Translate this page into:
Comparison of Different Equations with GFR Measured by Scintigraphy in Kidney Donors
Corresponding author: Prashant C Dheerendra, Department of Nephrology, Apollo Hospitals, Bangalore, Karnataka, India. E-mail: cdprash@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vinodh G, Dheerendra PC, Anitha A, Anandkumar DG, Vellakampadi D, Gokulnath. Comparison of Different Equations with GFR Measured by Scintigraphy in Kidney Donors. Indian J Nephrol. 2024;34:487-92. doi: 10.25259/ijn_417_23
Abstract
Background:
Technetium-99m diethylene-triamine-pentaacetate (99mTc-DTPA)-based scintigraphy is a convenient way to assess measured glomerular filtration rate (mGFR) in kidney donors. Equations have been developed to calculate GFR in the general population. This study aims to identify the best among commonly employed equations to better predict GFR when compared with scintigraphy-based mGFR. Also, the trends in mGFR values were studied over 1 year post-donation.
Materials and Methods:
Thirty-four kidney donors were recruited for this study from November 2017 to November 2018 and followed-up for a year. Estimated GFR (eGFR) was calculated using the Modification of Diet in Renal Disease (MDRD) Equation, Chronic Kidney Disease Epidemiology (CKD-EPI) Collaboration equation, and Nankivell formula; the values were compared to that obtained using 99mTc-DTPA both pre-and post-donation. Correlation and agreement between the eGFR and mGFR were studied using Statistical Package for the Social Sciences (SPSS) version 23.0 and Microsoft Excel.
Results:
mGFR was augmented by 32.3 ± 27.8% in the remnant kidney post-donation. The baseline mGFR, post-donation mGFR, and the quantum of its increase post-donation did not differ between overweight donors and donors with normal body mass index (BMI). mGFR correlated poorly with all the eGFR equations both pre- and post-donation. Bland-Altman analysis showed weak agreement with significant bias and variance between mGFR and all eGFR equations.
Conclusion:
In Indian kidney donors, mGFR by 99mTc-DTPA scintigraphy shows poor correlation and agreement with the commonly used eGFR equations. An individualized approach is needed to assess the kidney function of live donors to minimize harm to both the recipient and the donor.
Keywords
mGFR
eGFR
DTPA
Donor nephrectomy
CKD-EPI
Introduction
Kidney donation is a safe procedure in the short term but confers an elevated risk for kidney failure, cardiovascular mortality, and all-cause mortality over the long term.1 Hence, a comprehensive evaluation of the donor kidney function assumes heightened significance, keeping in mind the medical dictum of “primum non nocere” (first, do no harm).
The preferred method for assessing total renal function is the measurement of glomerular filtration rate (GFR). Creatinine clearance, requiring a 24-h urine collection, is commonly used for donor evaluation but has errors associated with timed collection and tubular secretion of creatinine. Inulin clearance is the gold standard to measure GFR but is cumbersome and impractical in daily clinical practice. Technetium-99m diethylene-triamine-pentaacetate (99mTc-DTPA) is a radionuclide that is useful to get a value of measured GFR (mGFR). Two methods are generally used to obtain mGFR using 99mTc-DTPA—a scintigraphy-based method and a plasma sampling method. The plasma sampling method involves repeated blood sampling though it is more accurate compared to the scintigraphy-based method.2 It also needs measurement of activity in the syringe before and after injection of the radionuclide and hence is a time-consuming process.3 The scintigraphy-based method is easier and quicker to perform.4,5
Various estimated GFR (eGFR) equations have been formulated based on patient characteristics like age, gender, race, serum creatinine, etc. While the equations are easy to use and inexpensive, they have not been validated in Indian kidney donors. The commonly used equations are the Modification of Diet in Renal Disease (MDRD) equation, Chronic Kidney Disease Epidemiology (CKD-EPI) Collaboration equation, and the Nankivell equation.6–8 The MDRD equation was derived from patients with kidney disease and underestimates GFR in people with good renal function.9 The CKD-EPI equation is the recommended equation for GFR estimation in people with normal renal function.10 Three variants of the equation are used incorporating serum creatinine or serum cystatin or both.6,11 The CKD-EPI creatinine is the most commonly used. The Nankivell formula is the only one derived from patients with a single functioning kidney after receiving a kidney transplant.8
Despite the availability of these equations, none of them has been validated among Indian renal donors. In this study, we aimed to evaluate which equation accurately estimated GFR pre- and post-donor nephrectomy when compared to 99mTc-DTPA-based scintigraphy measured GFR (mGFR). Also, we studied the trends in mGFR over a period of 1 year after donation.
Materials and Methods
Study participants
In this prospective observational study, a total of 34 live kidney donors who were evaluated at the Department of Nephrology at our hospital from November 2017 to November 2018 were included. The study was initiated after receiving approval from the Institutional Ethics Committee of the Scientific Review Board, number AplBlr/SRB/ DNB/0023/2017, dated 15/9/2017. Written informed consent was obtained from all participants.
Laboratory study
Donors were evaluated based on clinical history, physical examination, and laboratory investigation. Serum creatinine was measured using Jaffe’s uncompensated photometric method with a Beckman Coulter AU 680 pre-donation and 1 year post-donation. Other routine blood tests were done as part of donor work-up and follow-up.
A dynamic renal study (Gates’ method) was conducted utilizing 99mTc-DTPA as a radiotracer to determine the GFR level pre-donation and at 1 year post-donation. An intravenous injection of 99mTc-DTPA (3-5 millicurie) was administered prior to the scan. Dynamic imaging, with the participant in the supine position, was carried out using a gamma camera at an acquisition rate of 1 frame/3 seconds for 1 min and subsequently 1 frame/19 seconds for 19 min. GFR was calculated using the algorithm from Gates’ software. The eGFR was calculated based on serum creatinine level using the four variable MDRD equation, CKD-EPI creatinine equation, and Nankivell formula.
Statistical analysis
Categorical variables were represented as numbers or percentage. Continuous variables were represented as mean ± standard deviation. Spearman correlation was used to determine the correlation between mGFR and eGFR values.
Bland-Altman analysis was performed to study the agreement between mGFR and eGFR by various equations. The analysis plots the mean of the GFR obtained by the two methods along X axis against the difference between them along the Y axis. The plot was used to calculate bias and variance of eGFR compared to mGFR.
A p-value <0.05 was considered significant. Microsoft Excel and the Statistical Package for the Social Sciences (SPSS) version 23 software were used for all statistical analyses.
Results
Description of the study population
Thirty-four participants were evaluated in this study. The donors evaluated in the study were predominantly female (n = 28) as compared to males (n = 6). Age and BMI were not significantly different across the genders. Of the 34 donors, 22 were overweight and had a BMI of more than 25 kg/m2.
Twenty-four (70.5%) participants completed the 1-year follow-up. Lack of follow-up was mainly due to financial or logistical reasons. Table 1 depicts the important baseline characteristics of the participants.
| Parameter | Values |
|---|---|
| Age, Years (n = 34) | 47.5 (11.9) |
| Gender—Number of Females (%) | 28 (82.4%) |
| Pre-Diabetes—Number (%) | 9 (26.5%) |
| Hypertension—Number (%) | 4 (11.8%) |
| Overweight—Number (%) | 22 (64.7%) |
| Body Mass Index | 27.3 (4.7) |
| Pre-surgery Creatinine in Males, mg/dL (n = 6) | 0.98 (0.09) |
| Pre-Surgery Creatinine in Females, mg/dL (n = 28) | 0.74 (0.10) |
Frequency has been represented as number (%) while age, BMI, and serum creatinine values have been represented as mean ± standard deviation.
Changes in GFR by 99mTc-DTPA pre- and 1 year post-donation
Mean GFR measured by 99mTc-DTPA pre-donation was 104.49 ± 10.38 mL/min/1.73m2. The mean pre-donation mGFR of the remnant kidney was 51.41 ± 6.36 mL/min/1.73m2. Mean mGFR 1 year after donation was 67.30 ± 12.33 mL/min/1.73m2. The mGFR of the remnant kidney increased by an average of 32.3 ± 27.8%.
When mGFR values were compared in patients with BMI less than 25 kg/m2 (normal BMI) and more than 25 kg/m2 (overweight), no difference was found in the pre-donation values (102.33 ± 11.91 mL/min/1.73m2 vs 105 ± 10.02 mL/min/1.73m2, p = 0.56), post-donation values (67.88 ± 16.41 mL/min/1.73m2 vs 67.07 ± 11.00 mL/min/1.73m2, p = 0.89), and the quantum of increase of mGFR in the remnant kidney after donation (17.71 ± 15.14 mL/min/1.73m2 vs 15.17 ± 12.01 mL/min/1.73m2, p = 0.68).
Correlation and agreement between mGFR and eGFR
mGFR using 99mTc-DTPA was compared with eGFR obtained from the equations in donors both pre- and post-surgery. Although the estimated GFR results across formulas correlated strongly with each other, mGFR values correlated poorly with eGFR values as estimated by MDRD (p-value = 0.628) and CKD-EPI (p-value = 0.573) equations pre-surgery. Similarly, mGFR 1 year post-surgery correlated poorly with eGFR by MDRD (p-value = 0.300), CKD EPI (p-value = 0.368), or Nankivell (p-value = 0.301) equations. The correlation coefficients of the various methods are depicted as a correlation matrix in Figure 1.

- Correlation matrix of GFR measurements by various methods pre- and 1 year post-donation. There was poor correlation of mGFR with the commonly used eGFR equations. Generally, there was a strong correlation between the equations. The strongest correlation was between MDRD and CKD-EPI equations at both time points. DTPA= Technetium-99m diethylene-triamine-pentaacetate (99mTc-DTPA) GFR, MDRD = Modification of Diet in Renal Disease equation, CKD-EPI = Chronic Kidney Disease Epidemiology Collaboration equation, mGFR: measured glomerular filtration rate
Accuracy of estimation, defined as proportion of eGFR values within 10% of the mGFR values, was low across all formulas. Pre-donation, 74% values of eGFR by MDRD and 56% values by CKD-EPI differed from the 99mTc-DTPA based mGFR by a margin of more than 10%. Post-donation the proportions were 58%, 62.5%, and 67% for MDRD, CKD-EPI, and Nankivell formulas respectively.
Bland-Altman analysis evaluates the differences between two methods across the range of measurement. Comparison of methods by Bland-Altman analysis demonstrated high variability across mGFR and eGFR methods [Table 2]. mGFR demonstrated a positive bias pre-surgery when compared to both MDRD and CKD-EPI equations. This means that, on an average, mGFR values were higher than the eGFR values pre-surgery. Interestingly, post-surgery mGFR showed a negative bias compared to all the equations.
| Measured GFR | Estimated GFR | Bias | SD of Bias | 95% Limits of Agreement |
|---|---|---|---|---|
| Tc99-DTPA (Pre-Surgery) | MDRD | 15.25 | 16.05 | (−16.21 to 46.72) |
| CKD-EPI | 11.78 | 15.35 | (−18.3 to 41.86) | |
| Tc99-DTPA (Post-Surgery) | MDRD | −0.5352 | 17.48 | (−34.8 to 33.73) |
| CKD-EPI | −4.226 | 19.14 | (−41.73 to 33.28) | |
| Nankivell | −10.62 | 19.21 | (−48.28 to 27.04) |
GFR: Glomerular filtration rate, DTPA: Diethylenetriamine pentaacetate, CKD-EPI: Chronic kidney disease-Epidemiology collaboration, MDRD: Modification of diet in renal disease
Figures 2 and 3 depict the Bland-Altman analysis as a scatterplot. Both the figures show a few common characteristics. Data points clustered close to the zero line suggest strong agreement in Bland-Altman plots, but in this study, a sizeable number of points are distant from the zero line. Data points close to the bias line (dotted black line) suggest a strong correlation between the methods. But in our study a majority of the data points are away from the bias line. The range of limits of agreement (dotted red lines) is noted to be wide.
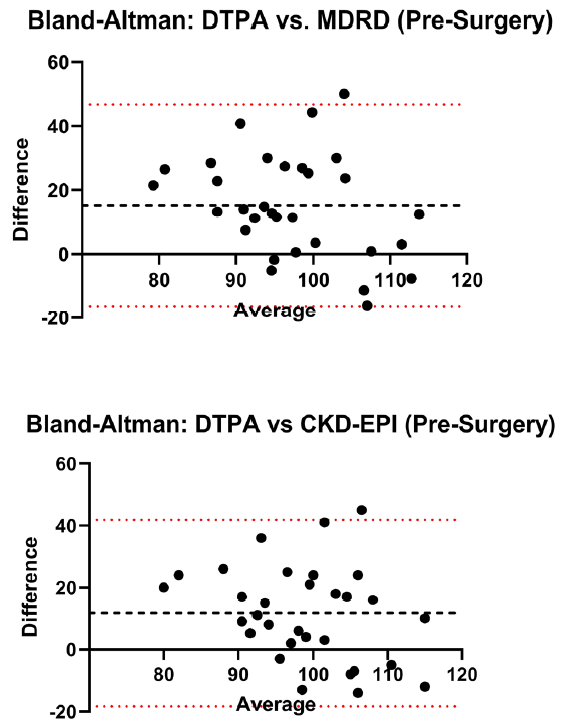
- Comparison of methods by Bland-Altman analysis demonstrated high variability, poor agreement, and positive bias across mGFR and eGFR methods pre-donation. DTPA = Technetium-99m diethylene-triamine-pentaacetate (99mTc-DTPA) GFR, MDRD = Modification of Diet in Renal Disease equation, CKD-EPI = Chronic Kidney Disease Epidemiology Collaboration equation.
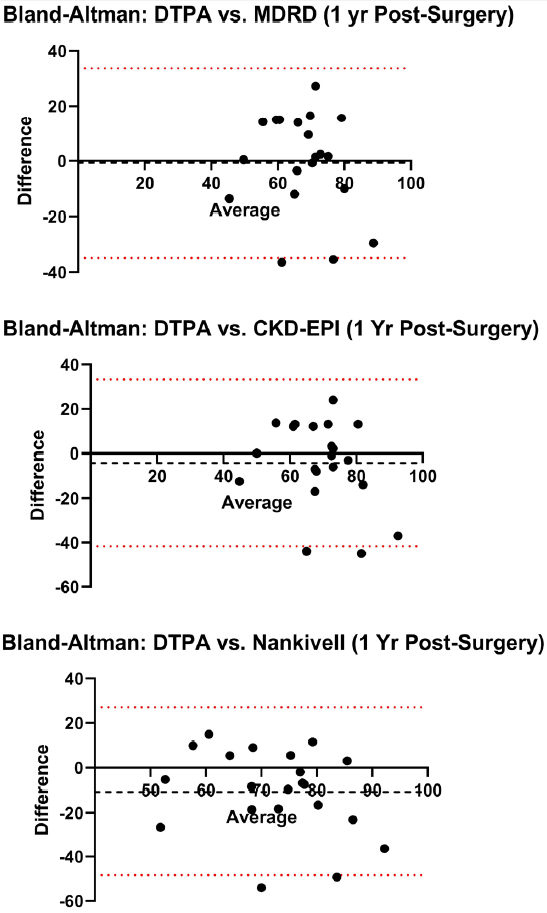
- Post-donation analysis of mGFR and the eGFR equations continued to show high variability and poor agreement but the bias was now negative. DTPA = Technetium-99m diethylene-triamine-pentaacetate (99mTc-DTPA) GFR, MDRD = Modification of Diet in Renal Disease equation, CKD-EPI = Chronic Kidney Disease Epidemiology Collaboration equation, mGFR: measured glomerular filtration rate, eGFR: estimated GFR.
Discussion
Evaluation of renal function in live kidney donors is an important part of pre-donation assessment. While many formulas are used, their validity in renal donors as a unique subpopulation is not well established in the Indian context. It is a common practice to perform tests to assess measured GFR for kidney donors.
Donors with BMI higher than 25 kg/m2 formed a substantial proportion (22 out of 34 donors) of donors in our study. There was no difference in pre- and post-donation mGFR between overweight and normal donors. In contrast, the study by Gozdowska et al. (n = 25) found a significant negative correlation between BMI and mGFR using methods similar to our study.12 A much larger retrospective study (n = 1878) also found a negative correlation between BMI and mGFR in obese women, though it used clearance of Cr-51-EDTA as the method to measure GFR.13
Our study confirmed a lack of accuracy of the eGFR equations compared to mGFR by 99mTc-DTPA scintigraphy noted previously in renal donors. Mahajan studied 122 renal donors from India and observed that median percentage absolute difference between the estimated GFR by MDRD and measured GFR was 20.8%.14 In Polish kidney donors, 73% of eGFR values estimated by MDRD and 67% by CKD-EPI differed by a margin of more than 10% from the scintigraphy-based mGFR using 99mTc-DTPA—findings similar to our study.15 Interestingly, the same study found that of 11 equations, mGFR by 99mTc-DTPA correlated best with the Nankivell formula with a correlation coefficient of 0.47 and p = 0.009.
Bland-Altman analysis is used to assess agreement between two methods of measurement. While correlation analysis looks at the strength of linear relationship between variables, Bland-Altman analysis looks at the differences and constructs limits of agreement within which 95% of the observed values occur. Most studies confirm the lack of agreement between mGFR by 99mTc-DTPA and eGFR.12,14–17 Specifically, the limits of agreement on Bland- Altman analysis need to be evaluated in a clinical context. In the present study, the limits of agreement are too wide to be clinically acceptable.
Ours is one of the few studies which have performed a follow-up mGFR estimation after donor nephrectomy. The GFR in the remnant kidney increased substantially (mean 32.3%) as previously reported in Indian kidney donors by Bahirani et al. and Chavan et al. with the mean increase after 3 months being 16.7 % and 21.2%, respectively.18,19 More importantly, as noted in the present study, overweight and obese donors had a similar augmentation in mGFR compared to donors with normal BMI.19 A study by Chen et al. measured GFR by 99mTc-DTPA at 1 month and 12 months after donor nephrectomy and concluded that a bulk increase in GFR occurred within the first month.20 The correlation and agreement between mGFR and eGFR continued to be weak post-donation.
Using plasma sampling of a radionuclide-like 99mTc-DTPA is more accurate than the Gates method to assess mGFR, even though the method is more cumbersome.21,22 Simplification of the plasma sampling method by limiting to a single blood draw or applying a correction factor based on large numbers of measurements in the population has been described.2,23 Their utility in clinical practice requires further study.
However, there are certain limitations to this study. The study had a relatively small sample size, and the follow-up period was short. In addition, there were more dropouts during the follow-up study than initially anticipated because of financial and logistical reasons. Instead of utilizing inulin clearance, which is considered the gold standard for measuring GFR, the study relied on scintigraphic measurement of GFR by Tc-99m DTPA, a more convenient method.
Conclusion
Kidney donation for transplantation carries some risk, particularly for those with preexisting medical issues. Reassuringly, overweight and obese donors have an increase in mGFR that is comparable to donors with normal BMI at the end of 1 year post-donation. Accurate evaluation of kidney function in donors is made more challenging by poor correlation and agreement between mGFR by Tc-99m DTPA scintigraphy and eGFR by the commonly used equations. mGFR obtained by plasma sampling after injection of Tc-99m DTPA is more accurate compared to the Gates’ method based on scintigraphy. The agreement of the plasma sampling method with scintigraphy-derived mGFR and the eGFR equations needs to be looked at in larger studies. It may be possible to calculate a correction factor based on a large population study comparing mGFR by scintigraphy and plasma sampling. This may allow clinicians to get a more accurate estimate of GFR while retaining the convenience of the scintigraphic method.
Acknowledgement
All authors would like to thank Apollo Hospitals, Bangalore for providing the necessary facilities to complete this work.
Conflicts of interest
There are no conflicts of interest.
References
- Comparison of glomerular filtration rate measurement methods between radionuclide in vivo scintigraphic gates’ and Plasma Sampling. Open Access Maced J Med Sci. 2019;7:2734-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Radiation oncology physics: a handbook for teachers and students. Vienna: International Atomic Energy Agency; 2005. p. :657. (STI/PUB)
- Application of newer clearance techniques for the determination of glomerular filtration rate. Curr Opin Nephrol Hypertens. 1998;7:675-80.
- [CrossRef] [PubMed] [Google Scholar]
- Split renal function testing using Tc-99m DTPA. A rapid technique for determining differential glomerular filtration. Clin Nucl Med. 1983;8:400-7.
- [CrossRef] [PubMed] [Google Scholar]
- Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006;145:247-54.
- [CrossRef] [PubMed] [Google Scholar]
- A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604-12.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Predicting glomerular filtration rate after kidney transplantation. Transplantation. 1995;59:1683-9.
- [CrossRef] [PubMed] [Google Scholar]
- Using serum creatinine to estimate glomerular filtration rate: Accuracy in good health and in chronic kidney disease. Ann Intern Med. 2004;141:929-37.
- [CrossRef] [PubMed] [Google Scholar]
- A unifying approach for GFR estimation: Recommendations of the NKF-ASN task force on reassessing the inclusion of race in diagnosing kidney disease. Am J Kidney Dis. 2022;79:268-288.e1.
- [CrossRef] [PubMed] [Google Scholar]
- Estimating glomerular filtration rate from serum creatinine and cystatin C. N Engl J Med. 2012;367:20-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Glomerular filtration rate estimation in prospective living kidney donors: Preliminary study. Transplant Proc. 2014;46:2592-7.
- [CrossRef] [PubMed] [Google Scholar]
- Extracellular fluid volume and glomerular filtration rate in 1878 healthy potential renal transplant donors: Effects of age, gender, obesity and scaling. Nephrol Dial Transplant. 2012;27:1429-37.
- [CrossRef] [PubMed] [Google Scholar]
- Assessing glomerular filtration rate in healthy Indian adults: A comparison of various prediction equations. J Nephrol. 2005;18:257-61.
- [PubMed] [Google Scholar]
- Formulas estimating glomerular filtration rate in the evaluation of living kidney donor candidates: Comparison of different formulas with scintigraphy-measured glomerular filtration rate. Transplant Proc. 2021;53:773-8.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison between two-sample method with 99mTc-diethylenetriaminepentaacetic acid, Gates’ method and estimated glomerular filtration rate values by formula based methods in healthy kidney donor population. Indian J Nucl Med. 2017;32:188-93.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Comparison of estimated GFR and measured GFR in prospective living kidney donors. Int Urol Nephrol. 2015;47:201-8.
- [CrossRef] [PubMed] [Google Scholar]
- Is DTPA the gold standard for glomerular filtration rate estimation in voluntary kidney donors before and after donor nephrectomy? Journal of Clinical and Diagnostic Research. 2021;15
- [Google Scholar]
- Measured glomerular filtration rate in live related kidney donors three months post-kidney donation: A single-center experience from western India. Cureus. 2023;15:e45103.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Compensatory changes in the retained kidney after nephrectomy in a living related donor. Transplant Proc. 2012;44:2901-5.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of methods for determination of glomerular filtration rate: Tc-99m-DTPA renography, predicted creatinine clearance method and plasma sample method. Ann Nucl Med. 2003;17:561-5.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of body mass index on gates method of glomerular filtration rate estimation: A comparative study with single plasma sample method. Indian J Nucl Med. 2019;34:19-23.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Comparison between three techniques for determining glomerular filtration rates: 99mTc-diethylene triamine penta-acetic acid renography, double plasma sampling method, and single plasma sampling method in Vietnamese patients. Indian J Nucl Med. 2021;36:300-3.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]








