Translate this page into:
From Rarity to Reality: Nivelon-Nivelon-Mabille Syndrome Presenting with Renal Tubular Acidosis
Corresponding author: Nitish Kumar, Division of Pediatric Nephrology, Department of Pediatrics, Institute of Medical Sciences, Banaras Hindu University, Varanasi, India. E-mail: doctornitishkumar@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Abhinay A, Panda S, Singh A, Kumar N. From Rarity to Reality: Nivelon-Nivelon-Mabille Syndrome Presenting with Renal Tubular Acidosis. Indian J Nephrol. 2024;34:678. doi: 10.25259/IJN_308_2024
Dear Editor,
A 9-year-old girl presented with growth failure, polyuria, and polydipsia for 4 years. Physical examination revealed rachitic rosary, wrist widening, and double malleoli without facial dysmorphism. There was a family history of infantile death from severe acute malnutrition. Laboratory investigations revealed normal anion-gap metabolic acidosis, hypokalemia, alkaline urine, and hypercalciuria. On the abdominal sonogram, bilateral medullary nephrocalcinosis was seen. Clinical and laboratory features were suggestive of distal renal tubular acidosis (dRTA). To confirm the diagnosis, genetic analysis was performed, revealing a novel heterozygous variant (c.10C>T, p.Arg4ter) in exon 2 of the Hedgehog Acyltransferase (HHAT) gene, which is classified as a likely pathogenic variant by the American College of Medical Genetics. The variant was confirmed with Sanger sequencing, as shown in [Figure 1]. The final diagnosis was dRTA due to Nivelon-Nivelon-Mabille syndrome (NNMS). Clinical screening of family members didn’t reveal any abnormality. Parents were given genetic counseling.
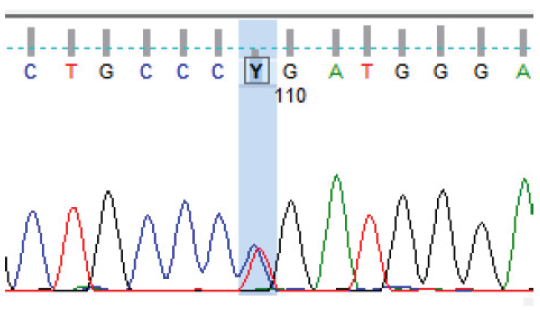
- Sanger sequencing data (electropherogram) showing nucleotide change at c.10C>T (p.Arg4Ter) in the HHAT gene. HHAT: Hedgehog Acyltransferase. Red, green, black, and blue color peaks in electropherogram show thymine, adenine, guanine, and cytosine bases, respectively.
NNMS is a rare autosomal recessive disorder that was originally reported in 1992 with antenatal severe dwarfism, global chondrodysplasia, severe microcephaly with cerebellar vermis hypoplasia, a hypoplastic iris, and a papillous coloboma.1 On extensive search of literature on NNMS, we found three cases. Abdel-Salam et al. (2019) reported two sisters from Saudi Arabia with microcephaly, cerebellar vermis hypoplasia, infantile-onset seizures, brachydactyly, and dysplastic nails.2 Saini et al. (2023) reported a patient with biallelic variants in HHAT, who presented with muscle spasm, microcephaly, short stature, muscle hypertrophy, and facial dysmorphism.3 There has been no report of renal involvement in NNMS. This letter intends to raise awareness among readers concerning the possibility of renal involvement in NNMS and HHAT gene-related disorders.
Acknowledgement
We thank all the residents and staff who were involved in the care of this patient.
Conflicts of interest
There are no conflicts of interest.
References
- New autosomal recessive chondrodysplasia—pseudohermaphrodism syndrome. Clin Dysmorphol. 1992;1:221-8.
- [PubMed] [Google Scholar]
- Biallelic novel missense HHAT variant causes syndromic microcephaly and cerebellar-vermis hypoplasia. Am J Med Genet A. 2019;179:1053-7.
- [CrossRef] [PubMed] [Google Scholar]
- Muscle spasms as presenting feature of nivelon-nivelon-mabile syndrome. Am J Med Genet A. 2023;191:238-48.
- [CrossRef] [PubMed] [Google Scholar]







