Caregiver Burden in Continuous Ambulatory Peritoneal Dialysis
Corresponding author: Shashank Sudarshan Dhareshwar, Department of Nephrology, St. Johns Medical College Hospital, Bengaluru, Karnataka, India. E-mail: shashank.dhareshwar@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Dhareshwar SS, Nithin R, Anantharam J, Kedlaya P, Satish R, Jha VK, et al. Study of Caregiver Burden in Continuous Ambulatory Peritoneal Dialysis. Indian J Nephrol. doi: 10.25259/ijn_424_23
Abstract
Background
Increased caregiver burden undermines caregivers’ mental and physical health and is an under recognized but critical aspect for the success of continuous ambulatory peritoneal dialysis (CAPD). This study was undertaken to quantify and identify the factors determining CAPD caregiver burden.
Materials and Methods
A cross-sectional study was conducted among 51 caregivers of CAPD patients visiting the centers from July to August 2023. Caregiver burden score was determined using “Zarit Burden Interview” by interview method.
Results
The mean age of caregivers was 42.8 ± 10.83 years with 52.9% females. The mean Zarit burden score of the caregivers was 29.18 ± 11.81. Younger caregivers experienced significantly higher burden (r = −0.34, P = 0.013). Lesser educated caregivers were perceiving a higher burden. Lower socioeconomic strata people had significantly higher burden (P < 0.001) and especially so when there was a loss in income attributed to caregiving. Patients who were covered by state insurance experienced a notably lower caregiver burden (19.2 ± 6.1) when compared to those who were self-financed (32.4 ± 11.08) or had company insurance (37.2 ± 13.6). Gender, religion, marital status, and type of family had no bearing on the caregiver burden.
Conclusion
Age, loss of income, education, and socioeconomic status are important determinants of caregiver burden. State sponsored program lowers caregiver burden significantly. A CAPD program should address these factors to mitigate caregiver burden.
Keywords
Chronic kidney disease
Continuous ambulatory peritoneal dialysis
Caregiver burden
Zarit burden score
End-stage renal disease
Introduction
Chronic kidney disease (CKD) is a global public health problem. In India, the prevalence of CKD is almost 17%. With the rising incidence of end-stage renal disease (ESRD), the costs related to delivery of renal replacement therapy has also come into the spotlight. In comparison to in-center hemodialysis (HD), continuous ambulatory peritoneal dialysis (CAPD) provides greater freedom, flexibility, and improved quality of life for most patients, while also being linked to reduced healthcare costs.1-5 CAPD can be performed at home by patients themselves or a caregiver and does not require infrastructure, HD requires specially trained human resource and sophisticated infrastructure. In spite of these obvious advantages, penetration of CAPD is very low as revealed in a recent survey by Jha et al. in their study “The state of nephrology in South Asia,” where they found that ∼1,75,000 and 8,500 people were receiving HD and CAPD, respectively, in India in 2018.6
Caregiver burden is a subjective experience involving multifaceted strains perceived by individuals who provide care for their family or loved ones over an extended period of time. This burden exerts adverse effects on both caregivers themselves and their dependents. CKD is a life-long condition, and its extended treatment places considerable strain on patients and their caregivers. As caregivers play a pivotal role in providing long-term patient care, comprehending and investigating the extent of their burden becomes essential. CAPD, a perpetually administered therapy, demands strict adherence to aseptic protocols during the procedure, financial support for CAPD supplies, advocating for the patient’s needs, and mastering technically intricate training. This rigorous routine can take a toll on both patients and caregivers who shoulder the procedural responsibilities. The emotional and psychosocial complexities compound the challenges they face. Amplified caregiver burden not only jeopardizes their mental and physical well-being but can also impact the quality of care and patient outcomes.7,8 Caregivers constitute a vital component of treatment protocols, with their conscientious care playing a preventive role against peritonitis and catheter loss. Yet, the daily regimen and responsibilities can become overwhelming. The accumulation of this prolonged stress has the potential to demotivate continued adherence to CAPD, potentially resulting in its inadequate use or discontinuation.
There are various ways to calculate caregiver burden, and they typically involve a combination of quantitative and qualitative assessments. Several standardized scales and questionnaires have been developed which include the Zarit Burden Interview (ZBI), caregiver strain index, and the caregiver reaction assessment. ZBI is one of the most widely used and well-studied caregiver burden assessment tools. It has been validated in a variety of populations and settings, and it has been shown to be reliable and valid.9,10
The assessment of caregiver burden is often overlooked within the realm of healthcare. Given that the efficacy of CAPD is partially reliant on the support of patients’ caregivers, we have undertaken a study to delve into the caregiver burden attributed to this treatment method. Our objective is to quantify and discern the factors that contribute to the burden experienced by caregivers of patients undergoing CAPD.
Materials and Methods
This cross-sectional study was conducted at a Medical College in South India from July to August 2023. In addition, ex-servicemen undergoing CAPD and receiving follow-up care at a Service Hospital were incorporated into the study. The evaluation of caregiver burden encompassed all caregivers of patients undergoing CAPD who were visiting the two centers. Caregivers of CAPD patients who had been admitted with complications associated with CAPD within the past month, as well as those who had commenced CAPD within the past 3 months, were excluded from the study. Using data extracted from the hospital, an average of 12 cases per month indicates an expected total of n = 48 cases. Based on this population size, using YAMANE equation for a known population size, sample size (n) = n = N/1 + Ne2 where n signifies the sample size, N is the population size, and e stands for the margin of error (for a 95% confidence level, the margin of error is typically 0.05). Substituting the given values: n = 48/1 + 48 × 0.05 × 0.05 = 48/1.12 = 42.85. Therefore, after approximating, the sample size was fixed at 50. Approval was obtained by the Institutional Review Board at St Johns Medical College Hospital, number IEC/1/735/2023, dated 15/06/2023 and the Institutional Review Board at IEC Command Hospital (Air Force), number CHAFB/IEC/32/2023, dated 13/07/2023, before commencing the study. Written informed consent was obtained from all study participants before data collection. Caregiver was defined as the person who stays with the patient, accompanies them during hospital visits, and/or oversees financial matters irrespective of whether the caregiver was physically doing the procedure or not. Information regarding sociodemographic variables and the history of CKD was gathered using a pre-tested, semi-structured questionnaire administered through interviews. The socioeconomic status (SES) was assessed using the modified Kuppuswamy scale. This modified scale encompassed three key parameters: the educational level and occupation of the head of the family, as well as the total family income. Based on the scores attributed to each of these parameters, participants were categorized into five distinct SES classes, as outlined in Table 1.11 Caregiver burden was assessed using the ZBI. This interview comprises 22 items, each rated on a 5-point Likert scale ranging from 0 (never) to 4 (nearly always), resulting in total scores that fall within the range of 0–88. The scores were interpreted as follows: 0–20 (little or no burden), 21–40 (mild to moderate burden), 41–60 (moderate to severe burden), and 61–88 (severe burden).12 The data were analyzed using the Statistical Package for the Social Sciences (Version 26.0). Quantitative variables with a parametric distribution were subjected to analysis using Student’s t-test, and when dealing with more than two groups, analysis of variance was applied. Pearson’s correlation coefficient was utilized to verify correlations between continuous variables. For variables with a non-parametric distribution, the Mann–Whitney test was employed. The definitions for the above are shown in Table 1.
| Caregiver | The person who stays with the patient, accompanies to hospital visits and manages the finances. |
| Caregiver burden | Stress and/or strain that caregivers may experience as a result of engaging in care giving tasks, affecting their mental and physical health and can also affecting care and patient outcomes. |
| Urban and rural | Caregivers staying in cities, suburbs, and towns were included under urban population. Caregivers staying in villages were included under rural population. |
| Nuclear and joint family |
Nuclear family included parents and their children. Joint family included grand-parents, parents, children, uncle, aunt, and cousins. |
| Level of education |
Secondary schooling and below were considered lesser educated. PU and above were considered better educated. |
| Employment status |
Working and engagement in any economic activity were considered employed. Caregivers not working or looking for a job were considered unemployed. |
| ZBI | The measure of caregiving burden comprises 22 questions, to which caregivers were asked to respond, assessing the impact of the patient’s disabilities on their lives and reflecting the stressors experienced due to caregiving. |
| Average monthly income | As stated by the caregiver over a 3 month period before starting peritoneal dialysis, was taken as the base line. The mean monthly income over a 3 month period before the ZBI was conducted was considered and the difference between the 2 values was taken as the loss of income |
ZBI: Zarit burden interview, PU: Pre-University
Results
The study population consisted of 51 caregivers [Supplementary Figure 1]. The demographic, social, and clinical characteristics of these caregivers are presented in Table 2. The mean age of the caregivers was 42.8 ± 10.8 years, with a female predominance (52.9%). About 62.7% of the caregivers were from urban areas, with 39.2% belonging to the upper middle class SES. The most common caregivers were wives (35.3%) and parents (33.3%). In terms of religious affiliation, 78.4% identified as Hindu, followed by Christian (11.8%) and Muslim (9.8%). Approximately 52.9% of the caregivers were from nuclear families, and 84.3% were married. About 54.9% of the caregivers were employed. The average CAPD vintage was 14.1 ± 3.9 months. The average monthly household income was Rs. 92,235.29 ± 131,250.6, while the mean income lost as a result of caregiving was Rs. 31,725.49 ± 17,197.76.
| Characteristics | Factor | Value | Zarit score | p value |
|---|---|---|---|---|
| Age (yrs) | 42.8 ± 10.83 | - | 0.013a (r = -0.34) | |
| Gender, n (%) | Male | 24 (47.1%) | 28.13 ± 10.4 | 0.55 |
| Female | 27 (52.9%) | 30.1 ± 13.1 | ||
| Residence, n (%) | Rural | 19 (37.3%) | 29.0 ± 11.8 | 0.89 |
| Urban | 32 (62.7%) | 29.5 ± 12.1 | ||
| Religion, n (%) | Hindu | 40 (78.4%) | 28.9 ± 11.2 | 0.104 |
| Muslim | 5 (9.8%) | 39.8 ± 12.0 | ||
| Christian | 6 (11.8%) | 27.5 ± 12.8 | ||
| Marital status, n (%) | Married | 43 (84.3%) | 27.5 ± 10.2 | 0.305 |
| Unmarried | 7 (13.7%) | 29.0 ± 11.9 | ||
| Separated | 1 (2%) | 47 | ||
| Type of family, n (%) | Nuclear | 27 (52.9%) | 27.2 ± 12.7 | 0.238 |
| Joint | 24 (47.1%) | 31.9 ± 10.3 | ||
| Number of family members, Mean ± SD | 5.10 ± 2.03 | |||
| Education, n (%) | Primary | 1 (2%) | 42 | 0.103 |
| Secondary | 10 (19.6%) | 35.1 ± 13.1 | ||
| PU | 11 (21.6%) | 30.2 ± 10.1 | ||
| UG | 17 (33.3%) | 23.6 ± 10.5 | ||
| PG | 12 (23.5%) | 30 ± 11.8 | ||
| Employment, n (%) | Employed | 28 (54.9%) | 28.5 ± 12.2 | 0.65 |
| Unemployed | 23 (45.1%) | 30 ± 11.5 | ||
| Change in employment, n (%) | Yes | 12 (23.5%) | 33.6 ± 12.6 | 0.134 |
| No | 39 (76.5%) | 27.7 ± 11.3 | ||
| Insurance n (%) | No insurance | 33 (64.7%) | 32.4 ± 11.08 | <0.001a |
| Company | 4 (7.8%) | 37.2 ± 13.6 | ||
| Govt. | 14 (27.5%) | 19.2 ± 6.1 | ||
| Socioeconomic status, n (%) | Upper | 8 (15.7%) | 20 ± 9.5 | <0.001 a |
| Upper middle | 20 (39.2%) | 25.4 ± 10.6 | ||
| Lower middle | 13 (25.5%) | 32.0 ± 10.1 | ||
| Upper lower | 9 (17.6%) | 39.6 ± 8.8 | ||
| Lower | 1 (2%) | 45 | ||
| Monthly income of household, Mean ± SD | 92235.29 ± 131250.6 | - | 0.48 (r = -1.01) | |
| Income lost due to caregiving | 31725.49 ± 17197.76 | - | <0.001a (r = 0.492) | |
| Caregiver health status, n (%) | Nil | 40 (78.4%) | 30.7 ± 12.3 | 0.212 |
| DM | 4 (7.8%) | 28.5 ± 4.7 | ||
| HTN | 5 (9.8%) | 22.6 ± 9.0 | ||
| Others | 2 (3.9%) | 16.5 ± 3.5 | ||
| Relation to the patient, n (%) | Husband to wife | 7 (13.7%) | 27.4 ± 11.8 | 0.98 |
| Wife to husband | 18 (35.3%) | |||
| Parent to children | 17 (33.3%) | |||
| Children to parents | 4 (7.8%) | |||
| Siblings | 3 (5.9%) | |||
| Others | 2 (3.9%) | |||
| CAPD Vintage(months) | 14.1 ± 3.9 | - | 0.09 (r=0.23) | |
| At least 1 episode of peritonitis previously, n (%) | Yes | 13 (25.4 %) | 28.8 ± 8.8 | 0.16 |
| No | 38 (74.6 %) | 31.8 ± 5.6 | ||
| Zarit score, Mean ± SD | 29.18 ± 11.81 | |||
| Severity of burden n (%) | Little | 17 (33.3%) | ||
| Mild | 20 (39.2%) | |||
| Moderate | 14 (27.4%) | |||
| No. of exchanges done per day by caregiver | 3 ± 0.52 | |||
| Caregiver doing PD, n (%) | Yes | 43 (84.3%) | 29.1 ± 11.4 | 0.934 |
| No | 8 (15.7%) | |||
SD: Standard deviation, Govt.: Government, CAPD: Continuous ambulatory peritoneal dialysis, r: Correlation coefficient, UG: Undergraduate, PG: Postgraduate, PU: Pre-University, DM: Diabetes mellitus, HTN: Hypertension, a: Statistically significant value observed.
The mean Zarit burden score of the caregivers was 29.18 ± 11.81. The burden levels were distributed as follows: 33.3% of caregivers experienced little burden, 39.2% reported mild burden, and 27.4% faced moderate burden. Among the caregivers, 84.3% were actively engaged in performing CAPD. About 25.4% of the patients had at least one episode of peritonitis in the past.
Several demographic variables were found to influence the Zarit scores. Specifically, females exhibited higher Zarit scores compared to males. Caregivers who identified as Muslim displayed higher scores than those from other religious backgrounds. Unmarried caregivers also registered higher Zarit scores. Those from joint families reported higher burden compared to those from nuclear families. All caregivers possessed some form of education, with 33.3% having an undergraduate degree and 23.5% holding postgraduate degrees. Interestingly, a negative correlation was observed between the level of education and the severity of caregiver burden (P = 0.103).
Furthermore, caregivers who were compelled to change jobs due to their caregiving responsibilities reported higher Zarit scores than those who retained the same employment (P = 0.134). Similar patterns were observed with SES, where caregivers from lower strata displayed higher burden scores. The presence or absence of insurance and SES were inversely related to Zarit scores with statistical significance.
Age also demonstrated a significant negative correlation with Zarit scores (r = −0.34, P = 0.013) [Figure 1]. Although the monthly household income displayed a weak correlation with caregiver burden (r = −0.101, P = 0.48), a noteworthy contribution to the severity of caregiver burden was observed when income was lost due to caregiving (r = −0.492, P < 0.001) [Figure 2]. Notably, 64.7% of caregivers did not possess health insurance. Remarkably, lower burden was associated with the government-sponsored CAPD program for service patients (P < 0.001) [Figure 3].
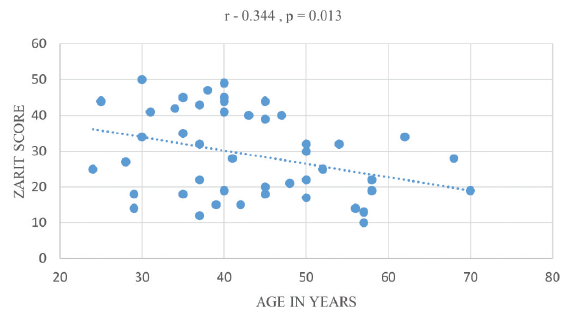
- Correlation of age with Zarit scores.
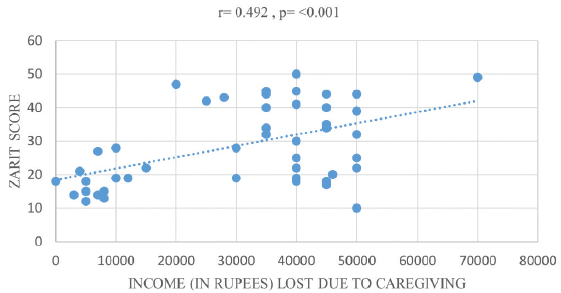
- Correlation of income lost due to care giving with Zarit scores.
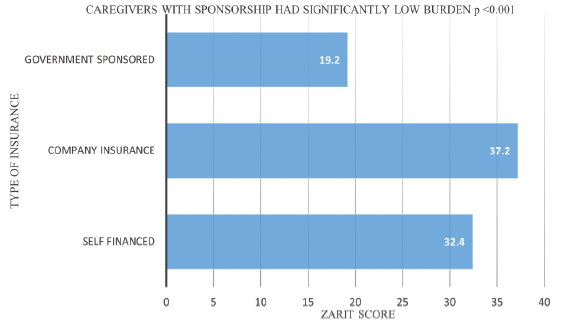
- Comparing Caregiver Zarit Score (Mean) with Insurance type.
Discussion
In a head-to-head comparison of various dialysis modalities, the results vary from country to country depending on tax breaks and government incentives.13,14 CAPD, a complex dialysis method, significantly impacts patients and caregivers’ lives, affecting their physical and psychosocial well-being.15,16 Caregivers, crucial to CAPD’s success, face increased anxiety, depression, and sleep issues, leading to a lower quality of life.17 Despite these challenges, their resilience directly influences patient survival and home dialysis support. However, the full impact of CAPD on caregivers is not fully understood.18 This study used the ZBI to assess caregiver burden and highlight the challenges they face.9,10
Our study primarily involved middle-aged caregivers, with a majority being females. A study by Nagarathnam et al. reported a similar age range, but their caregiver cohort was mainly male (mean age 43.3 ± 16.4 years, males 60%).19 In contrast, Griva et al.’s study predominantly included female caregivers (76%).20 Notably, both studies did not formally analyze caregiver burden based on gender.19,20 In our study, we noted a marginally higher average Zarit burden score in female caregivers compared to males. This could be due to females often balancing household tasks with providing CAPD assistance. An inverse relationship exists between the caregiver’s age and the perceived burden, demonstrated by a negative correlation. This finding is consistent with other studies.21,22 The observation is expected, as the younger generation, often driven by personal ambitions and career aspirations, is more susceptible to the significant impact of providing CAPD care for a family member.
Our study primarily included participants from the upper-middle-class. Notably, compromised income due to caregiving responsibilities significantly heightened caregiver burden unlike previous studies23,24 that explored the general association between income and burden, our focus was on the specific impact of income loss once CAPD care commenced. We found a weak correlation between lower income and caregiver burden, suggesting that families with sufficient monthly household income for additional expenditure were not significantly burdened when opting for CAPD. However, the loss of income due to caregiving had a substantial impact, as reflected in high Zarit scores.
Studies investigating the direct impact of education level on caregiver burden are relatively scarce. In our study, we found a negative correlation between the level of education and the severity of burden. The practice of CAPD is a technically complex procedure with multiple steps requiring stringent aseptic precautions. Among the caregivers in our study, those with lower educational levels faced challenges in comprehending the intricacies of the procedure. This difficulty could be attributed to the complex nature of CAPD. Interestingly, a study conducted by Nagarathnam et al.19 reported the opposite trend, where higher-educated individuals experienced greater burden. Notably, the study’s participant population encompassed caregivers of HD, CAPD, and transplant recipients, with a higher proportion of higher-educated individuals within the CAPD group. On the other hand, Zhang et al.23 did not find any relation between caregiver burden and educational level.
There has been no Indian study comparing mode of finance of CAPD in the context of caregiver burden. In our study, we found that patients who were covered by state insurance experienced a notably lower caregiver burden when compared to those who were self-financed or had company insurance. Specifically, among patients with insurance coverage, those enrolled in the state-sponsored CAPD program reported the least caregiver burden in contrast to other groups, a difference that held statistical significance. Remarkably, caregivers associated with patients under company insurance plans reported the highest burden. This discrepancy might arise due to the diverse reimbursement policies concerning coverage amount and duration, with company policies often being arbitrary, leading to a substantial share of out-of-pocket expenditures for both patients and caregivers. Importantly, the government-sponsored CAPD program for ex-servicemen, which encompassed all CAPD-related expenses, was associated with significantly lower caregiver burden. Zhang et al. too23 found that the financial strain imposed by medical costs related to dialysis results in increased caregiver burden due to disproportionate coverage by different insurances.
The study has its own limitations related to the cross-sectional nature of the study design, as only one assessment of ZBI was done precluding relevant longitudinal comparisons. Furthermore, only two centers were included in our study; hence, extrapolation of findings is uncertain.
Conclusion
Our study’s findings highlight that caregivers with higher burden were younger and less educated. In addition, caregivers from lower economic strata tend to experience heightened burdens. The impact of burden is significantly exacerbated when there is a loss of income due to CAPD, coupled with a lack of sponsorship. Considering these outcomes, it is imperative to incorporate an assessment of caregiver burden when evaluating the overall effectiveness of CAPD for patients. Determining the factors that influence burden, evaluating the caregiver’s needs, health status, and available financial and support resources, can lead to an improved CAPD experience. Therefore, promoting sponsorship and funding for CAPD implementation is essential. In the future, studies should focus on further elucidating these factors, devising strategies to alleviate their impact, and ultimately enhancing the quality of life for both patients and caregivers.
Conflicts of interest
There are no conflicts of interest.
References
- Similar outcomes with hemodialysis and peritoneal dialysis in patients with end-stage renal disease. Arch Intern Med. 2011;171:110-8.
- [CrossRef] [PubMed] [Google Scholar]
- Patient ratings of dialysis care with peritoneal dialysis vs hemodialysis. JAMA. 2004;291:697-703.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of patient survival between hemodialysis and peritoneal dialysis among patients eligible for both modalities. Am J Kidney Dis. 2018;71:344-51.
- [CrossRef] [PubMed] [Google Scholar]
- Cost of peritoneal dialysis and haemodialysis across the world. Nephrol Dial Transplant. 2013;28:2553-69.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic kidney disease in india: A clarion call for change. Clin J Am Soc Nephrol. 2018;13:802-4.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The state of nephrology in South Asia. Kidney Int. 2019;95:31-7.
- [CrossRef] [PubMed] [Google Scholar]
- Depression among low-income female muslim uyghur and kazakh informal caregivers of disabled elders in far Western China: Influence on the caregivers’ burden and the disabled elders’ quality of life. PLoS One. 2016;11:e0156382.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Factors associated with health-related quality of life among family caregivers of disabled older adults: A cross-sectional study from Beijing. Medicine (Baltimore). 2017;96:e8489.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The reliability, validity and feasibility of tools used to screen for caregiver burden: A systematic review. JBI Libr Syst Rev. 2009;7:1373-430.
- [CrossRef] [PubMed] [Google Scholar]
- Caregiver burden: A concept analysis. Int J Nurs Sci. 2020;7:438-45.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Socio-economic status scales updated for 2017. Int J Res Med Sci. 2017;5:3264.
- [CrossRef] [Google Scholar]
- Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist. 1980;20:649-55.
- [CrossRef] [PubMed] [Google Scholar]
- Increasing home based dialysis therapies to tackle dialysis burden around the world: A position statement on dialysis economics from the 2nd congress of the international society for hemodialysis. Nephrology. 2011;16:53-6.
- [CrossRef] [PubMed] [Google Scholar]
- Cost analysis of ongoing care of patients with end-stage renal disease: The impact of dialysis modality and dialysis access. Am J Kidney Dis. 2002;40:611-22.
- [CrossRef] [PubMed] [Google Scholar]
- Health-related quality of life and caregiver burden among peritoneal dialysis patients and their family caregivers in Japan. Perit Dial Int. 2003;23(2_suppl):200-5.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with burden in caregivers of patients with end-stage kidney disease (A systematic review) Healthcare. 2021;9:1212.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Social environmental stressors, psychological factors, and kidney disease. J Investig Med. 2009;57:583-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Evaluating burden and quality of life among caregivers of patients receiving peritoneal dialysis. Perit Dial Int. 2019;39:176-80.
- [CrossRef] [PubMed] [Google Scholar]
- Burden, coping mechanisms, and quality of life among caregivers of hemodialysis and peritoneal dialysis undergoing and renal transplant patients. Indian J Psychiatry. 2019;61:380.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Quality of life and emotional distress in patients and burden in caregivers: A comparison between assisted peritoneal dialysis and self-care peritoneal dialysis. Qual Life Res. 2016;25:373-84.
- [CrossRef] [PubMed] [Google Scholar]
- Carer’s burden of peritoneal dialysis patients. questionnaire and scale validation. Nefrol Engl Ed. 2018;38:535-44.
- [CrossRef] [PubMed] [Google Scholar]
- Psychosocial aspects of children and families of children treated with automated peritoneal dialysis. Pediatr Nephrol. 2013;28:2157-67.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Burden in primary family caregivers caring for uremic patients on maintenance peritoneal dialysis. Perit Dial Int. 2020;40(6):556-62.
- [CrossRef] [PubMed] [Google Scholar]
- Psychological and emotional status, and caregiver burden in caregivers of patients with peritoneal dialysis compared with caregivers of patients with renal transplantation. Transplant Proc. 2013;45:883-6.
- [CrossRef] [PubMed] [Google Scholar]








