Translate this page into:
DNAJB9-Associated Fibrillary Glomerulonephritis and Immunoglobulin A Nephropathy – A Rare Combination
Corresponding author: Dr. Sajeesh Sivadas, Department of Nephrology, Aster MIMS Hospital, Kotakkal, Kerala, India. E-mail: drsajeeshsivadas@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sivadas S, Narayanan R, Kurien AA, Abdulla MC. DNAJB9-Associated Fibrillary Glomerulonephritis and Immunoglobulin A Nephropathy – A Rare Combination. Indian J Nephrol. 2024;34:276–7. doi: 10.4103/ijn.ijn_101_23
Dear Editor,
A 67-year-old gentleman presented to us for evaluation of incidentally detected renal dysfunction. He had systemic hypertension for 10 years and was recently detected to have diabetes. The blood pressure was 150/90 mm of Hg and had no evidence of target organ damage related to diabetes or hypertension.
Urinalysis showed 2+ albuminuria with 10–16 red blood corpuscles/high-power field. The urine spot protein–creatinine ratio was 3.1 and serum creatinine was 1.6 mg/dl. C3 and C4 levels were normal. Serological testing for hepatitis B surface antigen, hepatitis C antibody, antinuclear antibody, antineutrophilic cytoplasmic antibodies, anti-glomerular basement membrane antibodies, serum cryoglobulins, and human immunodeficiency virus antibody were all negative. Serum protein electrophoresis with immunofixation was negative for monoclonal protein.
Renal biopsy showed histopathologic findings consistent with fibrillary glomerulonephritis and immunoglobulin A nephropathy dual glomerulopathy (in light, immunofluorescence, and electron microscopy), and all glomeruli stained positive for DNA-J heat-shock protein family member B9 (DNAJB9) [Figure 1].
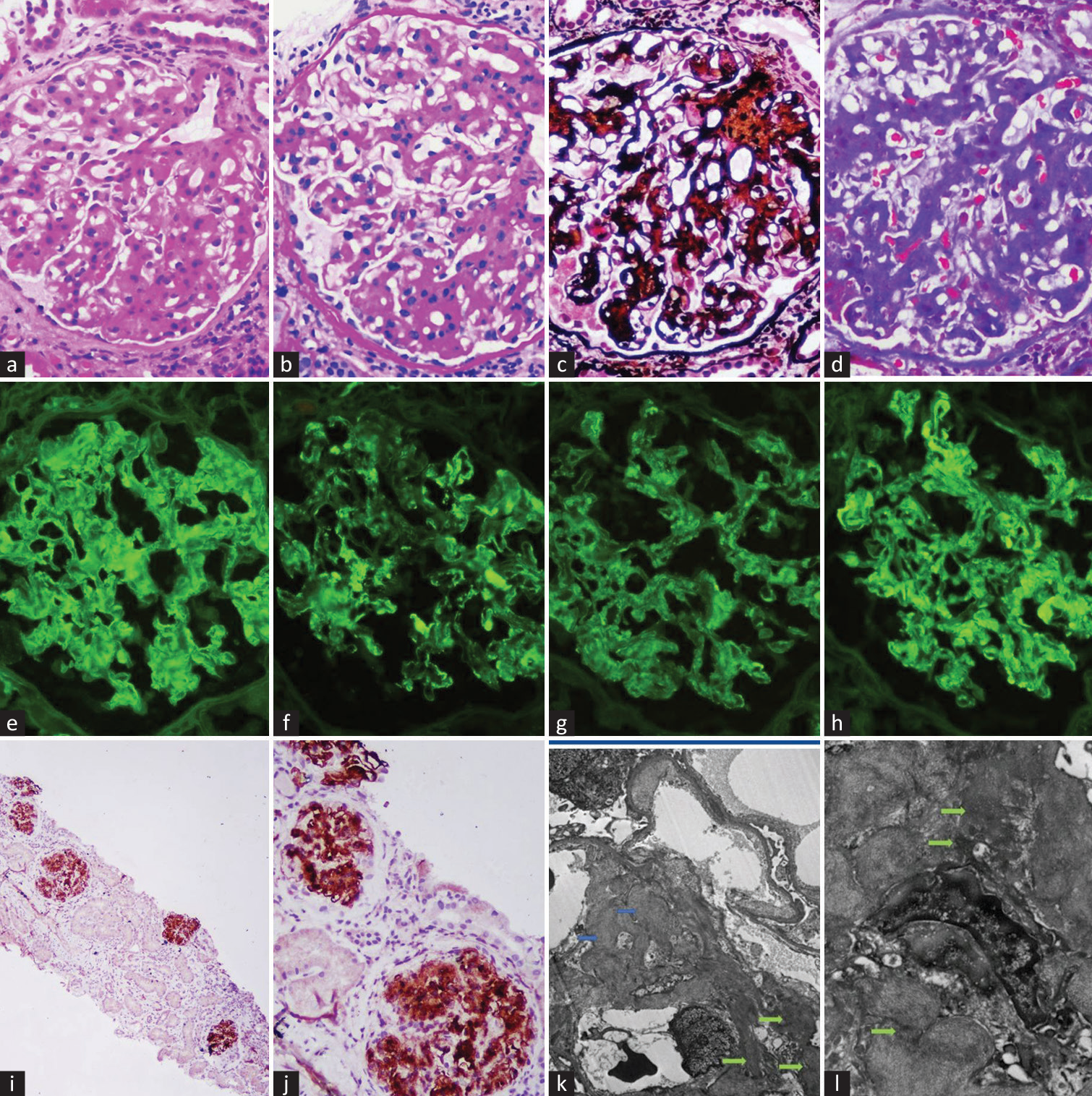
- Renal biopsy showing mesangioproliferative pattern of glomerular injury on light microscopy (a–d). Immunofluorescence microscopy showing smudge positivity of IgG along the capillary loops with intensely positive IgA and C3 over mesangium (×400) (e–h). Glomeruli were intensely positive for DNAJB9 immunohistochemical stain (×600) (i and j). Electron microscopy confirmed nonbranching linear fibrils on capillary loops and mesangium, along with electron-dense deposits consistent (arrows) with IgA over mesangium (k and l) DNAJB9 = DNA-J heat-shock protein family member B9.
His renin-angiotensin-aldosterone system blockade was enhanced to 80 mg daily of telmisartan. At 6 months follow-up, he is asymptomatic, and his blood pressure is well controlled with a serum creatinine of 1.4 mg/dl and urine spot protein–creatinine ratio of 1.6. He is advised to remain on close follow-up.
Coexistent FGN–IgAN glomerulopathy is an extremely rare form of glomerular disease.1,2 FGN–IgAN has a similar clinical presentation as FGN and is associated with infections (hepatitis C), autoimmune diseases, or malignancy in 30% of cases.3 In our patient, workup for secondary causes of FGN was negative. The discovery of DNAJB9 and immunohistochemical staining for DNAJB9 now make it possible to diagnose FGN even in the absence of ultrastructural evaluation.3 Our report highlights a patient with idiopathic FGN–IgAN dual glomerulopathy, an extremely rare glomerular disease. To our knowledge, this condition has not been reported before from the Indian subcontinent.
Acknowledgements
The authors thank Christopher P. Larsen, Arkana Laboratories, Little Rock, AR, USA, for his advice and help.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
References
- DNAJB9 is a specific immunohistochemical marker for fibrillary glomerulonephritis. Kidney Int Rep. 2018;3:56-64.
- [CrossRef] [PubMed] [Google Scholar]
- Fibrillary glomerulonephritis: Clinicopathologic features and atypical cases from a multi-institutional cohort. Clin J Am Soc Nephrol. 2019;14:1741-50.
- [CrossRef] [PubMed] [Google Scholar]
- Characteristics of patients with coexisting DNAJB9-associated fibrillary glomerulonephritis and IgA nephropathy. Clin Kidney J. 2021;14:1681-90.
- [CrossRef] [PubMed] [Google Scholar]






