Translate this page into:
Fibrillary glomerulonephritis presenting as crescentic glomerulonephritis
Address for correspondence: Dr. H. H. Shah, Hofstra Northwell School of Medicine, 100 Community Drive, 2nd Floor, Great Neck, New York 11021, USA. E-mail: hshah2@northwell.edu
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Fibrillary glomerulonephritis (FGN) is a rare primary glomerular disease that commonly presents clinically with hypertension, proteinuria, microscopic hematuria, and varying degree of renal insufficiency. Histologically, FGN can present with different patterns of glomerular injury, more commonly mesangioproliferative, membranoproliferative, and membranous nephropathy. While crescent formation has been described in some kidney biopsy series of FGN, crescentic glomerulonephritis pattern of glomerular injury has been rarely described. Optimal therapy and outcomes in FGN presenting with crescentic GN is not currently known. We report an adult patient who presented with massive proteinuria and severe renal failure. The kidney biopsy revealed crescentic FGN (C-FGN). The patient remained dialysis dependent despite immunosuppressive therapy. We also briefly review FGN, and the few reported cases of C-FGN that presented as rapidly progressive or advanced renal failure in the literature.
Keywords
Crescentic glomerulonephritis
fibrillary glomerulonephritis
glomerulonephritis
rapidly progressive glomerulonephritis
Introduction
Fibrillary glomerulonephritis (FGN), a rare glomerular disease was first described in 1977.[1] This rare entity is characterized by the presence of elongated, nonbranching randomly arranged microfibrils (10–30 nm) in the mesangium and/or glomerular capillary wall. Ultrastructurally, the microfibrils seen in FGN are indistinguishable from amyloid fibrils however differ from amyloid by its larger size and lack of reactivity to reagents that detect amyloid including Congo red.[2345] Different histological patterns of glomerular injury have been described in the kidney biopsy series of FGN including mesangioproliferative, membranoproliferative, membranous, diffuse sclerosing, and rarely endocapillary proliferative and crescentic.[23456] Clinically, FGN presents commonly with hypertension, proteinuria, hematuria, and renal insufficiency.[2345] A recent single-institution study of 66 cases with FGN showed a mean serum creatinine of 2.1 mg/dl at the time of kidney biopsy; however, one-third of cases had normal range serum creatinine levels (≤1.2 mg/dl).[5]
Rapidly progressive glomerulonephritis (RPGN) is a rare clinical syndrome that is associated with extensive crescent formation surrounding ≥50% of glomeruli on kidney biopsy. FGN presenting as RPGN has rarely been reported. Optimal therapy and outcomes of cases of FGN who present with RPGN are unknown. We present an interesting adult case of FGN who presented with renal failure and massive proteinuria secondary to crescentic glomerulonephritis. We also review the few cases of FGN presenting as rapidly progressive or advanced renal failure and crescentic glomerulonephritis that have been reported in the literature.
Case Report
A 66-year-old Caucasian female presented to the emergency room (ER) with 4-week history of intermittent abdominal pain, nausea, vomiting, and poor oral intake. Nephrology consultation was called for an evaluation of increased creatinine (17.54 mg/dl) found on laboratories performed in the ER. Serum creatinine performed approximately 4 months prior to the ER visit was within normal range (1.24 mg/dl). The review of systems was significant for generalized weakness. Her medication included amlodipine, benazepril, hydrochlorothiazide, and pantoprazole. On physical examination, blood pressure was elevated at 160/82 mm Hg. The rest of the examination was unremarkable. Urinalysis was significant for 3+ proteinuria and 25–50 red blood cells per high power field. Initial laboratory evaluation also revealed elevated blood urea nitrogen of 119 mg/dl and low hemoglobin level of 8.7 g/dL. A 24 h urine collection revealed 33 g of protein. On admission, all of the patient's home medications except amlodipine were discontinued. The patient was initiated on hemodialysis for uremia management. Serological testing for hepatitis B surface antigen, hepatitis C antibody, antinuclear antibody, antineutrophilic cytoplasmic antibodies, anti-glomerular basement membrane antibody, cryoglobulins, and human immunodeficiency virus antibody were all negative. Complement levels were normal. Serum immunofixation did not reveal any monoclonal immunoglobulin. Renal sonogram revealed increased echogenicity in both kidneys. A kidney biopsy was subsequently performed.
On light microscopy, twelve glomeruli were identified in one section. Eight (67%) glomeruli contained large cellular crescents. Of the remaining four glomeruli that did not have crescents, one was globally sclerosed and one showed segmental mild mesangial matrix expansion. There was marked endocapillary hypercellularity seen in several glomeruli. There was no fibrinoid necrosis. Bowman's capsule was focally disrupted by crescents. Eighty percent of the tubules were intact and there was a mild degree of tubular atrophy. There was no evidence of acute tubular necrosis. There was no interstitial fibrosis. However, there was mild to moderate interstitial infiltrates comprising of lymphocytes and occasional eosinophils and neutrophils. Congo red stain was negative in glomeruli. Immunofluorescence microscopy showed 1+ fine granular deposits of IgG along the capillary loops and 1+ deposits of C3 predominately in the mesangium. There was no glomerular staining for IgA, IgM, C1q, kappa, or lambda light chains. Electron microscopy showed severe effacement of epithelial cell foot processes. Structured electron-dense material was seen predominately in the mesangium with some capillary loops having subendothelial deposition [Figure 1]. These structures were randomly arranged fibrils measuring from 10 to 35 nm in diameter. The kidney biopsy findings were consistent with crescentic FGN (C-FGN).

- Electron photomicrograph showing structured subendothelial electron-dense deposits (arrows). Structures are randomly oriented fibrils (×27,000)
In view of the light microscopy findings of crescentic glomerulonephritis, the patient was initiated on intravenous pulse corticosteroid (methylprednisolone 1 g) daily for 3 days followed by daily oral prednisone (1 mg/kg) therapy. The patient was also initiated on daily oral cyclophosphamide (1.5 mg/kg) therapy awaiting results of electron microscopy. Electron microscopy results subsequently revealed FGN. The patient continued to remain dialysis-dependent despite receiving approximately 7 weeks of combined corticosteroid and cyclophosphamide therapy. Subsequently, both immunosuppressive agents were discontinued.
Discussion
FGN is a rare glomerular disease seen in 0.5–1% of native kidney biopsy series.[23] Clinically, the mean age of presentation of FGN is 55–60 years.[2345] The male to female ratio described in larger case series of FGN varies from 1:1.2–1.8 and the ratio of White Americans to African Americans ranges from 8.3–9.5:0.2-1.[35] Clinical features at the time of kidney biopsy commonly include hypertension, proteinuria, hematuria, and varying degree of renal insufficiency. Serum creatinine could also be in normal range. Nephrotic syndrome can be seen in one-third of the cases.[5]
Although thought to be an idiopathic condition,[2] a recent single-institution study of 66 cases with FGN found an association with malignancy in 15 (23%) patients.[5] Six out of these 15 cases with FGN and malignancy had multiple myeloma.[5] FGN has also been associated with hepatitis C viral infection.[7]
FGN can present morphologically with varying patterns of glomerular injury.[23456] The presence of crescents on light microscopic examination of kidney biopsy specimens of FGN have varied from none in some large kidney biopsy series to up to 20% in other such series.[2356] However, crescentic glomerulonephritis defined by the presence of crescent affecting ≥50% of glomeruli has rarely been reported. Nasr et al. reported three cases of crescentic and necrotizing glomerulonephritis in their kidney biopsy study of 66 cases of FGN.[5] Interestingly, one case was associated with P-antineutrophil cytoplasmic autoantibodies seropositivity. However, the clinical presentation, management, and outcomes of these three FGN cases with crescentic glomerulonephritis were not presented in this study. Several recent case series of FGN have not reported cases of crescentic GN.[68]
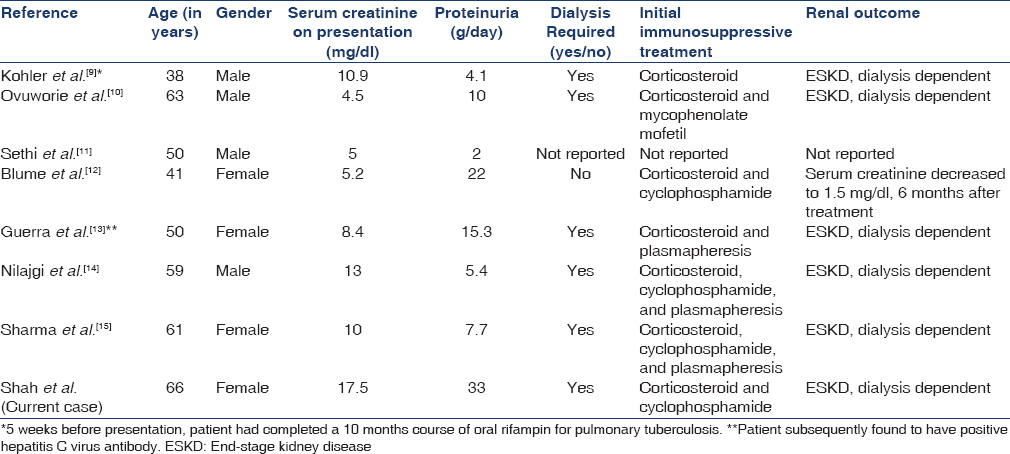
Few case reports of C-FGN cases presenting clinically with rapidly progressive or advanced renal failure have been described in the literature.[9101112131415] Table 1 summarizes the clinical presentation, treatment, and renal outcome of these cases.
FGN is associated with poor prognosis and 50% progress to end-stage kidney disease (ESKD) within 2 years of diagnosis.[235] Optimal approach and therapy for FGN are not known. While the use of both renin-angiotensin system (RAS) blockers alone or in combination with immunosuppressive agents has been reported in the literature, renal outcome to such therapeutic strategies is unknown. A retrospective study reported long-term renal outcomes in 27 cases with FGN who received either RAS blockers alone or in combination with immunosuppressive agents, mainly rituximab and cyclophosphamide.[6] As compared to the group that received immunosuppressive therapy, more (10 of 14) patients from the group that only received RAS blockers progressed to ESKD after a median 46-month follow-up period.[6] Of note, none of these patients had crescentic GN.[6] Another retrospective study evaluated the role of rituximab in 12 cases with FGN.[8] Eight out of the 12 cases had MPGN pattern of glomerular injury and none had crescentic GN.[8] The authors concluded that patients who did not progress with rituximab therapy had better renal function and shorter time from diagnosis to treatment than those who progressed during the study period.[8] Based on our literature review, optimal therapy of patients presenting with FGN and crescentic GN is not known and it seems that this group of patients may have a much poorer renal outcomes with rapid progression to ESKD than other patterns of glomerular injury described in patients with FGN.
Conclusion
We present a rare case of FGN presenting with crescentic glomerulonephritis. Our patient continued to remain dialysis-dependent despite receiving high-dose corticosteroid and cyclophosphamide for nearly 7 weeks.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This case was presented (as a poster presentation) at the National Kidney Foundation 2015 Spring Clinical Meetings in Dallas, Texas, USA, in March 2015.
References
- Nephrotic syndrome associated with amyloid-like glomerular deposits. Nephron. 1977;18:301-8.
- [Google Scholar]
- Fibrillary and immunotactoid glomerulonephritis: Distinct entities with different clinical and pathologic features. Kidney Int. 2003;63:1450-61.
- [Google Scholar]
- Clinical and pathologic features of fibrillary glomerulonephritis. Kidney Int. 1992;42:1401-7.
- [Google Scholar]
- Fibrillary glomerulonephritis and immunotactoid glomerulopathy. J Am Soc Nephrol. 2008;19:34-7.
- [Google Scholar]
- Fibrillary glomerulonephritis: A report of 66 cases from a single institution. Clin J Am Soc Nephrol. 2011;6:775-84.
- [Google Scholar]
- Long-term kidney disease outcomes in fibrillary glomerulonephritis: A case series of 27 patients. Am J Kidney Dis. 2013;62:679-90.
- [Google Scholar]
- Hepatitis C viral infection is associated with fibrillary glomerulonephritis and immunotactoid glomerulopathy. J Am Soc Nephrol. 1998;9:2244-52.
- [Google Scholar]
- Rituximab treatment for fibrillary glomerulonephritis. Nephrol Dial Transplant. 2014;29:1925-31.
- [Google Scholar]
- Crescentic fibrillary glomerulonephritis associated with intermittent rifampin therapy for pulmonary tuberculosis. Clin Nephrol. 1994;42:263-5.
- [Google Scholar]
- Rapidly progressive renal failure with nephrotic syndrome in a patient with type 2 diabetes mellitus: The differential of fibrillary deposits. Am J Kidney Dis. 2000;35:173-7.
- [Google Scholar]
- A case of fibrillary glomerulonephritis with linear immunoglobulin G staining of the glomerular capillary walls. Arch Pathol Lab Med. 2001;125:534-6.
- [Google Scholar]
- Fibrillary glomerulonephritis associated with crescents as a therapeutic challenge. Am J Kidney Dis. 2002;40:420-5.
- [Google Scholar]
- Crescentic fibrillary glomerulonephritis associated with hepatitis C viral infection. Clin Nephrol. 2003;60:364-8.
- [Google Scholar]
- Fibrillary glomerulonephritis: Presenting as crescentic glomerulonephritis causing rapidly progressive renal failure. NDT Plus. 2011;4:413-5.
- [Google Scholar]
- Fibrillary glomerulonephritis presenting as rapidly progressive glomerulonephritis. Am J Kidney Dis. 2012;60:157-9.
- [Google Scholar]







