Concomitant Histological Features of Membranous Nephropathy and Anti-Neutrophil Cytoplasmic Antibody Associated Vasculitis
Corresponding author: Vinoi George David, Department of Nephrology, Christian Medical College, Vellore, Tamil Nadu, India. Email: vinoigd@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Rajesh C, Mishra U, Roy S, Alam R, Raj Mani SS, Eapen JJ, et al. Concomitant Histological Features of Membranous Nephropathy and Anti-Neutrophil Cytoplasmic Antibody Associated Vasculitis. Indian J Nephrol. 2025;35:105-8. doi: 10.25259/IJN_140_2024
Abstract
The simultaneous occurrence of vasculitic glomerulonephritis and membranous nephropathy is unusual. We report two cases that presented to our outpatient department with rapidly progressive renal failure. On evaluation, in one patient, anti-myeloperoxidase (MPO) titers were high, and renal biopsy was suggestive of concurrent necrotizing and diffuse crescentic anti-MPO anti-neutrophil cytoplasmic antigen-associated glomerulonephritis with the circumferential cellular crescent formation and membranous glomerulopathy. He responded to plasmapheresis followed by maintenance immunosuppression with oral cyclophosphomide. Another patient was treated with Methylprednisolone and two doses of rituximab. Both the patients showed marked symptomatic improvement and became dialysis independent with stable creatinine at 3 months.
Keywords
Anti-neutrophil cytoplasmic antibody associated Vasculitis
Crescentic glomerulonephritis
Membranous nephropathy
Plasmapheresis
Rapidly progressing renal failure
Introduction
Membranous nephropathy (MN) is histologically characterized by subepithelial immunoglobulins deposits and complement.1 Vasculitic or crescentic glomerulonephritis is rarely seen in MN except in systemic lupus erythematosus.2,3 There are only a few cases with Wegener’s granulomatosis that combine MN and crescentic glomerulonephritis.4 Our knowledge of the immunopathogenesis, clinical features, treatment and outcomes of this unusual combination of membranous nephropathy and vasculitic or crescentic glomerulonephritis is limited. We report two patients who had concomitant necrotizing crescentic anti-MPO (Myeloperoxidase) associated glomerulonephritis and MN.
Case Reports
Case 1
A 58-year-old man with no known comorbidities presented with nonspecific pain abdomen. On evaluation, he was found to have hypertension, Serum creatinine - 3.4 mg/dl) and hematoproteinuria. At 12 days, his serum creatinine worsened to 10 mg/dl, and his anti MPO tires were >200 RIU/ml. Renal biopsy [Figure 1] suggested crescentic glomerulonephritis with IgG deposits. He was treated with a methylprednisolone pulse and four sessions of plasmapheresis. He required three sessions of hemodialysis, and was started on prednisolone and oral cyclophosphamide. At 3 months, he became dialysis independent.
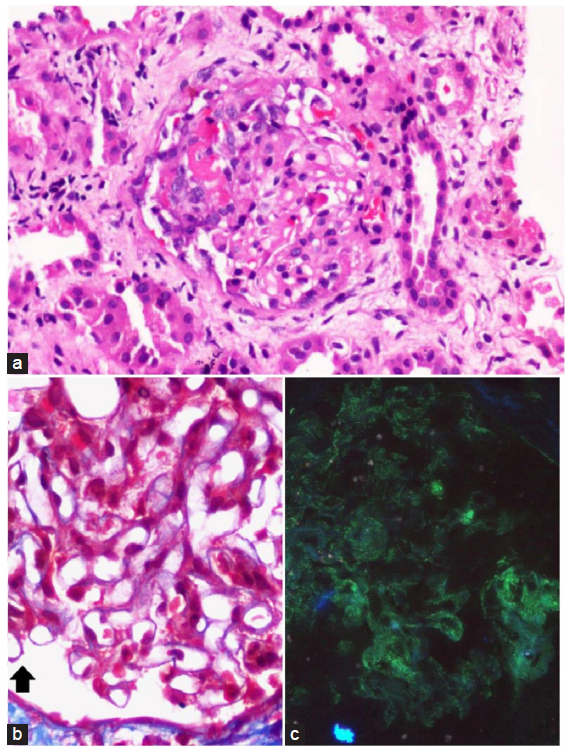
- (a and b) Glomerulus showing segmental fibrinoid necrosis and cellular crescent formation (Hematoxylin and Eosin stain) with concomitant segments of capillary wall thickening and subepithelial fuschinophilic deposits (bold black arrow in b), Masson trichrome stain), original magnifications X40. (c) Immunofluorescence microscopy depicting global fine granular (3+ intensity staining for IgG), original magnifications X40.
Case 2
A 51-year-old lady with no known comorbidities presented with acute febrile illness decreased urine output, and generalized swelling of the body. On evaluation, she was found to have hypertension and serum creatinine of 1.4 mg/dl. Over two weeks, she had rapidly worsening creatinine to 10 mg/dl and required hemodialysis. Her anti MPO titre were >200 RIU/ml. Renal biopsy suggested crescentic glomerulonephritis [Figure 2] with IgG deposits. She was given a methylprednisolone pulse and two doses of rituximab. At 3 months, she became dialysis independent. The clinical and renal biopsy findings and treatment details of both patients are mentioned in Table 1.
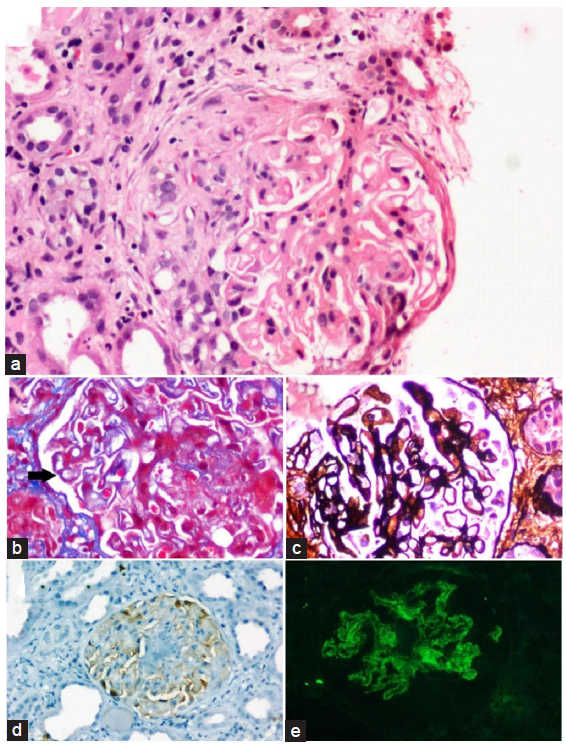
- (a) Glomerulus showing circumferential fibro cellular crescent formation, Hematoxylin and Eosin stain, (b) concomitant segments of capillary wall thickening and subepithelial fuschinophilic deposits (bold black arrow) Masson trichrome stain, (c) Segments of structural capillary wall abnormalities with spike formation, Jones methenamine silver stain, (d) PLA2R immunohistochemistry shows faint non diagnostic staining of podocytes(interpreted to be negative), original magnifications X40. (e) Immunofluorescence microscopy depicting global fine granular (3+intensity staining for IgG), original magnifications X40. PLA2R: phospholipase A2 receptor.
| Case 1 | Case 2 | |
|---|---|---|
| Age/Gender | 58/M | 51/F |
| Mode of presentation | RPRF | RPRF |
| BP at presentation (mm Hg) | 160/100 | 150/100 |
| Index serum creatinine (mg/dl) | 3.5 | 1.5 |
| Serum creatinine (mg/dl) at the time of biopsy at 10 days | 10.2 | 9.6 |
| Urine routine | RBC-8, Protein-2+ | RBC-10, Protein-3+ |
| 24 hour urine protein/creatinine ratio | 3.9 | 7.8 |
| Serum albumin (gm/dl) | 4.1 | 2.5 |
| Anti MPO tires RIU/ml | >200 | >200 |
| Anti GBM | Not done | Negative |
| Complements | Normal | Normal |
| Renal biopsy | ||
| No. of glomeruli | 11 | 10 |
| Globally sclerosed glomeruli | 2 | 2 |
| Glomeruli with active vasculitic lesions | 8 glomeruli showed circumferential cellular with crescent formation |
2 -glomeruli showed circumferential cellular crescents 5-glomeruli showed with fibrous crescent formation 1-glomerulus showed fibro cellular crescent |
| Tubular changes | Diffuse acute tubular necrosis, many tubules show intraluminal RBC casts | Diffuse acute tubular necrosis |
| Intersititum | 40% fibrosis | 50-60% fibrosis |
| Immunofluorescence | IgG (2+) membranous pattern | IgG (3-4+) membranous pattern |
| IHC for PLA2R | Not done | Negative |
| Treatment details | ||
| Induction |
MP pulse (Day 1-1 gram, Day 2 – 500 mg and Day 3- 500 mg Plasmapheresis |
MP pulse (Day 1-1 gram, Day 2 – 500 mg and Day 3- 500 mg Rituximab (1 gram two weeks apart) |
| Maintenance immunosupression | Pred/oral cyclophosphamide (1 mg/kg body weight) | Rituximab 1 gram at 4, 8, 12 and 16 months |
| Hemodialysis requirement | Yes | Yes |
| Serum creatinine (mg/dl) at 3 months | 2 | 2.5 |
| At 3 months - Off hemodialysis | Yes | Yes |
| Complications | ||
| Catheter related | Nil | Nil |
| Plasmapheresis related | Nil | Not applicable |
| Dialysis related | Nil | Nil |
| Immunosuppression related | Nil | Nil |
ANCA: Anti neutrophil cytoplasmic antibody; GBM: Glomerular basement membrane; MP: Methyl prednisolone; MPO: Myeloperoxidase; Pred: Prednisolone; RPRF: Rapidly progressing renal failure, BP: Blood pressure, IHC: Immunohistochemistry, PLA2R: Phospholipase A2 receptor.
Discussion
Immunoglobulin deposits are usually absent in the glomeruli of patients with anti neutrophil cytoplasmic antibody (ANCA)-associated glomerulonephritis. It is proposed that ANCA does not damage the glomerulus directly. Still, neutrophils activated by ANCA integrate into capillary walls and release several protein-degrading enzymes, and, finally, these pathological changes may cause necrosis to glomerular capillary walls.5 Membranous glomerulopathy has subepithelial deposits of immunoglobulins and complement, with microscopic changes in the glomerular basement membrane, including spike and bubbling formations. The association of membranous nephropathy and vasculitic/crescentic glomerulonephritis is found in fewer than 5% of cases of membranous nephropathy, usually with anti-PR3 antibodies.6 Tse et al. reported 10 cases of MN superimposed with vasculitic glomerulonephritis; four were ANCA-positive.6 Their kidney function recovered with immunosuppressive therapy and plasma exchange, except for one patient in whom the renal pathological findings were especially severe. Nasr et al. reported 14 patients with membranous glomerulonephritis (MGN) and ANCA-associated glomerulonephritis (ANCA-GN) and identified the rate of crescent formation as a risk factor for developing ESRD.7 This unusual combination of MN with vasculitic/crescentic glomerulonephritis, although often idiopathic,8,9 can occur in association with systemic lupus erythematous and anti-GBM antibodies,10 and ANCA-positive or negative systemic vasculitis. MN complicated by vasculitic glomerulonephritis appears to have a more aggressive clinical course than membranous nephropathy alone. Nakada et al. reported a case of concurrent MPO-/PR3-Negative ANCA-GN and membranous glomerulopathy.11 At present, any association between MN and ANCA-GN is unclear. Matsumoto et al. postulated a hypothesis that MPO is highly cationic; it can bind to anionic surfaces such as GBM or endothelial cells and possibly behave as a planted antigen. In anti MPO- GN, MPO released from neutrophils could be localized on the glomerular capillary walls, where it could interact with MPO-ANCA. This might explain why membranous glomerular lesions were induced during MPO-ANCA-associated GN.12 On the other hand, Nasr et al.7 suggested that the concurrence of MN and ANCA-GN may just be by chance because they occur together too infrequently to be related pathologically.
Our first patient received plasmapheresis followed by maintenance immunosuppression with cyclophosphamide as per methylprednisolone plasma exchange (MPEX),13 a randomized controlled trial by Szpirt et al.14 and CYCLOPS trials.15,16 The second patient received a methylprednisolone pulse followed by two doses of Rituximab based on induction trials in ANCA vasculitis like rituximab in ANCA associated vasculitis (RAVE) and rituximab versus cyclophosphamide in ANCA associated vasculitis (RITUXIVAS).17-19 She was planned to continue ritxuimab for maintenance immunosuppression based on the maintenance of remission using rituximab in ANCA associated vasculitis (MAINRITSAN) trial.20 Currently, both patients are dialysis independent, but they require long-term follow-up for relapses or worsening renal functions. Lack of serum PLA2R levels in both patients, IgG sub-classification, and tissue PLA2R in one patient were limitations of this study.
The association of MN and vasculitic/crescentic glomerulonephritis is rare and appears to have a more aggressive clinical course compared to membranous nephropathy alone. Early detection and treatment will have a good prognosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
References
- Primary glomerular disease. In: Brenner BM, Rector FC Jr, eds. The Kidney (3rd edn). Philadelphia: Saunders; 1986. p. :929-1013. http://nek.istanbul.edu.tr:4444/ekos/TEZ/25496.pdf
- [Google Scholar]
- Lupus membranous nephropathy: Long-term outcome. Clin Nephrol. 1993;39:175-82.
- [PubMed] [Google Scholar]
- Membranous glomerulonephritis. In: Heptinstall RH, ed. Pathology of the Kidney (4th edn). Boston: Little, Brown; 1992. p. :559-626. https://link.springer.com/chapter/10.1007/978-0-387-31127-2_2
- [Google Scholar]
- Coexistence of anti-neutrophil cytoplasmic antibody-associated glomerulonephritis and membranous glomerulopathy. Am J Clin Pathol. 1993;99:211-5.
- [CrossRef] [PubMed] [Google Scholar]
- Antineutrophil cytoplasmic antibodies. Lancet. 2006;368:404-18.
- [CrossRef] [PubMed] [Google Scholar]
- Association of vasculitic glomerulonephritis with membranous nephropathy: A report of 10 cases. Nephrol Dial Transplant. 1997;12:1017-27.
- [CrossRef] [PubMed] [Google Scholar]
- Membranous glomerulonephritis with ANCA-associated necrotizing and crescentic glomerulonephritis. Clin J Am Soc Nephrol. 2009;4:299-308.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Crescentic transformation in primary membranous glomerulonephritis. Postgrad Med J. 1991;67:574-6.
- [CrossRef] [PubMed] [Google Scholar]
- Acute renal failure in membranous glomerulonephropathy: A result of superimposed crescentic glomerulonephritis. J Am Soc Nephrol. 1995;6:1541-6.
- [CrossRef] [PubMed] [Google Scholar]
- Transformation of membranous glomerulonephritis into crescentic glomerulonephritis with glomerular basement membrane antibodies. Serial determinations of anti-GBM before the transformation. Nephron. 1984;38:134-7.
- [CrossRef] [PubMed] [Google Scholar]
- A case of concurrent MPO-/PR3-negative ANCA-associated glomerulonephritis and membranous glomerulopathy. Case Reports in Nephrology. 2015;2015:316863.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- MPO-ANCA crescentic glomerulonephritis complicated by membranous nephropathy: MPO demonstrated in epimembranous deposits. NDT Plus. 2009;2:461-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinical and histologic determinants of renal outcome in ANCA-associated vasculitis: A prospective analysis of 100 patients with severe renal involvement. J Am Soc Nephrol. 2006;17:2264-74.
- [CrossRef] [PubMed] [Google Scholar]
- Plasma exchange for induction and cyclosporine a for maintenance of remission in Wegener’s granulomatosis--a clinical randomized controlled trial. Nephrol Dial Transplant. 2011;26:206-13.
- [CrossRef] [PubMed] [Google Scholar]
- EUVAS (European Vasculitis Study Group). Pulse versus daily oral cyclophosphamide for induction of remission in antineutrophil cytoplasmic antibody-associated vasculitis: A randomized trial. Ann Intern Med. 2009;150:670-80.
- [CrossRef] [PubMed] [Google Scholar]
- A randomized, controlled trial of steroids and cyclophosphamide in adults with nephrotic syndrome caused by idiopathic membranous nephropathy. J Am Soc Nephrol. 2007;18:1899-904.
- [CrossRef] [PubMed] [Google Scholar]
- European vasculitis study group. rituximab versus cyclophosphamide in ANCA-associated renal vasculitis. N Engl J Med. 2010;363:211-20.
- [CrossRef] [PubMed] [Google Scholar]
- RAVE-ITN research group. rituximab versus cyclophosphamide for ANCA-associated vasculitis. N Engl J Med. 2010;363:221-32.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- European vasculitis society (EUVAS). Rituximab versus cyclophosphamide in ANCA-associated renal vasculitis: 2-year results of a randomised trial. Ann Rheum Dis. 2015;74:1178-82.
- [CrossRef] [PubMed] [Google Scholar]
- French Vasculitis Study Group. Rituximab versus azathioprine for maintenance in ANCA-associated vasculitis. N Engl J Med. 2014;371(19):1771-80.
- [CrossRef] [PubMed] [Google Scholar]







