Translate this page into:
Home Peritoneal Dialysis: Past, Present, and Future in India
Corresponding author: Georgi Abraham, Department of Nephrology, MGM Healthcare, Chennai, India. E-mail: abraham_georgi@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Rajesh AS, Abraham G, Mathew M. Home Peritoneal Dialysis: Past, Present and Future in India. Indian J Nephrol. doi: 10.25259/IJN_374_2024
Abstract
Since the initiation of home continuous ambulatory peritoneal dialysis (CAPD) in 1976, technological advancements have expanded the use of the therapy across the world. The disposable Y-set and newer solutions have made CAPD and automated peritoneal dialysis (APD) as the preferred renal replacement therapy across the world. Here, we describe the early years of experience of CAPD and APD, current state of treatment, and the future of this form of renal replacement therapy in India.
Keywords
Home peritoneal dialysis
advantages and adverse effects
penetration of CAPD
Introduction
Jack Moncrief and Bob Popovich initiated the first patient on continuous ambulatory peritoneal dialysis (CAPD) in 1975 in Austin, Texas, USA. Using a long stylet and a trocar, they implanted a Palmer catheter with cuffs to gain access to the peritoneal cavity and instilled dialysis fluid contained in a 2 L glass bottle.1 This technique allowed the maintenance of a continuous steady state with uremic solute clearance. Dimitrios Oreopoulos (Toronto) modified the technique using collapsible 2 L plastic bags and a spike system with a transfer set to instill the fluid into the peritoneal cavity with a permanently implanted Tenckhoff catheter with two cuffs, introduced in 1968 by Henry Tenckhoff.2 This modification led to the expansion of CAPD across the world. The introduction of the “Flush before Fill” technique by Dr Umberto Buoncristiani in the 1980s was the next major change, leading to a significant drop in the peritonitis rates from one episode every 18 to one every 40 patient months.3 The first peritoneal dialysis (PD) transfer system involved a straightforward connection mechanism, such as spike or luer lock, to connect the dialysis catheter to the dialysate solution bag. This design was simple but had a higher risk of contamination due to the frequent need for manual connections and disconnections. This was called the O-set, and the transfer set was reused after sterilization by bleach. To address the high risk of peritonitis associated with O sets, the Y-set system, which reduced the number of manual connections required, was developed, followed by the twin bag systems. These innovations lowered the incidence of peritonitis significantly.
The early days of CAPD in india
Permanent PD catheters, dialysis bag, and personnel with experience in CAPD were not available in India until 1991, when one of us (GA) initiated CAPD using the Y technique in Chennai on an elderly diabetic patient with severe left ventricular failure on maintenance hemodialysis.4 All materials had to be imported. The Government had no awareness and information about CAPD, and imposed hefty customs duties on the import of PD bags and disposables, raising the already high cost. Chronic PD was not favored by many nephrologists in India, who believed that a tropical climate would lead to increased rates of peritonitis.5 A representation by a couple of nephrologists to the Health Ministry paved the way for including import licenses without customs duty for dialysis fluid in 2 L collapsible bags, accessories, and catheters by 1994. A home portable cycler was used for the first time in 1997 for a patient in Chennai.6 Several global leaders in PD, including Dimitrios Oreopoulos, Joanne Bargman, Ram Gokul, Ramesh Khanna, Peter Blake, Norbert Lameire, Stephen Vas, Karl Nolph, and Simon Davis, supported the growth of PD in India through their extensive travels to many centers in India and conducting PD colleges and Continuing Medical Education (CME) schemes.
The establishment of the Peritoneal Dialysis Society of India (PDSI) in 1997 acted as a platform to expand PD in other South Asian countries. The Indian Journal of Peritoneal Dialysis (IJPD) has been published biannually since 2005 and disseminates PD-related science. One of the highlights was the Asian PD chapter meetings in Hyderabad (2005) and New Delhi (2023). A unique feature of the annual meetings of PDSI are the nurses and technicians’ sessions, which increases the pool of health workers trained in PD.7
Current practices and infection control
Most patients perform 2 L exchanges three times a day, and some do not instill fluids into the peritoneal cavity at night, leaving it dry. Most patients on 3 L exchanges per day showed a Kt/V of 1.67 and a two-year survival rate of 60% with a normalized protein equivalent of nitrogen appearance of 0.73–0.80 g/kg/d.7 In the authors’ experience, anuric patients with large body surface area require 4 L exchanges a day.
The access to the peritoneal cavity by a permanent flexible swan neck Tenckhoff catheter with either single or double cuff is the authors’ choice, since in their experience this has reduced the incidence of exit site infection (ESI).8 Other practitioners use a straight catheter as well with good results. In the initial years, PD catheter placement was done by surgeons, which led to significant delays since they did not prioritize this procedure. Over the last ten years, however, many nephrologists have developed proficiency in PD catheter placement, and many centers include PD catheter placement as part of nephrology training program. The application of mupirocin or gentamycin cream at the exit site, along with the fixation of the catheter to the anterior abdominal wall, also reduces ESI.9 In a small subgroup of patients with improper exit site care and uncontrollable diabetes mellitus, ESI and tunnel infections (TI) are seen [Figure 1].10 A cheap and affordable swan neck permanent PD catheter with peel away implantation set was developed by one of the authors of this paper (GA) [Figure 2]. One hundred of these catheters were donated for the African program at the World Congress of Nephrology at Cape Town in 2015. A multicentered prospective, uncontrolled, open-label, observational study was conducted in 21 centers representing all geographical regions of India between April 2010 and December 2011 to evaluate the pattern of PD-related peritonitis in India. A total of 244 patients were enrolled in the study from 21 centers. A total of 85 samples (35.3%) were culture positive, with 38 (44.7%) in the monsoon season, followed by 23 (27.1%) in the post-monsoon, 18 (21.2%) during winter, and 11 (12.9%) during summer. The highest culture positivity rate (72.7%) was observed with the automated culture technique. Organisms isolated were gram-negative in 47.8%, gram-positive in 36.7%, fungal in 13.3%, and Mycobacterium tuberculosis in 2.2%.11 The high culture negativity rates remain worrisome because it prevents the institution in providing appropriate therapy and also does not allow us to understand the current pattern of organisms and their sensitivity patterns, which is critical to the development of local protocols to guide empirical antibacterial therapy. It highlights the need for improvement in collection, storage, and culture techniques. Many of these issues have been covered in a recent book edited by GA, Diagnosis and Management of Complications of Peritoneal Dialysis-Related Peritonitis (Springer).12
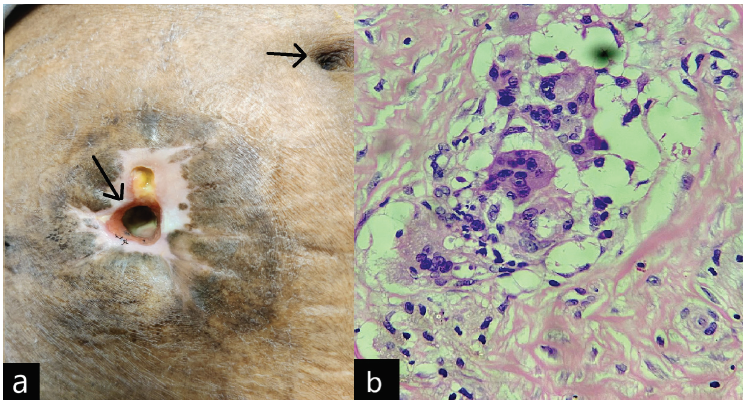
- (a) Catheter tunnel exit site (black arrows), (b) Histology showing foreign body granuloma.
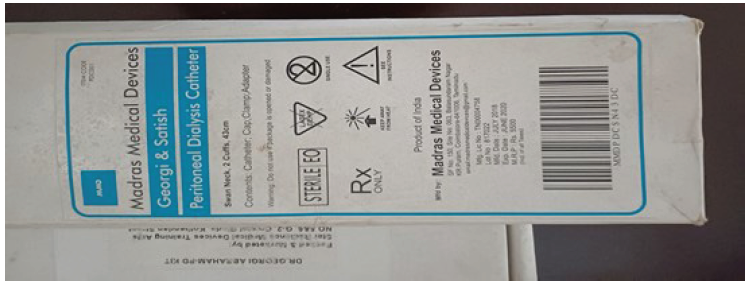
- Georgi and Satish swan neck peritoneal dialysis with peel away sheath.
Barriers to PD adoption
For the last 20 years, PD fluid bags have been manufactured in India. Only two companies are currently marketing PD bags in India. It is a pity that the local manufacturing does not extend to the production of plastic bags, which are still imported and constitute the bulk of the costs.
There is widespread assumption that PD is more expensive than hemodialysis (HD) in many developing countries, including India. This premise is based on weekly assumptions, however. A health economic study from India showed that the quality-adjusted life years (QALYs) lived per person on PD and HD was estimated to be 3.3 and 1.6, respectively. The authors concluded that a PD-first policy was cost-saving compared to an HD-first policy from a societal perspective.13 However, if only the direct costs are considered, the PD-first policy would be cost-effective only if the price of PD consumables can be brought down from its current market price, which is possible through strategic purchase by the government, which would be the major PD provider.
Of the various osmotic agents used for PD, the overwhelming majority continue to depend on dextrose-containing PD solutions, with a minority using Icodextrin.14 Patients during training for either CAPD or APD are advised to use the 2 L bags as per their ultrafiltration and solute removal capacity. Biocompatible bicarbonate- or amino acid-containing solutions are expensive and not available in India.
A major challenge faced by patients in the acceptance and outcomes of PD is the perceived inaccessibility to the mother unit (MU). With a dedicated PD team of nephrologists, technicians, and nurses, a regular home visit protocol has enabled the Hyderabad group to develop a unique PD remote monitoring system.15 Patients’ access to their MU round-the-clock improved PD outcomes, especially in rural areas. Nayak et al. found better patient survival rates in rural areas using short messaging services and inexpensive digital cameras.16 There was no difference in the rate of peritonitis among the groups.
Patient outcomes and survival rates
There are limited data on patient outcomes on PD in India. A multicentered (supervised by four nephrologists) study on PD, predominantly CAPD, examined technique survival at three years and above.17 Of the 209 patients included in the study, 150 had >3 years survival. Essentially, the study showed that nondiabetics, average transporters, nonsmokers with good nutritional status, and those with preserved hemoglobin (>Hb 11 g/dL), low peritonitis rate, >1 L/day ultrafiltration volume survived for over three years (76.6% at three years). Those patients who were on single (lifetime) payment for dialysis (provided by industry, see below) and those receiving full reimbursement survived longer than those who paid every month for dialysis.17
CAPD is particularly relevant for the pediatric population with kidney failure, given the shortage of pediatric HD in India. Kamath et al. initiated 30 children on chronic peritoneal dialysis (CPD) from January 2014 to December 2017. Despite limitations and challenges, the authors concluded that CAPD is feasible in young children with low body weight.18
A survey of 265 nephrologists in South Asia in 2009 reported that the factors preventing nephrologists from delivering PD were lack of appropriate training, lower reimbursement, poor infrastructure, and affordability. Over 80% felt that poor reimbursement is a critical factor in the poor penetration of PD among nephrologists.18 The overwhelming cost component goes toward the purchase of PD fluid bags. At one time, the major PD fluid suppliers introduced innovative financing schemes. Patients were provided a continuous lifetime supply of PD bags and accessories on a one-time lump-sum payment. This scheme, however, was abandoned, perhaps as the providers found it to be loss-making.
Protein-energy malnutrition (PEM) remains a major problem in end-stage kidney disease (ESKD) patients in general and amongst PD patients in particular in India. The general prevalence of PEM is reported to be 42–77% in developing countries, including India. It is strongly associated with morbidity and mortality. The prevalence of malnutrition amongst patients on PD was found to be 45.3% (95%CI; 29.5–62.1) higher as compared to hemodialysis group (43.1%, 95% CI; 32.2–54.7) followed by non-dialysis group (38.5%, 95% CI; 24.0–55.3). Males were predominantly affected by malnutrition as compared to females. Many communities in India are vegetarians, which often prevents optimal protein intake.19–21
Education
India has emerged as an important hub for education in PD. To expand PD to Africa and South Asian and East Asian regions, the International Society for Peritoneal Dialysis (ISPD) and the International Society of Nephrology (ISN) provided fellowship grants to aspiring doctors and nurses from Nigeria, Cameroon, Tanzania, Sudan, Kenya, the Democratic Republic of the Congo, Seychelles, Pakistan, Sri Lanka, Myanmar, Nepal, Iraq, Sultanate of Oman, and the UAE, who get hands-on exposure in many Indian centers, including ours.
In 2016, the Union Minister of Health and Family Welfare gave guidelines for rolling out PD to provide respite to kidney failure patients, particularly those living in remote areas, and enable them to have a better quality of life. He requested all the State/Union Territories governments to implement this program urgently and in full earnest.
Despite the many theoretical advantages of this treatment modality, unfortunately PD has stagnated in India. In fact, the absolute number of patients on this modality has come down over the last ten years. This is because of rapid growth in the number of HD facilities, the public finding of HD and the exclusion of PD, the continued perception of the high cost of PD, and reluctance on the part of nephrologists. The latter is partly linked to financial incentives, given that nephrologists stand to earn more from HD compared to PD.22-24 As a result, we urge the government and other partners to ensure uniform nephrologist reimbursement to remove any disincentive for this important therapy.
Conclusion
The future of home PD (CAPD, APD) as an kidney replacement therapy (KRT) resides with the appropriate training of young nephrologists, trained nurses, and technologists, creating awareness in the medical profession about the advantages of home PD as a suitable modality alongside policy and reimbursement reforms. Besides being the most appropriate KRT option for those living in remote rural areas with limited access to HD, PD is also appropriate for those with compromised cardiac function and HD access failures. The decline in the rate of peritonitis in-home PD patients and appropriate microbiological diagnosis with new technological applications are welcome and should be disseminated widely. The support provided by the central government and state government programs have increased the acceptance of home PD in public sector hospitals (medical college hospitals) in different parts of India. However, there is a need to streamline the continuous supply of dialysis fluid and accessories to prevent dropout with the help of the state governments.
Conflicts of interest
There are no conflicts of interest.
Reference
- Continous ambulatory peritoneal dialysis. Ann Intern Med. 1978;88:449-5.
- [CrossRef] [PubMed] [Google Scholar]
- A simple and safe technique for continuous ambulatory peritoneal dialysis (CAPD) Trans AM Soc Artif Intern Organs. 1978;24:484-7.
- [PubMed] [Google Scholar]
- CAPD trials and tribulations in establishing an effective therapy in India. J Renal Sci. 1999;2:26-8.
- [Google Scholar]
- How to set up a peritoneal dialysis program: Indian experience. Perit Dial Int. 1999;19:184-6. Available from: 10.1177/089686089901902S30
- [CrossRef] [PubMed] [Google Scholar]
- Advantages and disadvantages of automated peritoneal dialysis. Perit Dial Int. 1998;18:673.
- [Google Scholar]
- Are three exchanges suitable for Asian patients on peritoneal dialysis? Perit Dial Int. 2003;23:S37-9.
- [CrossRef] [PubMed] [Google Scholar]
- Oreopoulos natural history of exit-site infection (ESI) in patients on CAPD. Perit Dial Int. 1988;8:211-6.
- [Google Scholar]
- Chronic peritoneal dialysis in South Asia—challenges and future. Peritoneal Dialysis International. 2008;28:13-9. doi:10.1177/089686080802800103
- [PubMed] [Google Scholar]
- Access-related complications in peritoneal dialysis in developing countries. Advances in Ren Replace Ther. 2002;9:144-8.
- [CrossRef] [Google Scholar]
- Microbiology, clinical spectrum and outcome of peritonitis in patients undergoing peritoneal dialysis in India: Results from a multicentric, observational study. Indian J Med Microbiol. 2017;35:491-8.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and management of complications of peritoneal dialysis related peritonitis. Springer; 2023.
- Peritoneal dialysis-first initiative in India: A cost-effectiveness analysis. Clin Kidney J. 2021;15:128-35.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Ultrafiltration failure is a reflection of peritoneal alterations in patients treated with peritoneal dialysis. Front Physiol. 2018;20:1815.
- [CrossRef] [Google Scholar]
- Interference of maltose, icodextrin, galactose, or xylose with some blood glucose monitoring systems. Pharmacotherapy. 2007;27:1313-21.
- [CrossRef] [PubMed] [Google Scholar]
- Use of a peritoneal dialysis remote monitoring system in India. Perit Dial Int. 2012;32:200-4.
- [CrossRef] [PubMed] [Google Scholar]
- Predictors of long term survival on peritoneal dialysis in South India: A multicenter study. Perit Dial Int 2010:29-34.
- [Google Scholar]
- Clinical and dialysis outcomes of manual chronic peritoneal dialysis in low-body-weight children from a low-to-middle-income country. Perit Dial Int. 2020;40:6-11.
- [CrossRef] [PubMed] [Google Scholar]
- How to make peritoneal dialysis affordable in developing countries. Contrib Nephrol. 2009;163:243-9.
- [CrossRef] [PubMed] [Google Scholar]
- The effectiveness of protein supplementation on the nutritional management of patients on CAPD. Adv Perit Dial. 1989;5:177-80.
- [PubMed] [Google Scholar]
- Malnutrition and nutritional therapy of chronic kidney disease in developing countries: The Asian perspective. Adv Ren Replace Ther. 2003;10:213-21.
- [CrossRef] [PubMed] [Google Scholar]
- Estimates of malnutrition associated with chronic kidney disease patients globally and its contrast with India: An evidence based systematic review and meta-analysis. Clin Epidemiol Glob Health. 2021;21:100855. Available from: https://doi.org/10.1016/j.cegh.2021.100855
- [Google Scholar]
- Hemodialysis tunneled catheter-related infections. Can J Kidney Health Dis. 2016;3:2054358116669129.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Government support to peritoneal dialysis program in Kerala. Indian J Perit Dia. 2016;30:24. Available from: http://doi.org/10.15582/ijpd/2016/104081
- [CrossRef] [Google Scholar]







