Translate this page into:
Extramedullary Hematopoiesis: An Unusual Cause for Acute Kidney Injury
Address for correspondence: Dr. Anila Abraham Kurien, Renopath, Center for Renal and Urological Pathology, No. 27&28, VMT Nagar, Kolathur, Chennai - 600 099, Tamil Nadu, India. E-mail: anila_abraham08@yahoo.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Extramedullary haematopoiesis (EMH) is the development of hematopoietic tissue outside the bone marrow and commonly occurs in the reticuloendothelial system (liver and spleen). The involvement of other parenchymal organs is unusual. We describe a rare case of renal EMH due to acute lymphoblastic leukaemia presenting as renal failure.
A 29-year-old man presented with fever, anorexia, vague abdominal pain and weight loss of 7kg. On examination, he was pale, icteric; there was no lymphadenopathy. His blood pressure was 130/80 mmHg. Systemic examination revealed hepatosplenomegaly. There was no free fluid in the abdomen. Other systems were normal clinically. Blood tests showed haemoglobin of 6.5 g/dl, white cell count 3.5 × 10 3/ml (neutrophils 68%, lymphocytes 29% and eosinophils 3%). Serum creatinine was 11.1 mg/dl; serum potassium 6.4 mEq/l, corrected calcium levels 11.2 mg/dl. Lactate dehydrogenase was 548 U/l. Uric acid was 22 mg/dl. His liver function tests were as follows: serum bilirubin 4.5 mg/dl, direct 2.4, indirect 2.1, alanine transaminase 135 IU, aspartate transaminase 180 IU, serum albumin 3.1 g/dl. Peripheral smear showed microcytic hypochromic RBCs, leukopenia, and platelets with normal count and morphology. Reticulocyte count was 0.5% and no blast cells were seen. Urine analysis showed bland urine sediments. Ultrasonagram of kidneys revealed normal-sized kidneys. Since the patient was oligoanuric with severe metabolic acidosis and features suggestive of tumour lysis syndrome, he was initiated on hemodialysis.
A kidney biopsy was performed. Histological examination revealed multiple foci of dense interstitial infiltrate with cells of three distinct lineages including myeloid cells, erythroid cells and megakaryocytes [Figure 1]. The myeloid cells showed large nuclei with open chromatin and a moderate amount of cytoplasm. Eosinophils and eosinophilic precursors were seen. Erythroid cells were present in clusters and had a hyperchromatic round nucleus with a thin rim of cytoplasm. Megakaryocytes were recognised by their large size with multilobed nuclei and abundant granular cytoplasm. Interstitial haemorrhage and clusters of hemosiderin-laden macrophages were seen. Glomeruli and blood vessels were unremarkable but tubular epithelial cell injury was noted. There was no interstitial fibrosis and tubular atrophy. The diagnosis of EMH in the kidney was made. Immunohistochemical stains were performed to confirm the nature of the infiltrating cells. CD61 for megakaryocytes, myeloperoxidase for granulocytes and glycophorin for erythroid elements helped to establish the diagnosis [Figure 2]. The differential diagnosis on the biopsy includes acute interstitial nephritis as erythroid precursors may be mistaken for mature lymphocytes. Rarely, the megakaryocytes may resemble Reed–Sternberg cells in Hodgkin lymphoma. Lineage-specific immunohistochemical stains can be used to confirm the presence of hematopoietic cells.

- (a) Erythroid cells are usually present in clusters (arrows) H and E ×200. (b) Myeloid cells often include eosinophils and eosinophil precursors (black arrows). Hemosiderin granules (blue arrows) H and E ×200. (c and d) Megakaryocytes can be identified by their large size and multilobated nuclei (H and E ×200 in c, PAS ×400 in d)
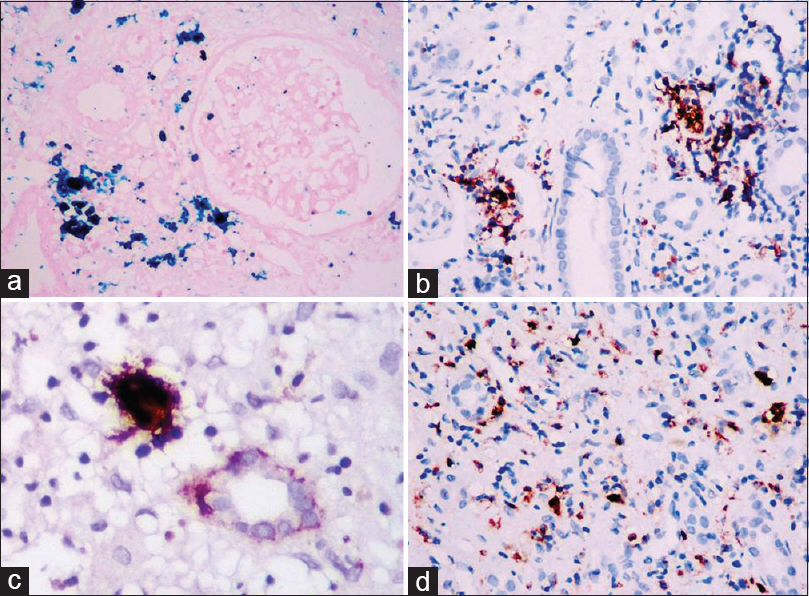
- (a) Hemosiderin granules are highlighted by Perls Prussian blue stain (×200). (b) Erythroid cells are identified with glycophorin immunostain (×200). (c) CD61 immunostain highlights a megakaryocyte (×400). (d) Myeloperoxidase stain identifies myeloid cells (×200)
Following the kidney biopsy, a bone marrow biopsy was done and a diagnosis of acute lymphoblastic leukemia T-cell lineage (Tdt +ve, CD3 +ve, CD 20 neg, CD 34 neg, MPO neg) was made. Leucopenia and the absence of blast cells in a peripheral smear in the patient could be explained by aleukemic variant of leukemia. After the first cycle of chemotherapy, though his renal function improved and he became dialysis independent, he developed pulmonary sepsis and succumbed to septic shock.
Renal EMH is a very rare occurrence with less than 20 cases that have been reported in the literature. Renal EMH has been reported in association with various haematological disorders include myeloma, myelofibrosis, chronic myeloid leukaemia and lymphoma. The renal involvement could be parenchymal, intrapelvic or perinephric and its manifestations vary depending upon the site of occurrence. Intrapelvic and perinephric lesions present as obstructive nephropathy, whereas parenchymal infiltration of renal interstitium presents as acute kidney injury similar to our patients. The pathophysiology of EMH in the kidney is not fully understood. It has been hypothesized that hematopoietic cells are derived from local mesenchymal pluripotent cells which then proliferate in response to a stimulating factor or may arise from the migration of stem cells from bone marrow to kidneys.[12] Renal extramedullary haematopoiesis has also been described in renal allografts.[3] However, most cases are asymptomatic and recognized on post-mortem examination.[14]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Renal extramedullary hematopoiesis: Interstitial and glomerular pathology. Mod Pathol. 2015;28:1574-83.
- [Google Scholar]
- Extramedullary haematopoiesis in the kidney: A case report and review of literature. Clin Lab Haematol. 2005;27:391-4.
- [Google Scholar]






