Translate this page into:
Hemodialysis: The Life Boat for AKI Patients in the COVID Cytokine Storm
Corresponding author: Dr. Eesha Shukla, Room 10, Girls PG Hostel, SRN Hospital, Prayagraj, Uttar Pradesh - 211 001, India. E-mail: eeshashukla95@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shukla E, Narain U, Gupta A. Hemodialysis: The Life Boat for AKI Patients in the COVID Cytokine Storm. Indian J Nephrol. 2024;34:237–40. doi: 10.4103/ijn.ijn_96_23
Abstract
Background:
Interleukin-6 (IL-6), a biomarker of hyperinflammatory immune response, can be used to determine the severity of coronavirus disease 2019 (COVID-19) in patients with multi-organ involvement requiring critical care. The aim of our study is to understand the utility of hemodialysis, not only in terms of reducing renal burden, but also improving the outcome by tackling the COVID cytokine storm syndrome.
Materials and Methods:
In this prospective, observational study, 126 patients admitted to the COVID intensive care unit (ICU) wards were treated with hemodialysis for acute kidney injury (AKI). Patients’ routine baseline blood parameters were evaluated. IL-6 was measured predialysis in all patients and on the day of discharge in the patients who survived.
Results:
Out of total 126 patients, 79 were survivors and 47 were nonsurvivors. Among nonsurvivors, majority were older (P = 0.009). Both the groups had a higher percentage of males (78.72% and 55.69% in survivors and nonsurvivors, respectively). Mean neutrophil lymphocyte ratio (NLR) and D-dimer level were significantly higher in nonsurvivors compared to survivors (P < 0.001). Mean serum urea, creatinine, and IL-6 levels were significantly greater in nonsurvivors (P < 0.001). Mean number of hemodialysis sessions received by survivors was higher. The curve between delta IL-6 and delta serum creatinine for survivors showed a significant positive association (r = 0.819, P < 0.001).
Conclusion:
Our study establishes IL-6 as a poor outcome predictor in COVID ICU patients with AKI. It also emphasizes the use of hemodialysis as a cost-effective lifesaving therapeutic interventional modality to not only improve the renal outcome, but also curb the cytokine storm by reducing IL-6 levels.
Keywords
AKI
COVID
cytokine storm
hemodialysis
Introduction
The term “cytokine storm,” first used 30 years back by Ferrara et al.1 for graft versus host disease post-allogeneic hematopoietic stem cell transplantation, acknowledges the immune system as a double-edged sword. Rewinding the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic, keeping in mind the role of unhinged hyperactive immune response as a protector turned destroyer, helps us address the question as to why some patients infected with coronavirus disease (COVID) merely had symptoms of common cold, whereas others developed acute respiratory distress syndrome (ARDS) along with multi-organ failure and eventually succumbed to death.
Various studies have established angiotensin converting enzyme-2 (ACE-2) as the functional receptor of SARS-CoV-2.2 This explains the vulnerability of lung alveolar cells, brush border epithelium of proximal renal tubule, cardiac, gastrointestinal, and endothelial tissues to the virus. The binding of S protein to ACE-2 leads to production of the inflammatory cytokines interleukin (IL)-1, IL-6, IL-10, and tumor necrosis factor-alpha (TNF-alpha), further leading to hypercytokinemia, diffuse endothelialitis, and eventually multi-organ damage.3 This theory was further strengthened by the good response of critically ill patients to glucocorticoids when compared to those who received usual care or placebo.4
IL-6 has been implicated as the flagbearer of inflammatory response as it promotes T-helper 2 response, T-helper 17 differentiation, and antibody production.5,6
Studies estimate that around 25% of the patients hospitalized with COVID-19 developed kidney injury and more than half of those admitted in the intensive care unit (ICU) for acute kidney injury (AKI) required dialysis.7 The aim of this study was to evaluate the role of hemodialysis as an interventional modality in COVID patients with acute renal insult and whether or not it helped with the clearance of IL-6.
Materials and Methods
Study design
This was a prospective, observational study. The participants included were patients admitted to COVID wards in Swaroop Rani Nehru Hospital, Prayagraj, India, from July 2020 to January 2022.
Primary objective
Our primary objective was to determine whether hemodialysis assisted in the elimination of IL-6 and its role as an interventional technique in COVID patients with acute kidney injury.
Inclusion criteria
We included all patients aged >18 years who had AKI AKI stage 3 according to KDIGO (Kidney Disease Improving Global Outcomes) guideline 2012.
Patients aged <18 years, those with a history of chronic kidney disease (CKD) and those treated with nephrotoxic drugs such as remdesivir and amphotericin B were excluded.
Study procedure
One hundred and twenty-six patients who were admitted to COVID wards and underwent hemodialysis were included in the study. Patients were tested for COVID using RT-PCR (Reverse transcription-polymerase chain reaction) or Truenat. Patients were categorized into survivors and nonsurvivors on the basis of their outcome. AKI group included patients with AKI stage 3 of KIDGO-2012 guideline. Data on patients’ history and comorbidities (hypertension, diabetes mellitus, cardiovascular, pulmonary, or malignancy) were collected and baseline investigation parameters like complete blood counts, liver function test, kidney function test, and glycated hemoglobin (HbA1c) were tested on the day of admission. Patients were monitored for urine output, blood pressure, respiratory rate, pulse rate, oxygen saturation, KFT, (Kidney function test) and other parameters daily. Based on the changes in kidney function and urine output, patients were subjected to hemodialysis using Fresenius Polysulfone membrane (FX-8) with an effective surface area of 1.4 m2 and ultrafiltration coefficient of 12 (ml/h × mmHg). Serum ferritin and C-reactive protein (CRP) levels on the day admission were correlated with the outcome of patients. IL-6 levels were measured from Tejas micro diagnostic center, Prayagraj, using Maglumi in vitro chemiluminescence immunoassay. The estimated molecular weight of IL-6 was 22–27 kDa. IL-6 was measured in both the groups, survivors and nonsurvivors, on the day of admission and again only in the survivor group on the day of discharge from the COVID ward.
Statistical analysis
The categorical variables were in the form of number and percentage (%). Quantitative data were presented as the mean ± standard deviation (SD). The analysis was done with the use of Statistical Package for Social Sciences (SPSS) software (ver. 21.0; IBM, Chicago, IL, USA). For statistical significance, a P value of less than 0.05 was considered statistically significant.
Ethical consideration
Institutional ethics committee – human research approved the study. Study procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000. The protocol was approved by the ethics committee (registration no. ECR/922/Inst./UP2017 issued under rule 122DD/of the Drugs and Cosmetics Rule 1945) of Moti Lal Nehru Medical College, Prayagraj, Uttar Pradesh, India.
Results
A total of 126 COVID-positive patients, who underwent hemodialysis for AKI, were selected. They were divided into survivors (n = 79) and nonsurvivors (n = 47) based on their outcome. On comparing baseline characteristics, it was found that nonsurvivors were older with a mean age of 57.49 years, while the survivors had a mean age of 45.19 years (P = 0.009). Similarly, the percentage of males was higher in nonsurvivors (78.72% [37/47]) versus survivors (55.69% [44/79]) (P < 0.001). The distribution of smokers and alcoholics among survivors and nonsurvivors was nonsignificant as shown in Table 1.
| Survivors (n=79) | Nonsurvivors (n=47) | P | |
|---|---|---|---|
| Demographics | |||
| Age (years) | 45.19±13.32 | 57.49±15.51 | <0.001 |
| Males | 44 (55.69%) | 37 (78.72%) | 0.009 |
| BMI (kg/m2) | 20.48±3.72 | 23.13±3.78 | <0.001 |
| Smoker | 30 (37.97%) | 24 (51.06%) | 0.151 |
| Alcoholic | 23 (29.11%) | 18 (38.29%) | 0.287 |
| Hematological parameters | |||
| Hemoglobin (g/dl) | 9.92±2.35 | 9.31±2.44 | 0.169 |
| NLR | 6.63±3.45 | 14.16±6.07 | <0.001 |
| Platelet count (lakhs/mm3) | 1.93±0.37 | 1.33±0.54 | <0.001 |
| D-dimer (mg/l) | 1.72±1.71 | 6.49±2.86 | <0.001 |
| Kidney function tests | |||
| Blood urea (mg/dl) | 146.82±40.21 | 232.28±74.03 | <0.001 |
| Serum creatinine (mg/dl) | 7.16±1.41 | 10.41±4.42 | <0.001 |
| IL-6 (pg/ml) | 142.57±45.52 | 356.95±78.21 | <0.001 |
| No. of hemodialysis sessions | 2.53±0.58 | 1.76±0.99 | <0.001 |
BMI=body mass index, COVID=coronavirus disease, IL-6=interleukin-6, NLR=neutrophil lymphocyte ratio
Hematological parameters showed higher mean hemoglobin level in survivors (9.92 mg/dl), whereas in nonsurvivors, the mean level was 9.31 mg/dl (P = 0.169). Mean platelet count was 1.93 and 1.33 lakhs/mm3 in survivors and nonsurvivors, respectively (P < 0.001). Mean neutrophil lymphocyte ratios (NLRs) were 6.63 ± 3.45 and 14.16 ± 6.07 and mean D-dimer levels were 1.72 and 6.49 mg/l in survivors and nonsurvivors, respectively (P < 0.001).
On evaluation of kidney function test, mean blood urea level in survivors was found to be lesser (146.82 ± 40.21 mg/dl) compared to nonsurvivors (232.28 ± 74.03 mg/dl) (P < 0.001). Mean serum creatinine level was significantly higher in nonsurvivors (10.41 ± 42 mg/dl) in contrast to survivors 7.16 ± 1.41 mg/dl (P < 0.001). In nonsurvivors, the mean IL-6 level was significantly higher (356.95 ± 78.21 pg/ml), whereas in survivors, the mean level was 142.57 ± 45.52 pg/ml (P < 0.001) as shown in Figure 1. Mean IL-6 level postdialysis as measured on the day of discharge from the COVID ward among survivors was 63.77 ± 32.64 pg/ml (P < 0.001) as shown in Table 2.
| Predialysis | Postdialysis | P | |
|---|---|---|---|
| Creatinine (mg/dl) | 7.16±1.41 | 5.86±3.22 | <0.0001 |
| IL-6 (pg/ml) | 142.57±45.52 | 63.77±32.64 | <0.0001 |
IL-6=interleukin-6, KFT=kidney function test
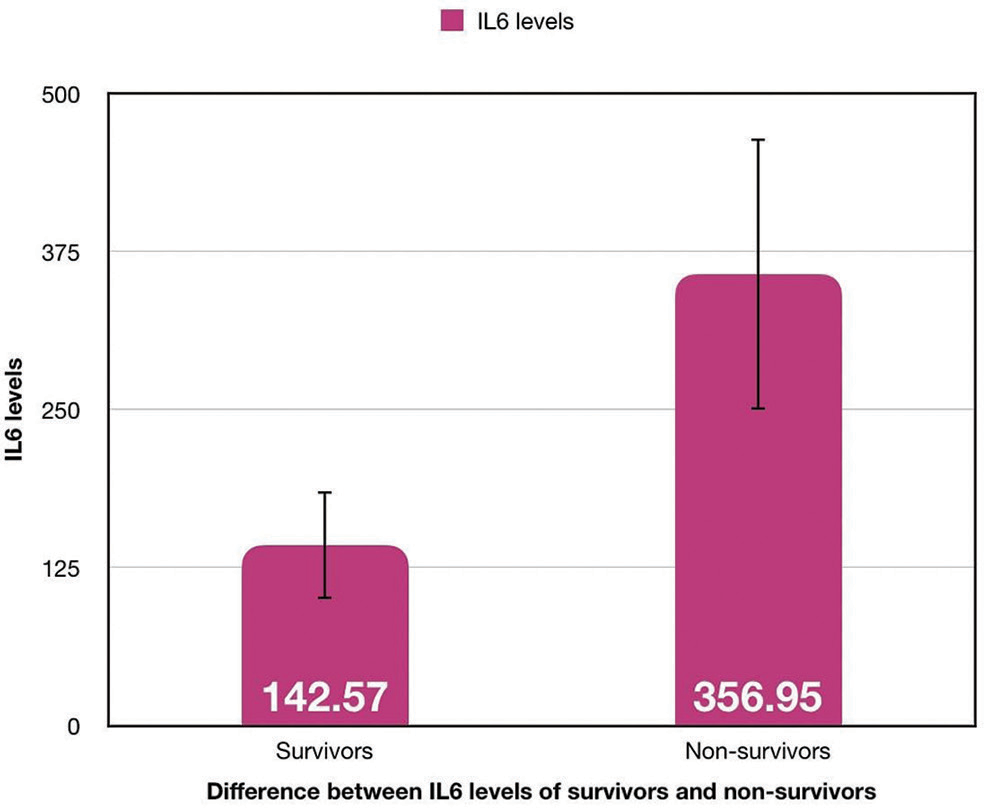
- Comparison of IL-6 levels (pg/ml) between COVID survivors and nonsurvivors. COVID = coronavirus disease, IL-6 = interleukin-6.
The mean number of hemodialysis sessions received by survivors was greater (2.53 ± 0.58) in comparison to nonsurvivors (1.79 ± 0.99) with a significant P value (<0.001).
The curve between delta IL-6 (difference between predialysis and on-discharge IL-6 level) and delta serum creatinine (difference between predialysis and on-discharge serum creatinine) for survivors showed a significant positive association (r = 0.819, P < 0.001), as shown in Figure 2.
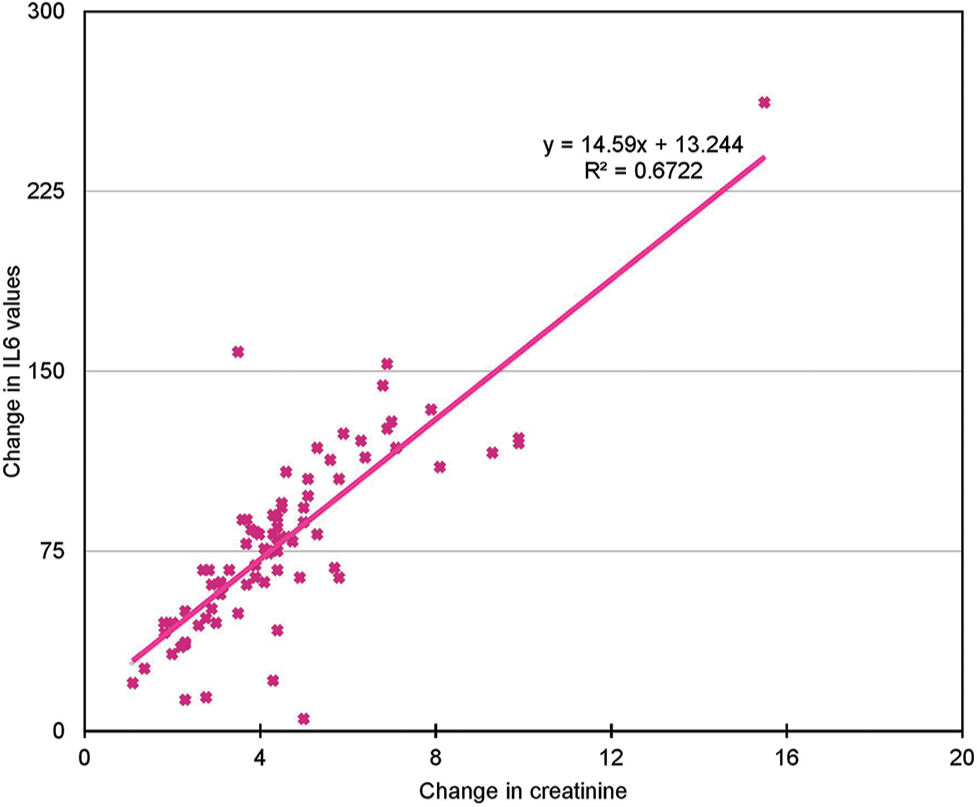
- Association curve between delta serum creatinine (mg/dl) and delta IL-6 (pg/ml) in COVID hemodialysis survivors (r = 0.819). COVID = coronavirus disease, IL-6 = interleukin-6.
Discussion
The hyperinflammatory process referred to as hypercytokinemia or cytokine storm lies at the heart of SARS-CoV-2 and mitigates its course of action deciding who will survive and who will not among those infected. Yet so far, we have been unable to come up with a clear-cut definition of COVID cytokine storm and the treatment is still running a trial and error course.
Considering IL-6 as the harbinger of COVID-CSS, we see a significant difference in the mean levels between survivors and nonsurvivors. Similar results were obtained in various studies showing elevated serum IL-6 levels ranging from 100 to 1000 pg/ml in patients with severe disease.8,9
Nonsurvivors had significantly higher mean age in comparison to survivors. Higher mortality in older patients can be attributed to more severe COVID-19, vexing the inflammatory response.10 Similarly, Biswas et al.11 observed increased mortality in older patients, most of them being males, which is consistent with the results of our study.
Characteristically decreased lymphocyte counts are observed in cases of COVID-CSS, which is in contrast to other cytokine storm disorders, either due to increased destruction of T lymphocytes or tissue infiltration.12 Our study mirrors similar results with increased NLR among nonsurvivors with a significant result.
The increased frequency of thromboembolic events pertaining to endothelialitis in COVID-CSS compared to other CSS13 plausibly explains the significantly high D-dimer levels in nonsurvivors in comparison to survivors.
Interplay between increased cytokine uproar and decreased kidney function shows the co-association of these factors in COVID patients, culminating into patient requiring hemodialysis. Our results were similar in terms of higher mean serum urea and creatinine level in non-survivors in comparison to survivors (P < 0.001). Also, patients in the survivors group received significantly greater number of hemodialysis sessions compared to nonsurvivors (P < 0.001), which could be attributed to various factors such as severity of COVID, early or late presentation after being referred from a number of hospitals, duration of hospital stay, and so on.
Previously, studies have been done using specialized high and medium cut-off hemodialysis membranes in COVID patients with CKD for cytokine reduction.10,14 But our study uniquely shows a positive correlation (r = 0.819) with a decreasing trend of IL-6 levels and serum creatinine predialysis and on the day of discharge from COVID ICU in patients with AKI using polysulfone membrane-based hemodialysis. It points toward the idea that hemodialysis not only helps in reducing the renal burden, but also decreases the cytokine load and inflammatory insult without increasing the cost burden.
Conclusion
Our study reaffirms IL-6 as the flagbearer of COVID-CSS and as a strong mortality predictor of patients with multi-system involvement requiring critical care.
Conflicts of interest
There are no conflicts of interest.
References
- Cytokine storm of graft-versus-host disease: A critical effector role for interleukin-1. Transplantat Proc. 1993;25:1216-7.
- [PubMed] [Google Scholar]
- What are the most common respiratory diseases encountered in clinical practice? Results of a pilot study in 737 Indian patients. Eur Respir J. 2015;46:PA3864.
- [CrossRef] [Google Scholar]
- Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: A meta-analysis. JAMA. 2020;324:1330-41.
- [CrossRef] [PubMed] [Google Scholar]
- IL-6 in inflammation, immunity, and disease. Cold Spring Harb Perspect Biol. 2014;6:a016295.
- [CrossRef] [PubMed] [Google Scholar]
- Blood serum levels of IL-2, IL-6, IL-8, TNF-alpha and IL-1beta in patients on maintenance hemodialysis, membranes. Cell Mol Immunol. 2006;3:151-4.
- [PubMed] [Google Scholar]
- Acute kidney injury in critically ill patients with COVID-19. Intensive care medicine. 2020;46:1339-48.
- [CrossRef] [PubMed] [Google Scholar]
- Elevated levels of IL-6 and CRP predict the need for mechanical ventilation in COVID-19. J Allergy Clin Immunol. 2020;146:128-36.
- [CrossRef] [PubMed] [Google Scholar]
- A dynamic COVID-19 immune signature includes associations with poor prognosis. Nat Med. 2020;26:1623-35.
- [CrossRef] [PubMed] [Google Scholar]
- Fluctuations in interleukin-6 levels during hemodialysis sessions with medium cutoff membranes: An analysis on COVID-19 case series. Blood Purif. 2022;51:953-8.
- [CrossRef] [PubMed] [Google Scholar]
- Association of sex, age, and comorbidities with mortality in COVID-19 patients: A systematic review and meta-analysis. Intervirology. 2021;64:36-47.
- [CrossRef] [PubMed] [Google Scholar]
- Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: An updated analysis. Thromb Res. 2020;191:148-50.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of high cut-off hemofilters in the removal of selected cytokines in patients during septic shock accompanied by acute kidney injury-preliminary study. Med Sci Monit. 2016;22:4338-44.
- [CrossRef] [PubMed] [Google Scholar]







