Translate this page into:
Current Status and Future of Artificial Kidney in Humans
Address for correspondence: Dr. Nitin K. Bajpai, Department of Nephrology, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India. E-mail: drnitinbajpai@gmail. com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The number of patients needing renal replacement therapy (RRT) is increasing rapidly with an increase in lifestyle diseases such as diabetes, hypertension, and metabolic syndrome. Kidney transplantation, whenever feasible, is the most preferred mode of RRT. However, there is a growing shortage of donor kidneys for transplantation. While dialysis is partially able to perform the filtration and excretion function of the kidneys, it is still not able to perform the other renal tubular and endocrine functions of a normal kidney and has quality-of-life issues with significant long-term morbidity. The need of the hour is to develop an ideal artificial kidney that would be wearable or implantable and would be able to perform the complete excretory, filtration, tubular, endocrine, and metabolic functions of the kidney while preserving the quality of life and minimizing complications. In this review, we discuss the characteristics of an ideal artificial kidney, the challenges of developing such a device, a brief description of the past and current work on this topic, and what the artificial kidney of the future should look like.
Keywords
Artificial kidney
bioartificial kidney
end-stage renal disease
renal replacement therapy
wearable kidney
"We grow what we can't engineer, we engineer what we can't grow."
Need for an Artificial Kidney
From 1990 onwards, the prevalence of patients needing renal replacement therapy (RRT) has doubled and is expected to rise even further.[12] With an increase in lifestyle diseases such as diabetes, hypertension, and metabolic syndrome and a growing proportion of the elderly in the general population, the shortage of donor kidneys for transplantation is only going to worsen.[3] Dialysis is partially able to perform the excretory and filtration functions of the kidney and correct electrolyte and fluid imbalances, predominantly by diffusion, but does not perform the other renal tubular functions, namely the endocrine, secretory, and metabolic functions. Even the filtration function is far from being selective and complete, and protein-bound uremic toxins (PBUT) and other larger molecules are retained due to the limited pore size. The discontinuous mode of treatment (2–3 sessions of 4 h every week) leads to inter-dialytic accumulation of fluids, electrolytes, and toxins, which are then rapidly recalibrated toward normal during dialysis, leading to large scale shifts, in glaring contrast to the homoeostasis maintained by normal kidneys. This cyclical insult has been postulated to be one of the major causes of cardiovascular (CVS) morbidity seen in such patients.[45]
Hemodialysis (HD) even when done regularly at a dialysis center, leads to patient fatigue, poor sleep, and travel- and time-related difficulties.[6] Less dialysis time is associated with hyperphosphatemia and malnutrition, which are important causes of CVS morbidity and lower survival in this group of patients.[78] Home dialysis helps in overcoming some of the above mentioned problems by providing a more personalized schedule, with longer and more frequent dialysis times with reduced fluid and dietary restrictions and an overall better quality of life, in addition to benefits seen in episodes of hypotension, left ventricular hypertrophy, and malnutrition.[9] However, even the most advanced equipment for home dialysis is bulky, with requirement of trained staff for operation, leading to low acceptance by the patients.[10] Peritoneal dialysis (PD) at home, either manually or automated (APD), has a high incidence of attendant complications, poor clinical outcomes, and quality of life.[11] These observations have continued to fuel the search for a real artificial kidney (AK) that would closely replicate the physiological process of the normal human kidney.
Characteristics of an Ideal Artificial Kidney
Nissenson proposed a patient-focused quality hierarchy ("quality pyramid") according to which the ultimate goal of RRT should be focused on improving the quality of life [Figure 1].[12] Theoretically, only a bio-engineered kidney identical to the normal, human kidney can fulfill all the criteria. An ideal mechanically engineered AK should have the following characteristics:

- Patient-focused quality pyramid. HR-QOL – Health-related quality of life, DM – Diabetes mellitus, MBD – Mineral and bone disorders, EOL – End of life, CVD – Cardiovascular diseases, CVC – Central venous catheters, AVF – Arterio-venous fistulae, mgmt. – Management, PTH – Parathyroid hormone, URR – Urea reduction ratio
-
Size: The device should be small enough to be wearable or implantable. The aim is to provide ambulatory dialysis. It should be ergonomic, should fit under clothes or be unobtrusive on the patient's outfit, and must be of manageable size and weight.
-
Vascular access: The vascular access of the AK should preferably be a subcutaneously implanted; needleless venous catheter (CVCs) resistant to displacement and dislodgement; resistant to thrombosis and obstruction by either stagnation of blood, deposition of fibrin, or blood proteins; and resistant to infection by biofilm formation.
-
Dialysis membrane: Dialysis membranes must be thromboresistant to prevent clotting, should exhibit hydraulic permeability and molecular selectivity, should not absorb and accumulate proteins, and should be biocompatible and durable when exposed to blood. The membrane must be able to function even under low pressures generated just by the pumping action of the heart and the wall tension of the blood vessels.
-
Integration of convective dialysis therapies: The ideal AK should also use convective therapies such as high flux hemodialysis, hemofiltration, or hemodiafiltration to achieve greater clearance of middle molecules and phosphate, which are often not cleared by conventional diffusion-based hemodialysis.
-
Blood pump and power source: In addition to being small, the blood pump should generate optimum force for propulsion of blood, enough to generate a pressure gradient to pass through the nanopore dialysis membrane but not so high as to cause hemolysis. The pump should be quiet, with low power consumption and heat generation. The ideal pump will be one that will just augment the flow generated by the pumping action of the heart. The power source should be small and quiet, with high energy generation and power storage capacity. It should preferably be self-recharging akin to the batteries of mechanical powered wristwatches that are charged by wrist movements of the wearer or by light exposure. Also, the energy source itself should not generate waste.
-
Dialyzer fluid characteristics, regeneration, and storage: For an ambulatory device, dialysate fluid should be low volume with an inbuilt circuit for dialysate regeneration.
-
Patient monitoring and troubleshooting: The monitoring system should be attuned to detect needle dislodgements, power failures, circuit blockages, presence of bubbles in the circuit or overall equipment failure by means of appropriate alarms to alert the patient or caregivers in his/her family. The vascular access device should be such that it can be rapidly and easily closed before blood loss occurs. The steps to be followed in case of device failure and the steps to clear the circuit of blockages and bubbles should be easy to understand and follow.
-
Lifespan: The lifespan of the device should be such that it should not need frequent replacements in case of an implantable device.
-
Endocrine functions: The device should supplement the endocrine functions of the native kidney, such as secretion of erythropoietin, by means of a refillable depot releasing the hormone directly into the bloodstream.
-
Cost and availability: Production and running costs should be sustainable, and it should be widely available.
-
Compatibility with imaging modalities: It should be compatible with magnetic resonance imaging.
Challenges in the Evolution of Artificial Kidney
The roadmap to the development of the ultimate AK is shown in Figure 2. The driving force on this road has been the quest for miniaturization and the greater use of bio-engineering to ultimately produce a human renal tubular cell-based AK. The goals in the development of an ideal AK have been outlined in the preceding section. The challenge is to achieve those goals. Thefirst challenge is the miniaturization of the dialysis machine. Conventional HD machines have polymer hollow fiber membranes that are 30–100 μm with non-uniform pore sizes, which limits both their hydraulic permeability and molecular selectivity.[13] Research in the field of nanotechnology has led to the use of more selective and permeable silicon nitride nanopore membranes (SNM), which have precisely cut out, uniformly sized, parallel slit-shaped pores all in a thickness of 0.1–1.0 μm, while the atomically thin graphene membranes promise even greater permeability and selectivity.[1415] The durability and biocompatibility on exposure to blood are still to be determined. Efficient water utilization is the next big challenge. In conventional HD, stationary, high maintenance water treatment plants with specific plumbing and electricity requirements generate approximately 120 L of dialysate over a 4-h session.[16] To overcome this, portable dialysis machines have to make use of a closed-loop system in which a small volume of dialysate can be circulated and purified each time for reuse within the circuit by using sorbent and enzyme technologies.[17] Phosphate and potassium are removed by ion exchangers and organic wastes such as creatinine and middle molecules by activated carbon.[18]
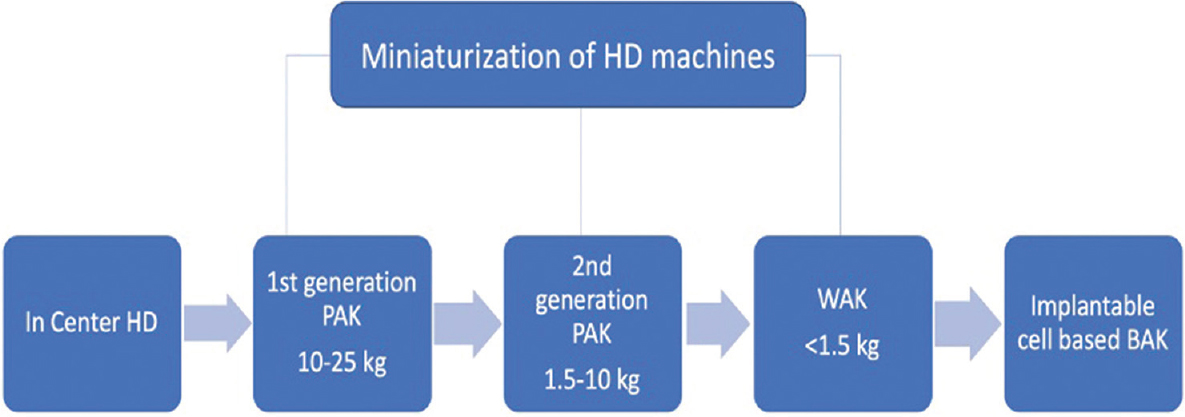
- Roadmap to development of artificial kidney. HD – Hemodialysis, PAK – Portable artificial kidney, WAK – Wearable artificial kidney, BAK – Bioartificial kidney
The removal of urea poses a bigger challenge because of its hydrophilic nature and low reactivity. Some of the available and experimental methods are
-
Use of a redesigned REcirculating DialYsis (REDY) sorbent system by using the enzyme urease to break down urea into ammonium and carbonate, once widely used but withdrawn due to aluminum toxicity, low flow rates, reports of osteomalacia, and cost ineffectiveness.[1920212223] While the risk of aluminum toxicity has been eliminated, there are persistent issues with excess ammonium generation; excess loss of calcium, potassium, and magnesium; and release of sodium by the cation exchanger.
-
Use of a large amount of activated carbon (2–5 kg) to take care of the daily urea production.[24]
-
Electrochemical degradation to carbon dioxide and nitrogen gas.[25]
-
Adsorption by zeolites, resins, silica, and chitosan.[26]
-
A new class of two-dimensional transition metal nitrides and carbides (mainly titanium carbide) comprising only a few atomic layers of transition metals interleaved with carbon or nitrogen, called MXenes, promises to be an efficient adsorbent for urea removal without any cytotoxicity.[2728]
Appropriate vascular access for ambulatory dialysis is of paramount importance. Needle-based access through fistulae, grafts, or central venous catheters (CVCs) carries the risk of infection, dislodgement, disconnection, infection, and thrombosis. Venous pressures may not show a large change with disconnection, and there can be life-threatening hemorrhage within minutes.[29] Subcutaneously implantable devices such as Lifesite Hemodialysis Access System and Dialock Hemodialysis Access System, which are cuff-less devices, have attempted to overcome this problem.[30] Hemaport was a percutaneously placed polytetrafluoroethylene graft that attempted to provide needleless access.[31] All the above mentioned devices were plagued by surgical site complications. More recent efforts have focused on the use of single-needle cannulation to minimize blood loss in case of dislodgement. Development of macromolecules (Endexo technology) that coat the inner and outer surface of CVCs can make them resistant to thrombosis and biofilm formation.[32] An integrated patient monitoring system that detects complications of vascular access, tubing, and clinical parameters of the patients using the device and communicates with a remotely located nephrologist or paramedical staff for monitoring via wireless connection networks is the future. One of the promising forerunners for such a system is the Tablo platform from Outset Medicals.[33]
Review of Past and Current Work on Artificial Kidney
The concept of a wearable dialysis machine for ambulatory dialysis has been around since the 1960s.[34] They use patient-generated pulses such as arterial and breathing pulses or forearm-mounted reservoirs to create a pressure gradient and drive the flow of blood and dialysate.[3536] Willem Kolff was thefirst to develop a wearable AK (WAK) weighing 3.5 kg.[37] The latest WAK, developed by Victor Gura et al., is a 5-kg device, worn like a belt, that connects to the vasculature via catheters and performs sorbent-based dialysis.[38] The modified REDY sorbent system is used along with a reactor bed containing urease, zirconium phosphate, hydrous zirconium oxide, and activated charcoal [ Figure 3]. The approximate total volume of the blood circuit is 65 ml and that of the dialysate circuit is 375 ml. Due to device-related issues, the trial testing this device in patients was stopped. A newer version of WAK, termed WAK 3.0, weighing only 1 kg is under development. The other devices under development are listed in Table 1. Miniaturized devices for peritoneal dialysis have also been developed and are currently awaiting clinical trials [Table 2].
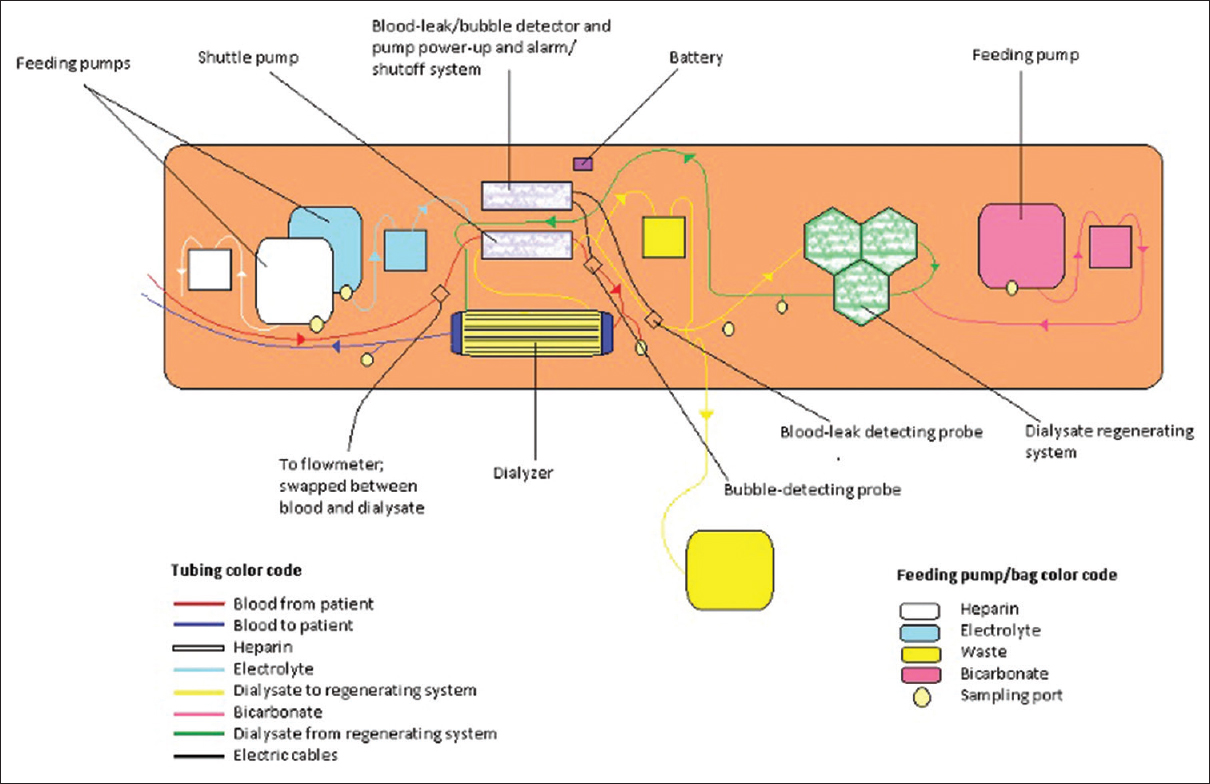
- Schematic representation of WAK
| Name | Weight | Key features | Issues | Status |
|---|---|---|---|---|
| The WAK™ | 5 kg (including dialysate) | Wearable device, REDY sorbent system, uses tunneled double-lumen CVC. Higher time adjusted clearance by 24-h continuous treatment/day compared to conventional HD. Preset ultrafiltrate volume achieved. Greater overall patient satisfaction. | Device related problems like excessive carbon dioxide bubbles in circuit and variable flow. | Newer version under development |
| Neokidney PAK[18] | 10 kg +6 l dialysate | Planned for alternate day 4-h dialysis. Portable. | - | Planned for human clinical trials |
| EasyDial PAK (Dharma™)[18] | 6.2 kg +3.7 l dialysate | Portable, uses a REDY sorbent system | Sodium release in exchange for ammonium adsorption by zirconium phosphate | Not yet approved for clinical trials |
| Medtronic PAK[18] | REDY sorbent system | Unknown | ||
| Possible regeneration of sorbent cartridges | ||||
| Fresenius PAK[18] | 30 kg | REDY sorbent system | Heavy | Unknown |
WAK – Wearable artificial kidney, PAK – Portable artificial kidney, REDY – Recirculating Dialysis, CVC – Central venous catheter
| Name | Weight | Status |
|---|---|---|
| CLS PD[18] | <3 kg with 2.5-3.0 L PD fluid | Recruiting in 1st human trail |
| AWAK PD[18] | <2 kg +2 L PD fluid | Awaiting clinical trial |
| WEAKID[18] | ~1.5 kg +dialysate (during night) + 2 L PD fluid | Awaiting clinical trial |
| ViWAK PD[18] | Weight: Unknown +2 L PD fluid | Device not finalized |
PD – Peritoneal dialysis, AWAK PD - Automated wearable artificial kidney for peritoneal dialysis, CLS PD - Cary Life System for peritoneal dialysis, WEAKID - WEarable Artificial KIDney, ViWAK - Vicenza Wearable Artificial Kidney
Developing a Bioartificial Kidney (BAK)
A bioengineered kidney would be implanted inside or on the human body and would do away with an external mechanical appendage in the best-case scenario. It would work continuously in providing clearance of fluids and solutes without the need for thrice weekly or daily connection to machines, eliminating associated complications such as infection, access complications, and diminished quality of life. A cell-based kidney would take over the endocrine and metabolic functions of the normal kidney and produce erythropoietin, vitamin D, renin, etc., thus reducing the need for injectable therapy and providing freedom from dietary constraints and better control of blood pressure and bone metabolism. It could act as a bridge therapy to kidney transplant by supplementing the residual renal function or even replace kidney transplant altogether.
To achieve this requires a complex interplay of advances in tissue engineering [Figure 4]. Attempts span from successful transplantation in animals to various phases of clinical trials:
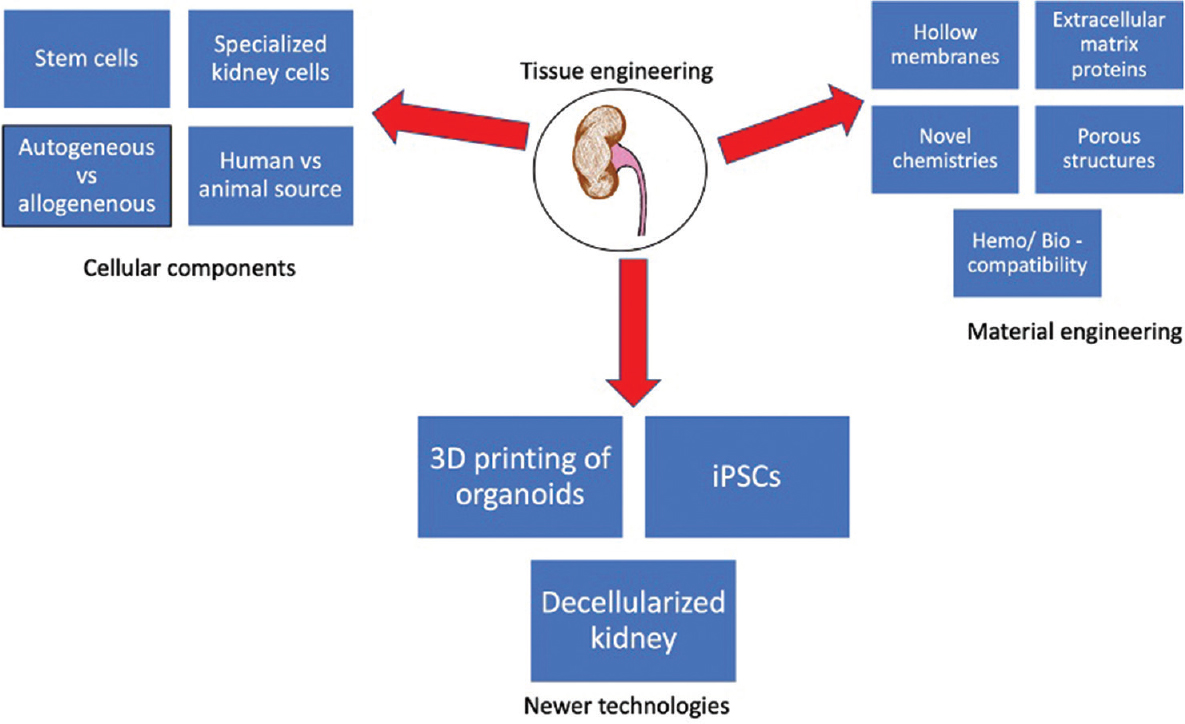
- Key features of the development of bioartificial kidney. iPSCs – Induce pluripotent stem cells
-
Growing a kidney in situ: De novo organogenesis: Metanephroi have been harvested from embryos and transplanted into the omentum of mice where they get vascularized by host kidneys and exhibit glomerular filtration, secretion of vitamin D, and erythropoietin after development.[3940] This is limited to animal studies as of now and shows promising results.
-
Supplementing a failing kidney: Cell transplantation: Fetal renal cells have been transplanted into the kidneys and onto polyglycolic acid polymer scaffolds in the omentum and abdomen and have been found to differentiate into mature renal cells capable of filtration and tubular function.[4142] Choosing the correct timing of gestation to harvest is these cells from the fetus is important to prevent dedifferentiation and formation of other organ systems.
-
Growing a kidney in vitro: Autologous adult stem cells have been injected into the nephrogenic regions of developing embryos so that they get the stimulus of appropriate molecular signaling and developmental milieu.[43] In addition, nuclear transplantation has been used to create cloned renal tissue using bovine fibroblasts on polycarbonate models.[44]
-
Reseeding decellularized kidney scaffold with iPSCs: This technique has been applied in rats and porcine models to create viable cellularized renal moieties that can then be orthotopically transplanted.[45] This process has been tried with variable success on human kidneys too. Further work in achieving upscaling of cell seeding and organ culture to achieve clinical viability.
-
Bio-engineering a kidney: Humes et al.[46] developed thefirst renal assist device (RAD) that consisted of primary renal cells seeded onto the hollow fibers of a standard hemofilter. This is the only BAK device tested in humans and inspired the development of the bioartificial renal epithelial cell system (BRECS) and implantable RAD (iRAD). BRECS attempted to overcome the problem of a reliable source of cells.[47] It is thefirst cryo-preservable, on-demand, cell therapy delivery system. It uses renal progenitor cells maintained on high-density porous disks that are cryopreserved and reconstituted 1–3 months later to provide cells that perform kidney-specific functions. These cells can then be seeded onto the fibers of a hemofilter. At present, preclinical trials for both acute and chronic kidney disease are being designed.
Challenges in Developing BAK
The majority of the above-mentioned techniques use stem cells. Being able to differentiate them into the correct phenotype is a major challenge. Implantation of these cells into embryos helps to overcome such problems to some extent, but using human cells in human embryos raises serious ethical concerns. Even then, the creation of a single urinary tract, appropriate vascularization of these organoids for transplantation, and a friendly pelvicalyceal system are formidable hurdles. A reliable source of these progenitor cells on a large scale along with their storage, cryopreservation, and distribution are also hurdles to sort out. Decellularization of human kidneys to produce extracellular matrix scaffolds has been demonstrated.[48] The next step would be to demonstrate the seeding of these scaffolds. However, issues such as the sterilization of such scaffolds and immune reactions to the extracellular matrix needed to be taken care of. The source of human kidneys for such a process also needs to be looked into. While BRECS has already been tested in large animals, designing an RCT in humans faces the challenge of maintaining an extracorporeal circuit of blood flow using a HD machine, along with its attendant complications.[49]
A Look at the Future of BAK
-
Implantable Renal Assist Device (iRAD): The team of Dr. Shuvo Roy at the University of California, San Francisco and Vanderbilt University Medical Center has taken upon the task of developing thefirst bioengineered implantable AK [Figure 5][50] that uses a microelectromechanical system (MEMS) with a hemofilter made of silicon nanopore membrane (SNM) with a renal tubule cell bioreactor, such as the BRECS, with immune-isolation properties.[51] This device would be implanted in the iliac fossa and anastomosed to the iliac vessels for blood flow and to the bladder or ureter. The greater permeability and selectivity of the SNM would let it function at pressures generated by the arterio-venous pressure difference alone, thus eliminating the need for additional pumps or immune-suppressants. Due to the use of MEMS, the total surface area of the device would be 0.1 m2. A small pilot study in dogs showed that the hemofilter remained unclotted, while the silicon membranes remained intact, without albumin leakage, for a period of 8 days.[13] The feasibility of this strategy in humans was tested by seeding a SNM with human renal cortical epithelial cells, which went on to develop tight junctions and cilia.[52] This paves the way for use in human trials. The biggest challenge for this device would be to minimize loss of macromolecules and to produce adequate ultrafiltrate for clinically relevant clearance of small, water-soluble, uremic toxins, followed by its reabsorption.[18] At present, thefirst human trial is being designed.[53]
-
Bioengineered living membranes: Human conditionally immortalized PTEC (ciPTEC) have been developed, which are enriched in influx and efflux transporters.[54] These cells when cultured on hollow tubes of hemofilter in the presence of albumin demonstrated clearance of PBUTs. Attempts to miniaturize such membranes may enhance the capabilities of standard and wearable HD devices.
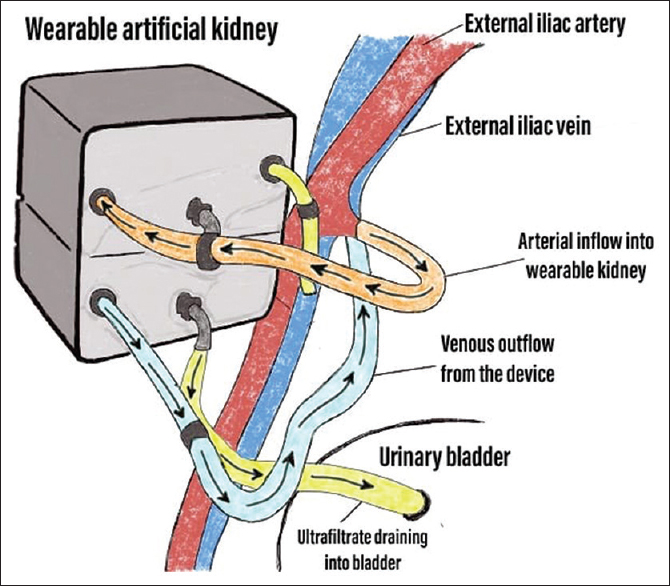
- The proposed model of the iRAD seen after implantation in the human right iliac fossa
Conclusion: 5-Year View of Artificial Kidney
The iRAD would be thefirst device for human clinical trials. Tissue-driven approaches continue to make strides in replicating the complex structure of the human kidney. Further studies should focus on (1) membrane characteristics: material type, porosity, additional coatings or modifications, and sieving coefficient; (2) cell characteristics: source, phenotype, genetic modification, passage number, culture conditions, and storage; and (3) renal functional aspects: active PBUT excretion, ion transport, vitamin D activation, immunogenic effect, and nutrient reabsorption capacity. The ultimate aim is to produce a dialysate-free, implantable, autonomous BAK.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Maintenance dialysis throughout the world in years 1990 and 2010. J Am Soc Nephrol. 2015;26:2621-33.
- [Google Scholar]
- Worldwide access to treatment for end-stage kidney disease: A systematic review. Lancet. 2015;385:1975-82.
- [Google Scholar]
- What are the key challenges we face in kidney transplantation today? Transplant Res. 2013;2(1):S1.
- [Google Scholar]
- Nontraditional risk factors for cardiovascular disease in patients with chronic kidney disease. Nat Clin Pract Nephrol. 2008;4:672-81.
- [Google Scholar]
- Kidney disease as a risk factor for development of cardiovascular disease: A statement from the American heart association councils on kidney in cardiovascular disease, high blood pressure research, clinical cardiology, and epidemiology and prevention. Circulation. 2003;108:2154-69.
- [Google Scholar]
- Patient and caregiver priorities for outcomes in hemodialysis: An international nominal group technique study. Am J Kidney Dis. 2016;68:444-54.
- [Google Scholar]
- Hyperphosphatemia: A novel risk factor for mortality in chronic kidney disease. Ann Transl Med. 2019;7:55.
- [Google Scholar]
- A systematic review of the effect of nocturnal hemodialysis on blood pressure, left ventricular hypertrophy, anemia, mineral metabolism, and health-related quality of life. Kidney Int. 2005;67:1500-8.
- [Google Scholar]
- United States Renal Data System: 2018 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States, Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases 2018
- Peritoneal dialysis in the US: Evaluation of outcomes in contemporary cohorts. Kidney Int (l):S21-6.
- [Google Scholar]
- Improving outcomes for ESRD patients: Shifting the quality paradigm. Clin J Am Soc Nephrol. 2014;9:430-4.
- [Google Scholar]
- First implantation of silicon nanopore membrane hemofilters. ASAIO J. 2016;62:491-5.
- [Google Scholar]
- An intravascular bioartificial pancreas device (iBAP) with Silicon nanopore membranes (SNM) for islet encapsulation under convective mass transport. Lab Chip. 2017;17:1778-92.
- [Google Scholar]
- Nanoporous atomically thin graphene membranes for desalting and dialysis applications. Adv Mater. 2017;29:1700277.
- [Google Scholar]
- Reusing and recycling dialysis reverse osmosis system reject water. Kidney Int. 2015;88:653-7.
- [Google Scholar]
- Creating a wearable artificial kidney: Where are we now? Expert Rev Med Devices. 2015;12:373-6.
- [Google Scholar]
- From portable dialysis to a bioengineered kidney. Expert Rev Med Devices. 2018;15:323-36.
- [Google Scholar]
- Applications of the Redy sorbent system to hemodialysis and peritoneal dialysis. Artif Organs. 1979;3:230-6.
- [Google Scholar]
- Dialysis fracturing osteomalacia without hyperparathyroidism in patients treated with HCO3 rinsed Redy cartridge. ASAIO J. 1981;27:634-8.
- [Google Scholar]
- Aluminum related dialysis osteomalacia and dementia after prolonged use of the REDY cartridge. ASAIO J. 1981;27:629-33.
- [Google Scholar]
- Aluminium release from the sorbsystem D-3160 and D-3260 cartridges. Life Support Syst. 1986;4:211-9.
- [Google Scholar]
- Portable/Wearable artificial kidney (WAK)-initial evaluation. Proc Eur Dial Transplant Assoc. 1976;12:511-8.
- [Google Scholar]
- Removal of urea in a wearable dialysis device: A reappraisal of electro-oxidation. Artif Organs. 2014;38:998-1006.
- [Google Scholar]
- MXene sorbents for removal of urea from dialysate: A step toward the wearable artificial kidney. ACS Nano. 2018;12:10518-28.
- [Google Scholar]
- Complexity of intercalation in MXenes: Destabilization of urea by two-dimensional titanium carbide. J Am Chem Soc. 2018;140:10305-14.
- [Google Scholar]
- Wearable artificial kidney and wearable ultrafiltration device vascular access—Future directions. Clin Kidney J. 2019;12:300-7.
- [Google Scholar]
- Preliminary results from the use of new vascular access (Hemaport) for hemodialysis. Hemodial Int. 2003;7:73-104.
- [Google Scholar]
- Results of human factors testing in a novel Hemodialysis system designed for ease of patient use. Hemodial Int. 2016;20:643-9.
- [Google Scholar]
- inventor; Applied Biological Sciences Laboratory Inc, assignee. Wearable dialysis apparatus. United States patent US 3,388,803. 1968;18
- [Google Scholar]
- The artificial kidney and its effect on the development of other artificial organs. Nat Med. 2002;8:1063-5.
- [Google Scholar]
- A wearable haemodialysis device for patients with end-stage renal failure: A pilot study. Lancet. 2007;370:2005-10.
- [Google Scholar]
- Transplantation of developing metanephroi into adult rats. Kidney Int. 1998;54:27-37.
- [Google Scholar]
- Transplantation of metanephroi to sites within the abdominal cavity. Transplant Proc. 2005;37:194-7.
- [Google Scholar]
- Improvement of kidney failure with fetal kidney precursor cell transplantation. Transplantation. 2007;83:1249-58.
- [Google Scholar]
- Complete spinal cord injury treatment using autologous bone marrow cell transplantation and bone marrow stimulation with granulocyte macrophage-colony stimulating factor: Phase I/II clinical trial. Stem Cells. 2007;25:2066-73.
- [Google Scholar]
- Human mesenchymal stem cells in rodent whole-embryo culture are reprogrammed to contribute to kidney tissues. Proc Natl Acad Sci U S A. 2005;102:3296-300.
- [Google Scholar]
- Generation of histocompatible tissues using nuclear transplantation. Nat Biotechnol. 2002;20:689-96.
- [Google Scholar]
- Regeneration and experimental orthotopic transplantation of a bioengineered kidney. Nat Med. 2013;19:646-51.
- [Google Scholar]
- Replacement of renal function with a tissue engineered kidney in uremic animals. Nat Biotechnol. 1999;17:451-5.
- [Google Scholar]
- Bioartificial renal epithelial cell system (BRECS): A compact, cryopreservable extracorporeal renal replacement device. Cell Med. 2012;4:33-44.
- [Google Scholar]
- Current strategies and challenges in engineering a bioartificial kidney. Front Biosci (Elite Ed). 2015;7:215-28.
- [Google Scholar]
- A bio-artificial renal epithelial cell system conveys survival advantage in a porcine model of septic shock. J Tissue Eng Regen Med. 2017;11:649-57.
- [Google Scholar]
- Achieving more frequent and longer dialysis for the majority: Wearable dialysis and implantable artificial kidney devices. Kidney Int. 2013;84:256-64.
- [Google Scholar]
- Innovations in wearable and implantable artificial kidneys. Am J Kidney Dis. 2018;72:745-51.
- [Google Scholar]
- Differentiated growth of human renal tubule cells on thin-film and nanostructured materials. ASAIO J. 2006;52:221-7.
- [Google Scholar]
- Ambulatory hemodialysis-technology landscape and potential for patient-centered treatment. Clin J Am Soc Nephrol. 2020;15:152-9.
- [Google Scholar]
- Novel conditionally immortalized human proximal tubule cell line expressing functional influx and efflux transporters. Cell Tissue Res. 2010;339:449-57.
- [Google Scholar]







