Translate this page into:
Depression, insomnia and sleep apnea in patients on maintenance hemodialysis
Address for correspondence: Dr. Tarun Rustagi, F 5/5 Krishan Nagar, Delhi-110051, India. E-mail: drtarun05@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Depression and sleep disorders are more frequent in patients on maintenance hemodialysis (HD) than the general population, and are associated with reduced quality of life and increased mortality risk. The purpose of this study was to assess the prevalence of depression, sleep apnea, insomnia in patients on HD as well as depression in their primary caregiver and to correlate these with the demographic profile. A cross-sectional study was conducted among 69 patients on maintenance HD for more than 3 months. There was high p revalence of depression (47.8%), insomnia (60.9%), increased risk of sleep apnea (24.6%) and depression in caregiver (31.9%). Depression was significantly more in patients with low monthly income (P=0.03), those on dialysis for more than 1 year (P=0.001) and the unemployed (P=0.009). High-risk patients for sleep apnea tended to be males with low monthly income (P=0.02). Insomnia was significantly higher in patients who were on dialysis for more than 1 year (P=0.003).
Keywords
End-stage renal disease
depression
hemodialysis
insomnia
sleep apnea
Introduction
Hemodialysis (HD) is a life sustaining treatment for patients with ESRD. It has revolutionized the treatment of end-stage renal disease (ESRD) and allowed patients with this disease throughout the world to survive longer. There has been a progressive increase in both the incidence and prevalence of patients with ESRD throughout the world.[1] Patients on HD are thought to be highly susceptible to emotional problems because of the chronic stress-related to disease burden, dietary restrictions, functional limitations, associated chronic illnesses, adverse effects of medications, changes in self-perception and fear of death.[2–5]
Depression is generally accepted to be the commonest psychological problem encountered in patients with ESRD.[1] It consists of a constellation of symptoms including anhedonia, feelings of sadness, helplessness, hopelessness, guilt and is accompanied by changes in sleep, appetite and libido.[1]
Sleep is important for overall physical and mental well-being. Sleep disturbances can include irregularity in sleeping habits, difficulty falling asleep, early morning awakening, frequent awakening at night, sleep apnea and restless leg syndrome. Sleep disturbances among dialysis patients are found to be related to duration of dialysis therapy, high levels of urea and/or creatinine, pain, disability and somatic complaints such as pruritus and bone pain.[6] The prevalence of sleep problems [insomnia, restless leg syndrome (RLS), periodic limb movement during sleep (PLMS), and sleep apnea] might contribute to impaired quality of life in patients with ESRD.[7]
Materials and Methods
We conducted a cross-sectional study to find out the prevalence of depression and sleep problems in patients on maintenance HD for more than 3 months and correlate it with their demographic profile. In addition, we studied the prevalence of depression in primary caregivers of the patients.
Our study includes 69 outpatients on maintenance HD from a dialysis center of a state-run tertiary care hospital in New Delhi, which caters to patients belonging to differing social and economic strata. All the patients dialyzed during March 2008 to May 2008 who were on HD for more than 3 months, were included. The patients were explained the aim and protocol of the study and were asked for their consent to participate. Of 73 patients approached, 69 agreed to participate and a written informed consent was obtained.
Patients were interviewed and were asked to complete a battery of questionnaires including Beck Depression Inventory (BDI) and Berlin Sleep Apnea (BSA) Questionnaire. Patients received the questionnaires in one of the routine visits for HD. A member of the research team interviewed them, explained the details and confirmed the answers with patients as to whether they scored properly about their subjective symptoms.
The original version of the Beck Depression Inventory (BDI-I) was used to assess the severity of the depressive symptoms.[8] The BDI is a 21-item self-report rating inventory measuring characteristic attitudes and symptoms of depression, with scores reflecting the presence and the severity of depressed mood. The 21 items are intended to be answered according to a 4-point Likert scale, in which 0 represents the absence of the problem and 3 represents an extreme problem, with a total score range of 0-63. The BDI is the most popular self-reporting tool for measuring depressive symptoms. It is a well-validated index of depression with a good correlation with the diagnosis of depression, and has been widely used to evaluate mental health in ESRD patients.[910] Patients who had a BDI score >15 were considered to have depressive symptoms, which is a slightly higher cutoff compared with the general population so as to avoid overdiagnosis of depression.[1112]
The primary caregivers were also asked for their consent to participate. They were also requested to complete the BDI. The BDI cutoff score for depression in this group was taken as >10. Although the cutoff has been variable in different studies, a score of >10 in general population and >15 in patients with ESRD has been suggested as a cutoff for depression.[13]
Symptoms of sleep apnea were assessed using a standardized BSA Questionnaire, which is regarded as a well-validated tool that predicts sleep apnea risk.[14] The Berlin Questionnaire is a 10-item questionnaire,[14] divided in three categories according to symptoms: snoring, sleepiness or chronic fatigue, presence of hypertension or obesity defined as BMI above 30 kg/m2. A subject is considered to have a high risk for obstructive sleep apnea if he/she is positive in any two of the categories. Being in the high-risk group predicted an apnea-hypopnea index >5/h with a sensitivity of 0.86, a specificity of 0.77 and a positive predictive value of 0.89.[14] Patients were classified into high risk and low risk for sleep apnea according to their response.
To assess insomnia we gave a battery of questions including difficulty falling asleep, maintaining sleep, non-refreshing sleep, inadequate sleep duration and evaluated the presence and frequency of the symptoms. Patients were considered to be suffering from insomnia if they reported at least one symptom to be ‘frequent’.[7]
For data management and statistical analysis, we used Epi info software version 3.2. Variables were compared by an independent t-test or χ2 test between groups. Results were considered significant at P < 0.05.
Results
The study group consisted of 69 patients of which 47 (68.1%) were males and 22 (31.9%) were females. As per the protocol we included only those patients who were on dialysis for more than 3 months. Of these, patients who were on HD for more than 1 year (37.7%) formed a separate group for analysis and were compared to those on HD for and less than 1 year (62.3%). Mean age was 53.82 ± 8.61 years. 43.5% of patients were between ages 40 and 55 years, while another 39.1% were over 55 years. The remaining (17.4%) were under 40 years of age.
Table 1 summarizes the demographic characteristics of the study population, Table 2 shows the prevalence of depression and sleep problems and Table 3 shows correlation of depression and sleep problems with various demographic characteristics.

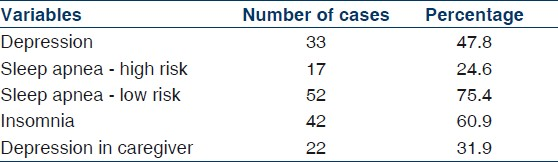
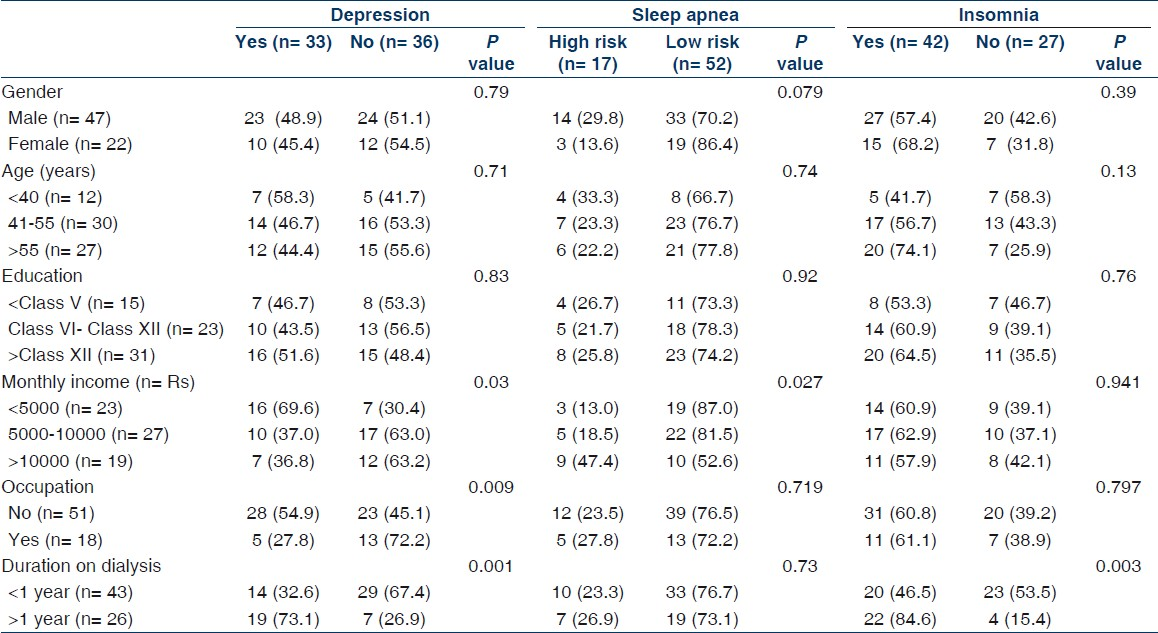
The prevalence of depression in our study population was 47.8%. Depression was found to be significantly more in patients who had monthly income less than Rs 5000, P=0.03, and among those who were on dialysis for more than 1 year (P=0.001). It was significantly less in patients who were employed even after being started on dialysis (P=0.009).
24.6% of the patients were found to be at risk for sleep apnea. Patients who were at high risk for sleep apnea tended to be males (P=0.07), and those who had monthly income more than Rs. 10000 (P=0.02).
We found very high prevalence of insomnia in our study group (60.9%). It was higher in patients who were older than 55 years, but did not reach significant levels. Insomnia was significantly higher in patients who were on dialysis for more than 1 year (P=0.003).
Of the 69 primary caregivers, 22 (32%) had a BDI score >10.
Discussion
Our study demonstrates the prevalence of depression and sleep disorders in patients on maintenance HD at a tertiary urban hospital in India, using a cross-sectional survey design. There is existing literature with quite a few numbers of studies assessing the prevalence of depression and sleep problems in ESRD patients on maintenance HD from other countries. Although these studies have established that such patients have a high overall prevalence of depression and sleep problems, there is paucity of such data from our country.
Compared to the population studied in the previous studies, there are significant differences in socioeconomic and cultural background of our population. Cultural and family values, social networking, family bonding with more involvement of caregiver, household earning system, lack of insurance or other benefits such as disability insurance are factors which could affect prevalence of depression and sleep problems in these patients. In addition, higher rate of illiteracy and poor socioeconomic conditions in our population could play an important role. There is also a lack of access to medical facilities, especially access to psychiatric evaluation and care. Only few studies have looked at socioeconomic factors associated with depression, and there are no studies looking at the prevalence of depression and sleep problems among HD patients from India. Mahajan et al.[15] have analyzed the incidence of depression and its effects on outcome among Indian peritoneal dialysis patients. Our study also evaluates the much less studied and much less established prevalence of depression in primary caregivers of the patients, who are at increased risk of depression from overall disease burden.
Additionally, country to country variability has also been recently noted for prevalence of sleep disorders in dialysis patients,[16] and could be explained at least in part by the suggested racial influence on self-reported sleep quality.[17] The present study was therefore undertaken to evaluate the actual prevalence of depression and sleep disturbances, and factors associated among Indian HD patients.
Similar to many other chronic diseases, ESRD affects the psychological state of the patients. Psychiatric illness in patients with ESRD has intrigued healthcare workers due to its effect on the morbidity and healthcare costs. Depression is recognized as the most common psychiatric abnormality, and is second only to hypertension in frequency as a comorbid diagnosis in ESRD patients.[31819] Estimated rates of clinical depression range from 20 to 30%, with as many as 42% showing some form of depressive affect.[1320–24] These rates are substantially higher than those found in the general population, for which rates of depression are 3%-6%,[25] and those found in older adults, for whom rates are 6%-10%.[26]
It is noteworthy that these estimates may be erroneously low, because patients often fail to seek mental healthcare. Nephrologists and dialysis nurses, who are not psychiatrists, often fail to recognize such symptoms, and physicians may pay less attention to somatic complaints of psychiatric illnesses, and therefore, leave these comorbidities undiagnosed. In India, it might be further more difficult to assess actual prevalence of depression or other psychiatric illnesses in these vulnerable patients, given the lack of access to mental healthcare and social stigma associated with psychiatric diagnoses.
Depression has significant effects on both individual patient well-being and delivery of medical care. HD patients with depression have lower quality of life, more functional impairments, greater occurrence of comorbid conditions and psychopathological states including suicide, lower adherence to drug treatment and an increased likelihood of long-term body pain.[2127–29] These patients also have higher rates withdrawal from maintenance dialysis, hospitalization, cardiovascular disease events and mortality.[22–2430–32]
In the past two decades, several questionnaires (including BDI, Hamilton Depression Rating Scale, Hospital Anxiety and Depression Scale; Center for Epidemiological Study of Depression) have been used to screen for depression in ESRD patients. The BDI has been studied extensively, and its use has been validated to screen for depression in patients with ESRD.[9133334] Although the cutoff has been variable in different studies, a higher cutoff value has been proposed to diagnose depression in patients on maintenance dialysis.[92135] Craven et al.[9] showed that a BDI score ≥15 had a 92% diagnostic sensitivity and 80% specificity in making the diagnosis of depressive disorder in patients with ESRD treated with HD or peritoneal dialysis. Even other studies using different questionnaires have used higher cutoff scores for depression in HD patients compared to general population.[2021]
Our results reveal a high prevalence (47.8%) of depressive symptoms among HD patients, similar to various studies across different populations around the world.[1321–23] The prevalence of depression in the current study was higher than that reported previously in the DOPPS (20%)[36] and CHOICE studies (19-24%).[3037] Ibrahim and Salamony[37] reported a prevalence of depression to be 33.33% (BDI score ≥15). Patients with BDI scores ≥15 had significantly lower total quality of life scores and mental scores in the same study.[37] Different studies have used different criteria for diagnosing depression. Lowry and Atcherson[38] reported an 18% prevalence of major depression, using American Psychiatric Association criteria, in a group comprised mostly of white patients beginning home HD in Iowa. Hinrichsen et al.[39] found that 17.7% of prevalent center HD patients satisfied criteria for minor depressive disorder, and 6.5% met criteria for a diagnosis of major depression according to the Schedule for Affective Disorders and Schizophrenia.
There was no gender difference in the prevalence of depression in this study. This is consistent with another study from Pakistan which showed similar finding,[40] though many studies do clearly indicate higher prevalence of depression in female patients. Ibrahim and Salamony[37] report that out of 20 patients with BDI score ≥15, 14 were females. Unemployment is an important factor associated with depression in these patients. Those patients who were employed even after start of dialysis had significantly lower prevalence (P=0.009) of depression. This association has also been reported previously.[37] Patients have a sense of being a financial burden, which is much more when they are unemployed. Also the patients who had been on dialysis for more than a year had increased prevalence of depression. This can be attributed to increased sense of dependence on dialysis for survival over a long period of time.
Sleep disorders, which in turn aggravate the well-being of ESRD patients.[41] Further, it is important to realize that unrecognized depression may compromise the patients’ quality of life and may cause sleep disorders, increasing the mortality risk in HD patients.[164243]
Interestingly, 80% of dialysis patients suffer from sleep abnormalities,[44] much more than the general population. The most frequently reported complaints are insomnia, restless leg syndrome, sleep-disordered breathing and excessive daytime sleepiness.[41]
The results of our study show increased prevalence of sleep disorders in our HD population. The sleep disorders are usually observed in the old-age group,[4546] while our subjects were relatively young , which supports more the notion that uremia and its complications are more likely to be the cause of these sleep disorders in HD patients than aging.
In our study, based on the BSA Questionnaire, 24.6% patients were classified as high risk for sleep apnea. These findings are consistent with those from other studies which have shown similar findings. Mucsi et al. report that 32% patients were high risk for sleep apnea.[4] There was a trend for males to be at high risk for sleep apnea (P=0.07). This tendency can be explained because sleep apnea is more common in men in the general population. Also, the prevalence of sleep apnea increases with age, but we did not observe this tendency. Musci et al.[4] suggested that pathophysiology of sleep disorders like sleep apnea, insomnia may be different in general population and in medically ill which is reflected by high prevalence in the latter group and relative lack of age and gender associations seen in general population.
The prevalence of insomnia among our study participants was 60.9%, comparable to previous reports of insomnia in HD patients.[46–49] Mucsi et al.[7] report 49% patients were insomniac in the study conducted by them. Williams et al.[6] reported that sleep problems ranged from 40 to 61%. Kraus and Hamburger[50] found that 60% of their dialysis sample complained of sleep problems. Other studies reported approximately 50% of their patients with sleep disturbances.[6] Epidemiological studies in general population have shown higher prevalence of insomnia symptoms in females.[7] Our study did not find any such gender association. We cannot provide a good explanation for this, but as discussed earlier different pathophysiology of sleep disorders in medically ill patients might be responsible.
Older studies have suggested impairment in the quality of life in caregiver of dialysis patients.[5152] There have not been many studies specifically studying depression in this group. Our study reports high prevalence of depression in the caregivers of patients on dialysis. This can be explained as caregivers of HD patients may feel a heavy burden because they are obliged to play an important role in supporting patients on dialysis. We suggest social and psychological support interventions to be considered to improve the symptoms of depression in this group.
There are several limitations to our study. These include a lack of a community comparison group and the reliance on self-report measures for assessing depression and sleep disorders. Secondly, testing was performed during one of the routine HD visits. Although testing in this environment may result in worse test performance and limit the generalizability of tests to other populations, it has the beneficial effect of assessing HD patients in the same environment in which they are likely to receive most medical counseling from healthcare providers. A third important limitation was the lack of a gold standard for identifying depression. Although the BDI provides reasonable screening data, identifying patients at risk for depression, it does not diagnose depression itself, and several of these symptoms are common in the dialysis population. There is strong overlap between uremic and depressive symptoms, making it difficult to recognize and define “depression” in the ESRD population.
Conclusion
Maintenance HD is associated with high prevalence of depression and insomnia. A significant part of this population is at high risk for sleep apnea syndrome. Apart from this, the primary caregivers also have increased tendency to have depressive symptoms.
Sleep problems (insomnia, sleep apnea) are associated with higher illness intrusiveness which represents illness-induced disruptions to lifestyles and activities.[4] Depression has been linked to an increased risk of mortality, hospitalization and dialysis withdrawal in different studies.
Our results, thus, advocate for incorporating a standard assessment and eventually treatment of depression and sleep disorders into the standard care provided to HD patients to improve psychological and overall well-being, quality of life, and consequently, reduce morbidity and mortality risk in this population. In addition, we believe that our finding of a high prevalence of depression in the caregivers of the patients is of interest to the clinician.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Depression in chronic dialysis patients: assessment and treatment. Nephrol Dial Transplant. 2000;15:1911-3.
- [Google Scholar]
- Depression, symptoms and the quality of life in patients on Hemodialysis for End Stage Renal Disease. Am J Nephrol. 2009;29:36-42.
- [Google Scholar]
- Pathways linking affective disturbances and physical disorders. Health Psychol. 1995;14:374-80.
- [Google Scholar]
- Depression, alexithymia and long-term mortality in chronic hemodialysis patients. Psychother Psychosom. 2010;79:303-11.
- [Google Scholar]
- Correlates of sleep behavior among hemodialysis patients, The Kidney Outcomes Prediction and Evaluation (KOPE) Study. Am J Nephrol. 2002;22:18-28.
- [Google Scholar]
- Sleep disorders and illness intrusiveness in patients on chronic dialysis. Nephrol Dial Transplant. 2004;19:1815-22.
- [Google Scholar]
- The Beck Depression Inventory as a screening device for major depression in renal dialysis patients. Int J Psychiatry Med. 1988;18:365-74.
- [Google Scholar]
- The diagnosis of major depression in end-stage renal disease. Psychother Psychosom. 1997;66:38-43.
- [Google Scholar]
- The Beck Depression Inventory requires modification in scoring before use in a haemodialysis population in the UK. Nephron Clin Pract. 2008;110:c33-8.
- [Google Scholar]
- Depression and anxiety in urban hemodialysis patients. Clin J Am Soc Nephrol. 2007;2:484-90.
- [Google Scholar]
- Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131:485-91.
- [Google Scholar]
- Analysis of depression and its effect on outcome among adult Indian peritoneal dialysis patients. Perit Dial Int. 2007;27:94-6.
- [Google Scholar]
- Sleep quality predicts quality of life and mortality risk in haemodialysis patients: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS) Nephrol Dial Transplant. 2008;23:998-1004.
- [Google Scholar]
- Racial differences in health-related quality of life among hemodialysis patients. Kidney Int. 2004;65:1482-91.
- [Google Scholar]
- US Renal Data System: USRDS 2004 Annual Data Report: Atlas of End-Stage Renal Disease in the United States, Bethesda, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases.
- [Google Scholar]
- Survival in hemodialysis patients: the role of depression. J Am Soc Nephrol. 1993;4:12-27.
- [Google Scholar]
- Depression and cognitive function in maintenance hemodialysis patients. Am J Kidney Dis 2010 [In Press]
- [Google Scholar]
- The predictive value of self-report scales compared with physician diagnosis of depression in hemodialysis patients. Kidney Int. 2006;69:1662-8.
- [Google Scholar]
- Death or hospitalization of patients on chronic hemodialysis is associated with a physician-based diagnosis of depression. Kidney Int. 2008;74:930-6.
- [Google Scholar]
- Dialysis Outcomes and Practice Patterns Study (DOPPS): Depression as a predictor of mortality and hospitalization among hemodialysis patients in the United States and Europe: Kidney Int. . 2002;62:199-207.
- [Google Scholar]
- The association of depressive symptoms with survival in a Dutch cohort of patients with end-stage renal disease. Nephrol Dial Transplant. 2010;25:231-6.
- [Google Scholar]
- The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095-105.
- [Google Scholar]
- Prevalence and risk factors for depression in non-demented primary care attenders aged 75 years and older. J Affect Disord. 2008;111:153-63.
- [Google Scholar]
- Functional impairment, depression, and life satisfaction among older hemodialysis patients and age-matched controls: a prospective study. Arch Phys Med Rehabil. 2000;81:453-9.
- [Google Scholar]
- Depression is an important contributor to low medication adherence in hemodialyzed patients and transplant recipients. Kidney Int. 2009;75:1223-9.
- [Google Scholar]
- Depressive symptoms predict the subsequent risk of bodily pain in dialysis patients: Japan Dialysis Outcomes and Practice Patterns Study. Pain Med. 2009;10:883-9.
- [Google Scholar]
- Temporal relation among depression symptoms, cardiovascular disease event, and mortality in end stage renal disease: contribution of reverse causality. Clin J Am Soc Nephrol. 2006;1:496-504.
- [Google Scholar]
- Effect of depression on health care utilization in patients with end-stage renal disease treated with hemodialysis. Eur J Intern Med. 2009;20:411-4.
- [Google Scholar]
- Multiple measurements of depression predict mortality in a longitudinal study of chronic hemodialysis outpatients. Kidney Int. 2000;57:2093-8.
- [Google Scholar]
- Depression in end-stage renal disease patients treated with hemodialysis: tools, correlates, outcomes, and needs. Semin Dial. 2005;18:91-7.
- [Google Scholar]
- Depression in end-stage renal disease hemodialysis patients. Nat Clin Pract Nephrol. 2006;2:678-87.
- [Google Scholar]
- Validation of 2 depression screening tools in dialysis patients. Am J Kidney Dis. 2005;46:919-24.
- [Google Scholar]
- Health -related quality of life as a predictor of mortality and hospitalization: The Dialysis Outcomes and Practice Patterns Study (DOPPS) Kidney Int. 2003;64:339-49.
- [Google Scholar]
- Depression, quality of life and malnutrition-inflammation scores in hemodialysis patients. Am J Nephrol. 2008;28:784-91.
- [Google Scholar]
- A short-term follow-up of patients with depressive disorder on entry into home hemodialysis training. J Affect Disord. 1980;2:219-27.
- [Google Scholar]
- Quality of sleep and health-related quality of life in haemodialysis patients. Nephrol Dial Transplant. 2003;18:126-32.
- [Google Scholar]
- Characteristics of depression in hemodialysis patients: symptoms, quality of life and mortality risk. Gen Hosp Psychiatry. 2006;28:306-12.
- [Google Scholar]
- Insomnia symptoms and their correlates among the elderly in geriatric homes in Alexandria, Egypt. Sleep Breath. 2007;11:187-94.
- [Google Scholar]
- Sleep disorders in hemodialysis patients. Saudi J Kidney Dis Transpl. 2010;21:300-5.
- [Google Scholar]
- Sleep disorders in patients with end-stage renal disease undergoing dialysis therapy. Nephrol Dial Transplant. 2006;21:184-90.
- [Google Scholar]
- Factors contributing to sleep disturbance and hypnotic drug use in hemodialysis patients. Intern Med. 2006;45:1273-8.
- [Google Scholar]
- Sleep disturbance in chronic hemodialysis patients: the impact of depression and anemia. Ren Fail. 2007;29:673-7.
- [Google Scholar]
- Quality of life of family caregivers of elderly patients on hemodialysis and peritoneal dialysis. Am J Kidney Dis. 2006;48:955-63.
- [Google Scholar]
- Burden and quality of life of caregivers for hemodialysis patients. Am J Kidney Dis. 2002;39:805-12.
- [Google Scholar]







