Translate this page into:
Hemorrhage from lumbar artery following percutaneous renal biopsy
Address for correspondence: Dr. R. Ram, Department of Nephrology, Sri Venkateswara Institute of Medical Sciences, Tirupati, Andhra Pradesh, India. E-mail: ram_5_1999@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
We present a 58-year-old lady who underwent ultrasound-guided renal biopsy for suspected acute glomerulonephritis. Within minutes, the radiologist noticed an echogenic band around left kidney and in the muscular planes. Computerized tomography revealed focal active contrast extravasation from arcuate or interlobular artery in lower pole of left kidney and lumbar artery at third lumbar vertebra. The bleeding vessel was occluded with gelfoam.
Keywords
Kidney biopsy
hemorrhage
lumbar artery
Introduction
Clinically significant complications following kidney biopsies range from 0.4%[1] to 8.1%.[2] Peri-renal hematomas requiring blood transfusions are encountered in 1-5% cases.[3] The incidence of major complications is, fortunately, lower. Puncture of other organs and arteries is exceptional. Laceration of the lumbar artery during renal biopsy has been reported only in four instances.[4567] A solitary report of mesenteric artery laceration has been the exception.[8]
Case Report
A 58-year-old lady presented with swelling of face that progressed to involve abdomen and feet, along with oliguria, cola colored urine and breathlessness on minimal exertion. On examination, she had puffiness of eyelids and swelling of feet. Pulse was 102 beats/min and blood pressure was 140/100 mmHg. Cardiovascular examination revealed left ventricular third sound and respiratory system examination revealed bilateral crackles in infrascapular areas. Investigations showed hemoglobin of 12.1 g/dl, platelet count 2.57 lakhs/cumm, random blood glucose 82 mg/dl, blood urea 88 mg/dl, serum creatinine 5.63 mg/dl, total serum proteins 7.8 g/dl, and albumin 4.0 g/dl. Urinalysis revealed albumin: +, red blood cells: 10–12/hpf, and red blood cell casts. Ultrasound abdomen showed normal sized kidneys. The 24 h urine protein was 1.1 g, total cholesterol 258 mg/dl, antistreptolysin O >400 U/L, complement 3 435 mg/L (reference range: 1032–1495 mg/L), and complement 4 150 mg/L (reference range: 167–385 mg/L).
Patient was subjected to a renal biopsy with a 16 gauge automated spring-loaded biopsy gun with length for sample notch being 1.6 cm and a possible penetration depth of 22 mm (Bard Biopty Systems, USA). It was done under real-time ultrasound guidance. The left kidney was biopsied. After first specimen, the check ultrasound was normal. After second pass, the patient complained of pain from the biopsy site to the left flank and anterior abdomen. The radiologist noticed the appearance of an echogenic band around left kidney and in the muscular planes. A computerized tomography scan of abdomen revealed left perinephric collection of 1200 ml and heterogenous collection in left lumbar region [Supplementary Figure 1]. Angiogram revealed a focal active contrast extravasation from arcuate or interlobular artery in lower pole of left kidney and from lumbar artery at third lumbar vertebra [Supplementary Figure 2]. Her blood pressure fell to 80/60 mmHg from the pre-biopsy reading of 140/100 mmHg, and the hemoglobin dropped to 8.1 g/dl. She was started on whole blood transfusion and inotropes. Within 1 h aortic, renal and lumbar artery angiogram was performed. Right femoral artery was cannulated with a Cordis 6.0F femoral sheath, into which a Judkin's diagnostic catheter 5.0F was passed. Into this catheter, floppy percutaneous transluminal coronary angioplasty guidewire, 0.014 inch in diameter and 300 cm in length was passed to reach the bleeding site in the lumbar artery. The bleeding site was approximately 10.5 cm away from the vertebral column [Figure 1 and Supplementary Figure 3]. Over this guidewire, a micro catheter, 2.25F and 130 cm in length (AsahiIntecc) was passed [Supplementary Figure 4]. Into this micro catheter, Gelfoam was injected so as to occlude the bleeding site [Supplementary Figure 5]. The blood pressure improved to 130/80 mm Hg immediately after the procedure. She did not require any blood transfusions. The hematoma remained palpable for 5 weeks. The light and immunofluorescence microscopy confirmed the diagnosis as postinfectious glomerulonephritis.
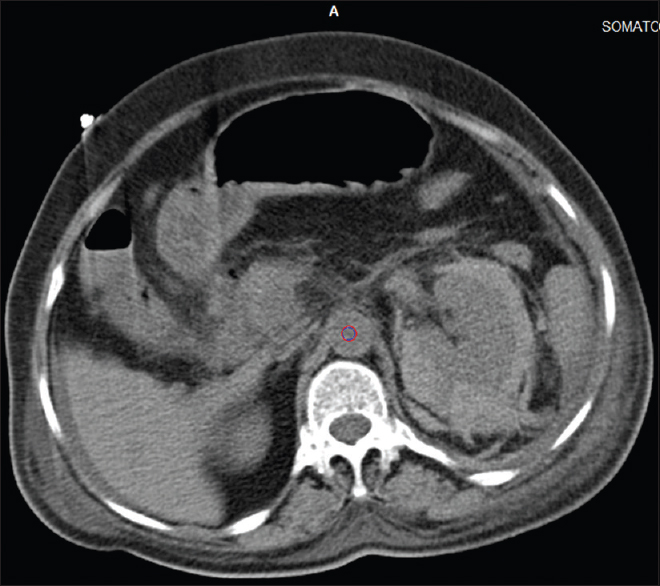
- Computed tomography scan abdomen: Bleeding from lumbar artery
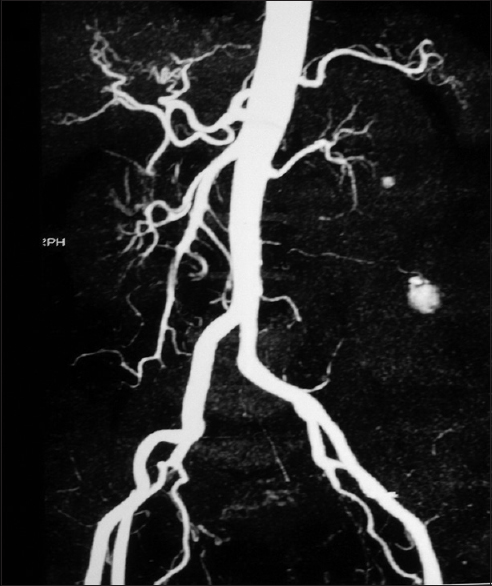
- CT showing angiogram: Bleeding from lumbar artery
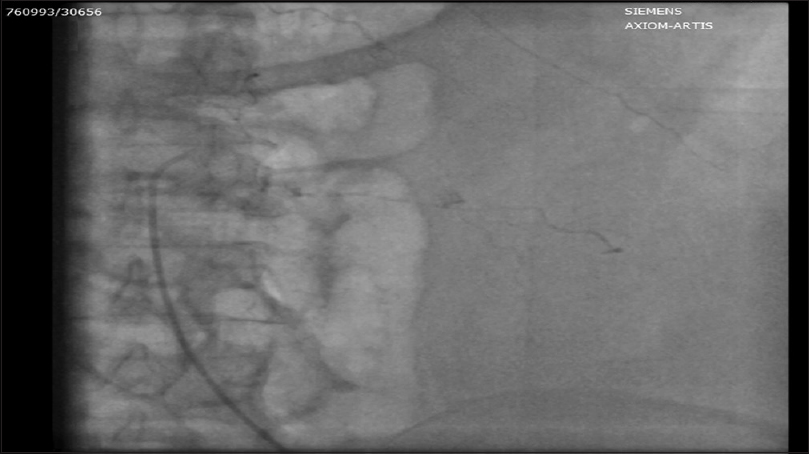
- Angiogram: Bleeding from lumbar artery

- Renal angiogram: No bleeding in the kidney

- 2.25F micro catheter introduced into lumbar artery

- Lumbar artery embolized with gelfoam
Discussion
Lumbar arteries are in series with the posterior intercostal arteries. Usually, four on each side [Figure 2], they arise posterolaterally from the aorta opposite the lumbar vertebrae. A fifth, smaller pair occasionally from the median sacral artery but lumbar branches of the iliolumbar arteries usually takes their place. The lumbar arteries posterolaterally on the four upper lumbar vertebral bodies, behind the sympathetic trunks, to intervals between the lumbar transverse processes and continue into the abdominal wall. The right arteries pass posterior to the inferior vena cava; the upper two right and first left are also posterior to the corresponding crus. Arteries of both sides pass under tendinous arches (which span the lateral cavities of the vertebral bodies) for attachment of psoas major, proceeding posterior to the muscle and the lumbar plexus. They then cross the quadratus lumborum, the upper three posterior, the last usually anterior to it. At its lateral border, they pierce the posterior aponeurosis of the transversus abdominis, advancing between it and the internal oblique. They anastomose with one another and the lower posterior intercostal, subcostal, iliolumbar, deep circumflex iliac and inferior epigastric arteries. As the upper three pairs of lumbar arteries pass behind the quadratus lumborum, they are at risk injury from the renal biopsy needle.[2]
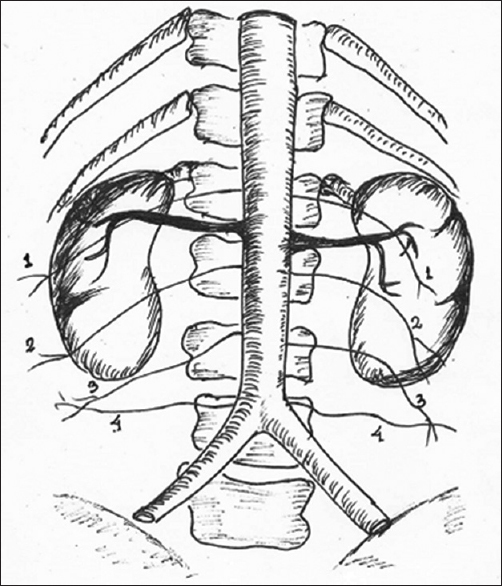
- Anatomy of lumbar arteries (1–4)
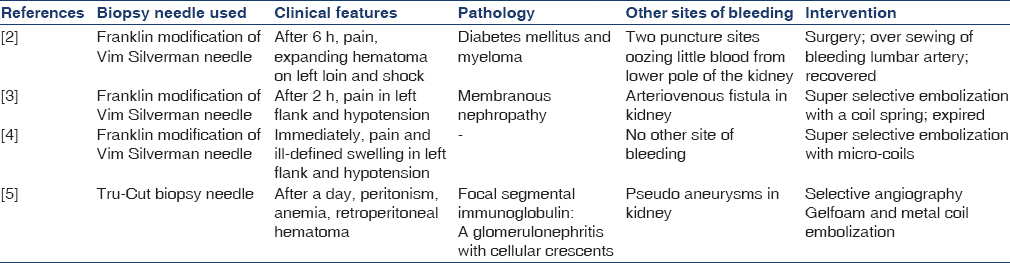
In the two previous reports [Table 1], the presence of bleeding sites and arteriovenous fistula in kidney has misled and the laceration of the lumbar artery was missed. There was a delay of 20 h and 48 h in these two patients respectively before the laceration of the lumbar artery was recognized.
Embolization of lumbar artery is fraught with the risk of infarction of the spinal cord. The artery of Adamkiewicz (or great anterior radiculomedullary artery or arteria radicularis anterior magna) is the dominant thoracolumbar segmental artery that supplies the spinal cord. This artery has a variable origin; but most commonly arises[7] on the left (~80%) at the level of 9th–12th intercostal artery (~70%). It arises from the radiculomedullary branch of the posterior branch of the intercostal or lumbar artery, which arises from the thoracic or abdominal aorta respectively.[9] The variations of its origin include from lumbar arteries at the level of L1 or L2 (10%), intercostal arteries at the level of T5 to T8 (15%) and arises on the right (20%). The injection of Gelfoam and placement of coils should be done only after considering all these variations in the origin of this artery. The use of liquid embolization materials is also contraindicated due to higher risk of spinal cord injury.[7] The lumbar artery embolization has been reported to have caused infarction of paraspinal muscles in two patients.[10]
Bleeding from lumbar artery is a rare complication but can be successfully managed with prompt recognition and intervention.
Acknowledgments
Figure 2 is redrawn from reference 2 by Dr. Amitabh Jena, Additional Professor, Surgical Oncology, Sri Venkateswara Institute of Medical Sciences, Tirupati.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Health and Public Policy Committee. American College of Physicians: Clinical competence in percutaneous kidney biopsy. Ann Intern Med. 1998;108(2):301-302.
- [Google Scholar]
- Complications of percutaneous renal biopsy: An analysis of 1,000 consecutive biopsies. Clin Nephrol. 1975;4:223-7.
- [Google Scholar]
- Complications of the percutaneous kidney biopsy. Adv Chronic Kidney Dis. 2012;19:179-87.
- [Google Scholar]
- Severe haemorrhage from a lumbar artery as a complication of percutaneous renal biopsy. Postgrad Med J. 1985;61:69-70.
- [Google Scholar]
- Massive hemorrhage from a lumbar artery following percutaneous renal biopsy. Am J Kidney Dis. 1986;7:250-3.
- [Google Scholar]
- Embolic control of lumbar artery hemorrhage complicating percutaneous renal biopsy with a 3-F coaxial catheter system: Case report. Cardiovasc Intervent Radiol. 1991;14:175-8.
- [Google Scholar]
- Embolization of lumbar artery due to retroperitonal bleeding following renal biopsy. Nephrol Dial Transplant. 2005;20:820-2.
- [Google Scholar]
- Laceration of a mesenteric artery: Unusual complication of percutaneous renal biopsy. South Med J. 1980;73:1413-4.
- [Google Scholar]
- MR angiography and CT angiography of the artery of Adamkiewicz: State of the art. Radiographics. 2006;26(Suppl 1):S63-73.
- [Google Scholar]
- Paraspinal muscle infarction. A painful complication of lumbar artery embolization associated with pathognomonic radiographic and laboratory findings. Radiology. 1976;119:609-13.
- [Google Scholar]







