Translate this page into:
Difficult Vascular Access in a Patient on Chronic Hemodialysis
Address for correspondence: Dr. G. Kumar, Department of Pediatric Nephrology, Sheikh Khalifa Medical City, Al Karamah Street, P. O. Box 51900, Abu Dhabi, UAE. E-mail: kumargurinder@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Long-term chronic hemodialysis in patients with end-stage renal failure requires a durable vascular access. Patients with central venous catheters (CVCs) are prone for recurrent infections, vascular thrombosis, and vascular stenosis, which contribute to significant morbidity and mortality. We present a case of a 31-year-old male who had a transhepatic hemodialysis catheter lasting for 4.5 years.
We report a 31-year-old male who had been on renal replacement therapy for the past 15 years. The native kidney disease was reflux nephropathy progressing to end-stage renal failure. Peritoneal dialysis was started at the onset but had to be switched to hemodialysis due to recurrent peritonitis. Multiple attempts for arteriovenous fistula and grafts were unsuccessful. Prothrombotic workup was negative. Hence, the patient had been maintained on tunneled CVCs (internal jugular/subclavian and femoral access) for almost 12 years. Femoral access was 14 F × 24 cm permacath, and the tip was positioned within the left semi azygos vein. However, multiple vessel catheterization and instrumentation resulted in thrombosis of most of his accessible veins including iliac veins along with superior vena cava syndrome.
Computed tomographic angiography done showed multiple dilated vascular channels seen in the anterior abdominal wall, perihepatic, mesenteric, and retroperitoneal region, pelvis as well as in both groins. There was evidence of probable left axillary-iliac bypass, which was thrombosed [Figure 1].
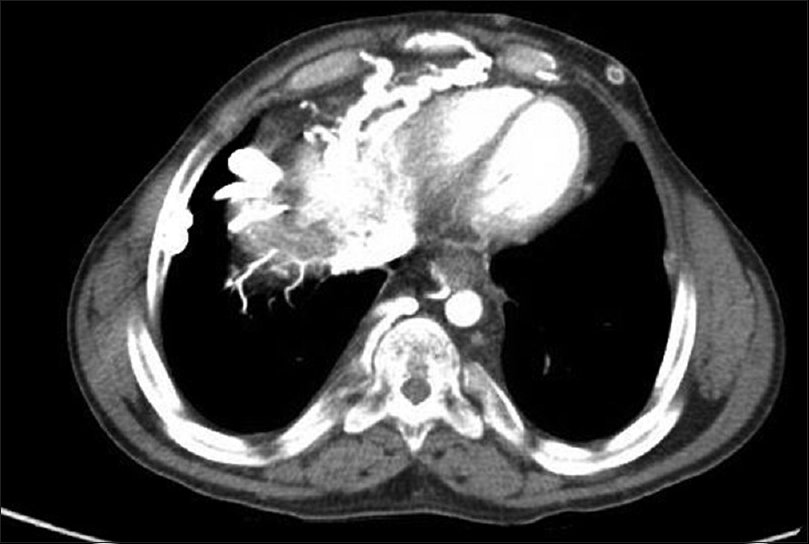
- Computed tomographic angiogram abdomen showing multiple dilated vascular channels in anterior abdominal wall and perihepatic, mesenteric, and retroperitoneal regions
Ultimately, he required a transhepatic vascular access, which was inserted in September 2012. SplitCath III-Medcomp permacath 14 F × 28 cm was used and catheter tip was confirmed in inferior vena cava (IVC). The hepatic route was chosen over translumbar route in view of higher risk of complications encountered with translumbar approaches such as bleeding secondary to injury to right renal artery or its aberrant branches, kinks. Transrenal route, although described, is not used as renal veins are not desirable in patients with kidney disease. Transfemoral catheter is usually inserted for short-term use and may not be very suitable for patients on chronic hemodialysis.
After a primary patency of 1 year, there were issues of inadequacy of dialysis as Kt/V was 0.8 and urea reduction rate was 54%. Hence, repeat angiography was done which showed right hepatic vein stenosis. This was treated with 8 mm balloon (noncompliant balloon 8 mm diameter × 4 cm long and pressure applied was 14 psi) angioplasty and successful over-the-wire catheter exchange, with placement of a 28 cm tunneled transhepatic split tip catheter (Ash Split) [Figures 2 and 3]. Subsequently, the patient has been doing well with the same catheter for the past 4.5 years. There has been no infection during this period. The primary patency was for 1 year and primary assisted patency was for 4.5 years.

- Image of the location of transhepatic vascular access on the patient
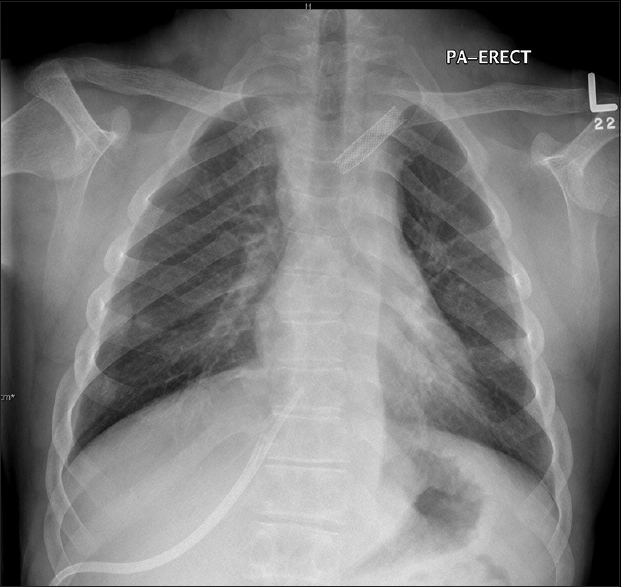
- X-ray of the chest showing the transhepatic vascular access
Maintaining vascular access is a challenge while managing patients with end-stage renal disease as the CVCs carry a significant risk of infection and occlusion requiring an exchange. One of the long-term sequelae of CVC use is central venous occlusion.[1] The most commonly sites of placement of dialysis catheters, in order of preference, are right internal jugular vein, left internal jugular vein, external jugular veins, and femoral veins. Rahman and Kuban elaborated unconventional routes of placement of dialysis catheters including placing them through translumbar, transhepatic, and transrenal route.[2] Po et al. first described the transhepatic approach when they reported a similar patient who had failed peritoneal dialysis and difficult vascular access and required a transhepatic vascular access which lasted for over 1 year.[3] Immediate complications associated with transhepatic vascular access include perihepatic hematoma and hepatic arterial injury, and long-term complications include catheter dislodgement/migration, catheter-related sepsis, and catheter thrombosis. Sanal et al. evaluated 38 patients with transhepatic tunneled hemodialysis catheters and evaluated the patency using Kaplan–Meier analysis and found it to be a safe and functional alternative route in patients who do not have an accessible central venous route.[4]
In conclusion, transhepatic venous catheterization is an option for patients on chronic hemodialysis who have exhausted all the other options of central venous access provided the suprarenal IVC is patent. It can be a reliable vascular access if there are no secondary complications of thrombosis and infection.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Complex central venous catheter insertion for hemodialysis. J Vasc Access. 2014;15(Suppl 7):S136-9.
- [Google Scholar]
- Dialysis catheter placement in patients with exhausted access. Tech Vasc Interv Radiol. 2017;20:65-74.
- [Google Scholar]
- Safety and functionality of transhepatic hemodialysis catheters in chronic hemodialysis patients. Diagn Interv Radiol. 2016;22:560-5.
- [Google Scholar]






