Translate this page into:
Coronary Angiography Profile at the Time of Hemodialysis Initiation in End-Stage Renal Disease Population: A Retrospective Analysis
Address for correspondence: Dr. S. Raju, Department of Nephrology, Nizams Institute of Medical Sciences, Punjagutta, Hyderabad - 500 082, Telangana, India. E-mail: sreebhushan@hotmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
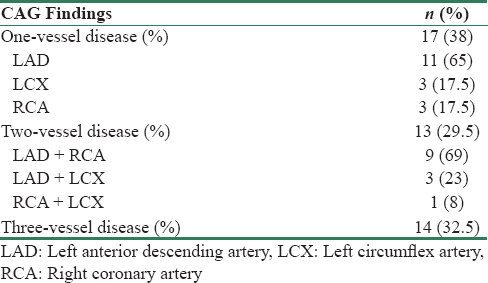
Cardiovascular disease is associated with increased mortality in dialysis population. However, there are very few studies that assessed the prevalence of coronary artery disease (CAD) at the time of initiation of hemodialysis (HD). The present study was aimed to assess the prevalence of CAD in end-stage renal disease (ESRD) patients at the time of initiation of HD and the risk factors for CAD in this population. This was a single-center retrospective study and included ESRD patients who underwent coronary angiography (CAG) at the time of initiation of HD. Inclusion criteria were age >18 years and those who were subjected to CAG within 2 weeks of initiation of HD. According to the findings on CAG, patients were divided into no CAD and CAD groups. CAD was diagnosed if there was >50% stenosis of vessel. Clinical and laboratory parameters between these two groups were analyzed. Ninety-seven patients were included in the study based on the inclusion criteria. Forty-four (45%) patients were diagnosed with CAD. Patients who had CAD were younger compared to no CAD group (50.7 + 10 vs. 55.8 + 9.3 years; P = 0.01). Majority of them were males. Diabetic nephropathy (DN) was associated with increased risk of CAD (60% vs. 40%, P = 0.007). History of smoking, high high-sensitivity C-reactive protein (hs-CRP), low total cholesterol, and low high-density lipoprotein (HDL) were associated with significantly increased risk of CAD. Gender, symptoms of CAD, serum low-density lipoprotein (LDL), very LDL, and triglycerides were not associated with increased risk of CAD. Neither calcium (Ca), phosphorus (PO4), nor Ca × PO4products were associated with an increased risk of CAD. Resting electrocardiogram abnormalities had no significance in predicting CAD (32% in CAD and 19% in no CAD group). Echocardiography showed regional wall motion abnormalities/global hypokinesia in 18% patients of CAD group and 3.8% patients of no CAD group (P = 0.03). Single-, double-, and triple-vessel disease was documented in 17 (38%), 13 (29.5%), and 14 (32.5%) patients, respectively, and the most common vessel involved was the left anterior descending artery. At the initiation of HD in ESRD patients, CAD was seen in almost half of the patients. DN was a significant risk factor for CAD. Other risk factors for CAD include smoking, low cholesterol, low HDL, and high hs-CRP levels.
Keywords
Coronary angiography
end-stage renal disease
initiation of hemodialysis
Introduction
Cardiovascular disease accounts for almost half of the deaths of patients with end-stage renal disease (ESRD).[1234] Causes of cardiovascular mortality in patients with chronic kidney disease (CKD) and ESRD include both nontraditional risk factors such as altered calcium-phosphorus metabolism, inflammation, oxidative stress, as well as traditional risk factors such as hypertension, smoking, diabetes, and dyslipidemia.[5] The overall prevalence of coronary artery disease (CAD) in chronic dialysis patients ranges between 30% and 60% in various studies.[67891011] The gold standard test to diagnose CAD is coronary angiography (CAG), which is invasive. Although, in general population, computerized tomography CAG is a valid noninvasive alternative, especially in low-probability cases, this is not reliable in Stage 5 CKD patients due to altered bone mineral metabolism.
The prevalence of CAD in dialysis patients had been assessed by CAG in various studies. However, all these studies were carried out in chronic hemodialysis (HD) patients; only one study assessed prevalence of CAD at the initiation of HD, but sample size was very small (n = 24).[12] Knowledge about CAD at the initiation of dialysis is important as cardiovascular system (CVS) involvement is the most common cause of death in HD patients and better screening strategies can be employed to decrease CVS-related mortality.
The aim of the present study was to assess the prevalence of CAD in ESRD patients at the initiation of HD and risk factors for CAD in this population.
Materials and Methods
This was a single-center retrospective study to assess the prevalence of CAD in ESRD patients at the initiation of HD and the risk factors for CAD in this population. Medical records of eligible patients who underwent CAG between August 1, 2013, and May 31, 2016, were analyzed. All these patients were essentially covered by insurance and protocol CAG was performed in all these patients at the time of initiation of HD irrespective of the presence or absence of CAD symptoms.
Inclusion criteria were age >18 years and those who were subjected to CAG within 2 weeks of initiation of HD. Exclusion criteria were previous history of CAD, and CAG performed in chronic HD patients. Data regarding age, sex, history of smoking, symptoms of CAD, and diabetic nephropathy (DN) were obtained. Laboratory parameters such as lipid profile, calcium, phosphorous, Ca × PO4 product, high-sensitivity C-reactive protein (hs-CRP), resting electrocardiogram (ECG), and echocardiography were noted. DN was diagnosed when it was biopsy proven or when patient had diabetes mellitus of more than 10-year duration with typical DN clinical picture.
The resting ECG was recorded as abnormal if there was evidence of pathological Q-waves, left ventricular hypertrophy, ST depression or elevation of >1 mm, T-wave inversion, or bundle branch block. Regional wall motion abnormality (RWMA) and global hypokinesia were documented in echocardiography. In CAG, we evaluated the presence or absence of CAD, number of vessels involved among left anterior descending artery (LAD), left circumflex artery (LCX), and right coronary artery (RCA). Stenosis >50% was considered as CAD.
According to the findings on CAG, patients were divided into no CAD and CAD groups. Clinical and laboratory parameters between these two groups were analyzed. The approval of the Institutional Ethics Committee was taken before conducting this study.
Statistical analysis
The clinical characteristics of the patients were presented as mean ± standard deviation for continuous variables and as percentages for categorical variables. Unpaired t-test and Chi-square analyses were performed for continuous and categorical variables, respectively. All statistical tests were two-tailed with P < 0.05 to indicate statistical significance.
Results
A total of 97 patients were included in the final analysis [Table 1]. Of the total 44 (45%) patients who were diagnosed with CAD, majority were male patients, i.e., 36 patients in no CAD group and 27 in CAD group. Patients of CAD group were significantly younger with a mean age 50.7 ± 10 years as compared to 55.8 ± 9.3 years in no CAD group (P = 0.01). Eleven patients in CAD group and 4 patients in no CAD group were smokers and smoking was associated with an increased risk of CAD (P < 0.01). Symptoms of CAD, which includes chest pain associated with dyspnea, nausea, vomiting, and diaphoresis were not different in two groups; 4 and 8 patients in no CAD and CAD patients. A total of 21 (40%) patients in CAD group and 30 (68%) patients in the no CAD group were diabetics (P = 0.007).

Although altered bone mineral metabolism is considered as a nontraditional risk factor for CAD in CKD patients, this was not reflected in our study. Calcium, phosphorous, and Ca × PO4 product were not different significantly between two groups. Low total cholesterol and low high-density lipoprotein (HDL) cholesterol were associated with increased risk of CAD (P = 0.02 and 0.03, respectively), whereas low-density lipoprotein (LDL), very LDL, and triglycerides were not associated with increased CAD risk. Mean hs-CRP was 11.8920.43 and 38.0663.47 mg/l in no CAD and CAD groups, respectively, and it was associated with an increased risk of CAD (P = 0.005). ECG abnormalities were noted in 10 and 14 patients in no CAD and CAD groups, respectively, and ECG changes were not predictive of CAG findings (P = NS). Echocardiography abnormalities in the form of RWMAs or global hypokinesia were documented in 2 and 8 patients in no CAD and CAD groups, respectively (P = 0.03). Overall, CAD was diagnosed in 44 patients. Details of various number and vessels involved is shown in Table 2.
Discussion
The epidemiology of CAD by CAG was studied in chronic dialysis patients by various authors.[67891011] To the best of our knowledge, patients with ESRD were evaluated at the time of initiation of HD in one study published by Joki et al. in 1997.[12] However, the sample size in this study was small (n = 24) and about 50% of patients had chest symptoms suspicious of CAD.
In the present study, the mean age of CAD group was statistically younger than no CAD group, whereas in the study published by Joki et al., age was not significantly differed between two groups.[12] The reason for this difference was not clear, but in Joki et al. study, smoking and diabetes were not differed significantly between two groups, whereas in our study smoking, diabetes and hs-CRP levels were significantly higher in CAD group. Whether age itself or other traditional and nontraditional risk factors in this group contributed to CAD should be tested with larger sample size and by regression analysis in further studies.
In the present study, <20% of the patients had CAD symptoms, and the presence or absence of CAD symptoms is not predictive of CAG findings. This finding is consistent with various studies, in which, compared with the general population, ESRD patients are less likely to have typical CAD symptoms.[1314151617] Almost half of the patients initiated on HD were diagnosed with CAD in the present study, and hence, screening for CAD should be done in all the patients at the time of initiation of HD. However, performing CAG for all patients, especially in asymptomatic patients, is not practical, and hence, some sort of noninvasive method should be considered. Unfortunately, noninvasive methods such as resting ECG, exercise ECG, and pharmacological stress tests are not good predictors of CAD in this special population. Although echocardiography finding of RWMA/global hypokinesia achieved statistical significance between the groups in the present study, only 18% of patients in CAD group had positive findings, which mean that it has a poor correlation. Hence, a reasonable noninvasive alternative is a long-standing due, and at this time, reasonable noninvasive method to screen for CAD would be dobutamine stress echocardiography which has sensitivity and specificity of 75% in dialysis population, though unfortunately, this was not done in the present study population.[18]
In our study, smoking was significantly associated with an increased risk of CAD and it could be due to the endothelial dysfunction induced by smoking. Increased incidence of cardiac disease due to smoking in HD patients was earlier reported by Di Benedetto et al. and Shah et al.[1920]
DN is associated with an increased risk of CAD as in the general population, and in the present study, 68% of the patients of CAD group patients were diabetics. In the study by Joki et al., 73% of the patients were diabetics and 44% of the patients were diabetics in the study conducted by Sharma et al.[1218]
Low total cholesterol and low HDL cholesterol were associated with an increased risk of CAD. Lower rather than higher cholesterol was significant risk factor for CAD in this population. Malnutrition-induced inflammation which leads to subsequent atherogenesis could be the possible explanation.[21] Traditionally, hs-CRP is considered as a significant risk factor for CAD in the general population. It is also associated with an increased mortality in the dialysis patients when serum hs-CRP level is >3 mg/l.[22] In the present study, the mean hs-CRP level was significantly higher in CAD group and consistent with the earlier literature.
Kidney Disease Outcomes Quality Initiative guidelines recommend that the calcium-phosphate product be maintained below 55 mg/dl2 in dialysis patients to prevent vascular calcification, atherosclerosis, and other bone mineral-related diseases. In the present study, calcium, phosphorous, and mean Ca × PO4 product in both the groups were in normal range and were not significantly different; better calcium, phosphorous, and Ca × PO4 product could be due to the use of noncalcium-containing phosphate binder as cost was not a limiting factor for these insured patients. We did not analyze the role of parathyroid hormone (PTH).
Important limitations of our study were that it was a retrospective analysis and that the present cohort may not reflect the general CKD population as all of them were insured population. Prospective studies involving larger sample size, which represent overall CKD population are needed. The present study only looked at prevalence of CAD and its risk factors at initiation of HD; follow-up data about treatment they received and survival was not analyzed which should be addressed in future studies.
Conclusion
At the initiation of dialysis in ESRD patients, CAD was seen in almost half of the patients. DN was a significant risk factor for CAD. Other risk factors for CAD include smoking, low cholesterol, low HDL levels, and high hs-CRP levels.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- A prospective comparison of methods for determining if cardiovascular disease is a predictor of mortality in dialysis patients. Am J Kidney Dis. 1994;23:382-8.
- [Google Scholar]
- The clinical epidemiology of cardiac disease in chronic renal failure. J Am Soc Nephrol. 1999;10:1606-15.
- [Google Scholar]
- Kidney disease as a risk factor for development of cardiovascular disease: A statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation. 2003;108:2154-69.
- [Google Scholar]
- Cardiac diseases in maintenance hemodialysis patients: Results of the HEMO study. Kidney Int. 2004;65:2380-9.
- [Google Scholar]
- Premature cardiovascular disease in chronic renal failure. Lancet. 2000;356:147-52.
- [Google Scholar]
- Dialysis-associated ischemic heart disease: Insights from coronary angiography. Kidney Int. 1984;25:653-9.
- [Google Scholar]
- Coronary angiography is the best predictor of events in renal transplant candidates compared with noninvasive testing. Hypertension. 2003;42:263-8.
- [Google Scholar]
- Cardiovascular risk evaluation before kidney transplantation. J Am Soc Nephrol. 2005;16:843-5.
- [Google Scholar]
- High prevalence of occult coronary artery stenosis in patients with chronic kidney disease at the initiation of renal replacement therapy: An angiographic examination. J Am Soc Nephrol. 2005;16:1141-8.
- [Google Scholar]
- Coronary artery disease in uremia: Etiology, diagnosis, and therapy. Kidney Int. 2001;60:2059-78.
- [Google Scholar]
- Diabetes and coronary artery disease impose similar cardiovascular morbidity and mortality on renal transplant candidates. Nephrol Dial Transplant. 2007;22:1456-61.
- [Google Scholar]
- Onset of coronary artery disease prior to initiation of haemodialysis in patients with end-stage renal disease. Nephrol Dial Transplant. 1997;12:718-23.
- [Google Scholar]
- How to manage the renal patient with coronary heart disease: The agony and the ecstasy of opinion-based medicine. J Am Soc Nephrol. 2003;14:2556-72.
- [Google Scholar]
- Clinical characteristics of dialysis patients with acute myocardial infarction in the United States: A collaborative project of the United States Renal Data System and the National Registry of Myocardial Infarction. Circulation. 2007;116:1465-72.
- [Google Scholar]
- Renal failure and acute myocardial infarction: Clinical characteristics in patients with advanced chronic kidney disease, on dialysis, and without chronic kidney disease. A collaborative project of the United States Renal Data System/National Institutes of Health and the National Registry of Myocardial Infarction. Am Heart J. 2012;163:399-406.
- [Google Scholar]
- Use of evidence-based therapies in short-term outcomes of ST-segment elevation myocardial infarction and non-ST-segment elevation myocardial infarction in patients with chronic kidney disease: A report from the National Cardiovascular Data Acute Coronary Treatment and Intervention Outcomes Network Registry. Circulation. 2010;121:357-65.
- [Google Scholar]
- Relation between renal function, presentation, use of therapies and in-hospital complications in acute coronary syndrome: Data from the SWEDEHEART register. J Intern Med. 2010;268:40-9.
- [Google Scholar]
- Dobutamine stress echocardiography and the resting but not exercise electrocardiograph predict severe coronary artery disease in renal transplant candidates. Nephrol Dial Transplant. 2005;20:2207-14.
- [Google Scholar]
- Risk factors and underlying cardiovascular diseases in incident ESRD patients. J Nephrol. 2005;18:592-8.
- [Google Scholar]
- Are traditional risk factors valid for assessing cardiovascular risk in end-stage renal failure patients? Nephrology (Carlton). 2008;13:667-71.
- [Google Scholar]
- Are there two types of malnutrition in chronic renal failure? Evidence for relationships between malnutrition, inflammation and atherosclerosis (MIA syndrome) Nephrol Dial Transplant. 2000;15:953-60.
- [Google Scholar]
- Usefulness of clinical evaluation, troponins, and C-reactive protein in predicting mortality among stable hemodialysis patients. Am J Cardiol. 2006;98:1283-7.
- [Google Scholar]







