Translate this page into:
Isolated renal mucormycosis in an immunocompetent child
Address for correspondence: Dr. L. Senthil Nayagam, SB Hospital, Medical College Road, Rajappa Nagar, Thanjavur - 613 007, Tamil Nadu, India. E-mail: lsnayagam@yahoo.co.in
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Isolated renal mucormycosis (IRM) in an immunocompetent child is extremely rare condition and carries a grave prognosis. We report an 18-month-old child with IRM who was managed successfully with amphotericin B and nephrectomy.
Keywords
Amphotericin B
children
isolated renal mucormycosis
Introduction
Mucormycosis is an invasive, opportunistic fungal infection seen in immunodeficient individuals. Renal involvement is usually a part of multi system involvement. Isolated renal mucormycosis (IRM) is a rare disease and is even rarer in children and immunocompetent individuals. We report a case of isolated, unilateral renal mucormycosis in an immunocompetent 18 month-old child. The child was managed successfully with nephrectomy and amphotericin B.
Case Report
An 18-month-old male child presented with 3 days history of fever, rigors and pyuria, 5 months prior to admission. He was born to non-consanguineous parents. The child is appropriately immunized for his age. He weighed 11 kg and had normal height for age also. Urine microscopy showed plenty of pus cells. Ultrasonogram (USG) showed a swollen left kidney. There was no obstruction or perinephric collection. Right kidney was normal. Urine culture grew Escherichia coli. He was treated with ceftriaxone for a week and the child recovered. The child had two similar episodes in the next 4 months. He was treated with oral cefixime and oral ciprofloxacin for a week each time by the pediatrician. He was referred to us for recurrence of fever and pyuria. At admission, the child was toxic with a temperature of 39°C, heart rate 142/min and respiratory rate 38/min and had a palpable, enlarged left kidney. Pertinent laboratory data included hemoglobin 13.8 g/dl; white blood cell count 14,900/mm3 (neutrophils 11,622 and lymphocyte 2980); serum creatinine 0.8 mg/dl; fasting blood glucose 79 mg/dl; and human immunodeficiency virus-negative. Urinalysis had a pH of 6.5, plenty of white blood cells and red blood cells. Urine and blood bacterial culture was sterile. Intravenous urogram and 99mTc ethylene dicysteine renal scintigraphy showed a non-functioning left kidney. USG continued to show swollen left kidney with perinephric stranding with suggestion of intra renal abscess formation along with a perinephric collection of size 4 cm × 3 cm. The child was not responding to piperacillin/tazobactum and amikacin. As the child continued to be toxic, surgical drainage of abscess was considered. During exploration, the left kidney was found be necrotic and hence left nephrectomy was done. The child continued to have fever in the postoperative period.
Histopathology report, received on the 3rd postoperative day, showed extensive necrosis and suppuration bordered by epitheloid cell granuloma along with interstitial inflammation by lymphocytes, plasma cells and neutrophils. The necrotic area shows numerous fungal elements which are broad non-septate with irregular branching consistent with mucormycosis [Figure 1]. A diagnosis of isolated left kidney mucormycosis was made. He was started on conventional amphotericin B at a dose of 1 mg/kg/d from the fourth postoperative day. The child tolerated amphotericin B well and became afebrile within the next 3 days. He was continued on amphotericin B for 4 weeks. He continues to thrive well and has normal weight for age. He did not have any recurrence of symptoms or any other opportunistic infection.
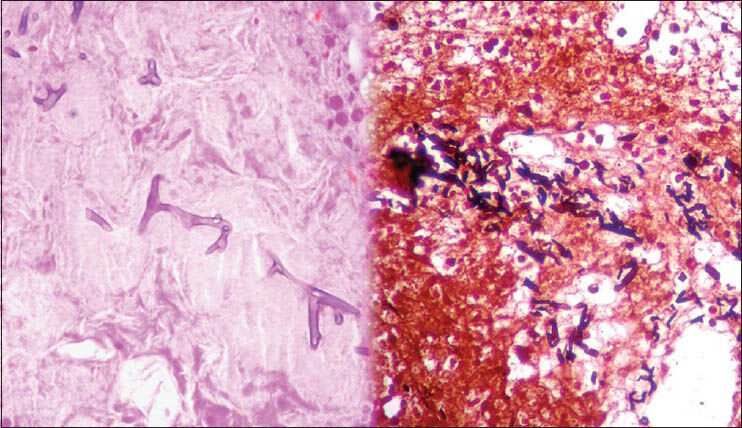
- H and E (left) and periodic acid Schiff (right) stained kidney tissue showing broad non-septate hyphae with right angle branching
Discussion
Invasive mucormycosis is an opportunistic fungal infection usually affecting patients with debilitating diseases such as cancer, transplant recipients, inherited and acquired immunodeficiencies, diabetes mellitus, diabetic ketoacidosis, malnutrition and penetrating wounds to the skin.[1] It has also been reported in patients receiving deferoxamine therapy, injection drug users and those with no apparent immune impairment. Our patient did not have any of the recognized risk factors. Use of multiple antibiotics prior to admission for the treatment of his urinary infection may have contributed to the development of mucormycosis.
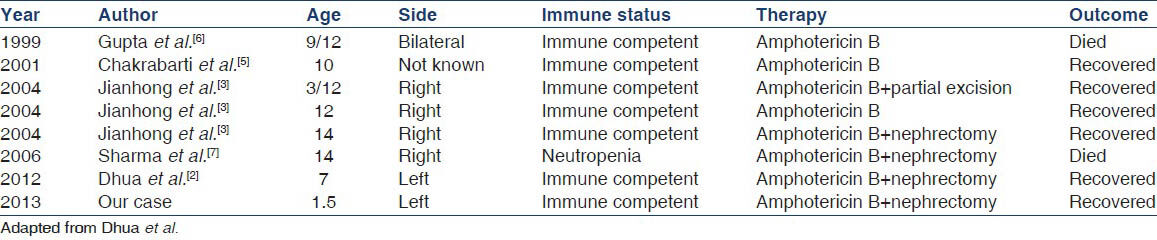
IRM is a very rare disease in children. Only eight cases have been reported in the English literature so far[2] (including our case) [Table 1]. Mucormycosis can be divided into five subtypes-rhinocerebral, pulmonary, gastrointestinal, cutaneous and disseminated.[3] In an extensive review of mucormycosis in pediatric patients by Roilides et al., the patterns of organ involvement identified were rhinocerebral (18%), pulmonary (16%), gastrointestinal (21%) and cutaneous (27%).[4] Renal involvement occurs in 19% of adult patients with disseminated disease.[5] However, such data in pediatric cases is lacking. Isolated renal involvement is very rare in children. Very few cases have been reported. Jianhong et al. reported three immunocompetent children with IRM all of whom recovered with surgery and anti-fungal therapy.[3] Dhua et al. have reported a case of IRM following a pyeloplasty in an immunocompetent child.[2] Local infection of the kidney did not progress to disseminated disease in any of these patients and it is not clear whether infection localized to the kidney is an intrinsic characteristic of IRM. Our patient had a bacterial pyelonephritis to begin with and superinfection with mucor later on.
Renal involvement may be unilateral or bilateral. The typical presenting symptoms are fever, flank pain, pyuria and hematuria. Bilateral involvement results in acute renal failure and is usually fatal. Computerized tomography (CT) typically shows enlarged kidneys with hypodense areas and is the imaging modality of choice. Pathologically there is vascular invasion with renal infarction and diffuse inflammatory infiltrates. Presence of irregularly shaped broad (10-20 μm) non-septate and right angle branching hyphae is important for diagnosis of mucormycosis. Unless the tissue is freshly inoculated into Sabouraud's agar culture identification would be difficult.[6]
Treatment involves combined surgical and medical management. Extensive debridement of necrotic tissue, which may involve nephroureterectomy along with amphotericin B is the treatment of choice. Overall survival for IRM is 65%.[2] There are isolated reports of successful management of IRM with amphotericin B alone.[58] However, combined amphotericin B with nephrectomy offers the best chance for cure.
Our patient recovered uneventfully after undergoing left nephrectomy and 4 weeks of amphotericin B. Even in immunocompetent children non-resolving pyelonephritis should raise the possibility of mucormycosis and immediate surgical debridement should be considered. IRM has a favorable outcome compared with other forms of invasive mucormycosis and may be considered as a separate disease entity.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Epidemiology and outcome of zygomycosis: A review of 929 reported cases. Clin Infect Dis. 2005;41:634-53.
- [Google Scholar]
- Isolated mucormycosis in a post-pyeloplasty kidney in an immuno-competent child. J Indian Assoc Pediatr Surg. 2012;17:132-4.
- [Google Scholar]
- Invasive zygomycosis in neonates and children. Clin Microbiol Infect (15 Suppl 5):50-4.
- [Google Scholar]
- Ten years experience in zygomycosis at a tertiary care centre in India. J Infect. 2001;42:261-6.
- [Google Scholar]
- Renal zygomycosis: An under-diagnosed cause of acute renal failure. Nephrol Dial Transplant. 1999;14:2720-5.
- [Google Scholar]
- Isolated renal mucormycosis: An unusual cause of acute renal infarction in a boy with aplastic anaemia. Br J Radiol. 2006;79:e19-21.
- [Google Scholar]
- Successful medical management of isolated renal zygomycosis: Case report and review. Clin Infect Dis. 1998;26:601-5.
- [Google Scholar]







