Translate this page into:
Kidney Health for Vulnerable: Challenges and Solutions
Address for correspondence: Dr. Priti Meena, Assistant Professor, Department of Nephrology, AIIMS, Bhubaneshwar, Odisha, India. E-mail: pritimn@gmail.com
-
Received: ,
Accepted: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
The global epidemic of kidney disease now affects over 850 million people.[1] The journey of a patient with chronic kidney disease (CKD) is fraught with many difficulties. Besides delayed diagnosis and limited access to healthcare, she has to face many anticipated and unanticipated hardships. The kidney health stakeholder community has come to realize that there is “many a slip between the cup and the lip” when it comes to caring for these patients. “Kidney health for all” has meaning only if all aspects of health-care delivery are considered.
This year’s 2023 World Kidney Day theme, “Kidney Health for All – Preparing for the Unexpected, Supporting the Vulnerable!” recognizes issues which are slowly becoming vital for the patients with kidney disease. In addition to pre-existing and, in many instances, deep-rooted social and economic inequities, this year’s theme brings to attention the alarming effects of unexpected calamities, be they local (earthquakes, floods, wars, extreme weather) or global, like the coronavirus disease 2019 (COVID-19) pandemic and climate change. In addition to tremendous immediate losses, these catastrophes have an enduring impact on humans, the environment, and the economy. People with long-term illnesses such as CKD are particularly vulnerable to these unexpected calamities. These events disrupt health-care delivery, including access to dialysis, laboratory work, visits to nephrologists, and distribution of medications and immunosuppressive agents. Patients on dialysis, especially in-center hemodialysis, are the worst affected as they are left at the mercy of circumstances while trying to ensure continuity of care. There are many instances where unseasonal and extreme weather variations have prevented patients from reaching their dialysis units.[2] Issues such as the interruptions in supply chain leading to shortage of dialysis consumables, extreme temperatures, scarcity of food, and shortage of clean water make the situation more daunting. Low-resource countries are disproportionately more affected due to their limited resilience capacity. Some of these calamities are recurrent, and failure of the policymakers to factor them into delivery of care introduces a man-made element to these natural calamities. During the COVID-19 pandemic, massive disruptions in dialysis delivery led to large number of avoidable deaths.[3] Essential outpatient services for nephrology care also took a hit.[4] Transplantation services were discontinued in many parts of the world, leading to untold hardships for economically vulnerable patients who had to spend their savings on dialysis. Climate change and subsequent environmental catastrophes also increase the incidence of kidney diseases.[5] The collapse of the health-care infrastructure, disruption of immunization drives, inadequate sanitation, and large-scale relocation of people during these events tend to trigger outbreaks of communicable diseases such as cholera, measles, malaria, and the novel coronavirus, and it is expected that cases of acute kidney injury rise in conjunction with these calamities.[6] The health and well-being of patients on hemodialysis, peritoneal dialysis, or kidney transplants have been adversely impacted due to the ongoing armed conflict in Ukraine.[7] In already economically challenged countries like Lebanon and Sri Lanka, the COVID-19 pandemic and events like the explosion in Beirut have exacerbated their crisis and compounded the hardships for renal patients.[8] India being a geographically diverse country, some states are especially vulnerable to catastrophes like landslides and floods. The health impacts of flooding are well recognized, and the National Centre for Disease Control has issued public health guidelines aiming to reduce adverse health effects after floods.[9] The situation related to disrupted healthcare will be no different in Turkiye, Syria, and Lebanon following the recent devastating earthquake. There is an urgent requirement for more resilient and adaptable health-care systems for kidney patients in distressed situations. We need to develop unique indigenous solutions targeting local issues. An example of such a solution is setting up a unified dashboard for allocating and scheduling dialysis for COVID-19 patients in Mumbai, which successfully averted mortality from delayed or denied dialysis.[10] It is imperative that health systems, particularly in lower- and middle-income countries, build up their human resources, create sustainable policies, and establish strategic partnerships to be adequately prepared to handle potential threats to the renal community. This is particularly important and relevant in India, where little thought and attention has been given to this issue. Figure 1 shows some important challenges and solutions for patients with kidney diseases during disastrous events.
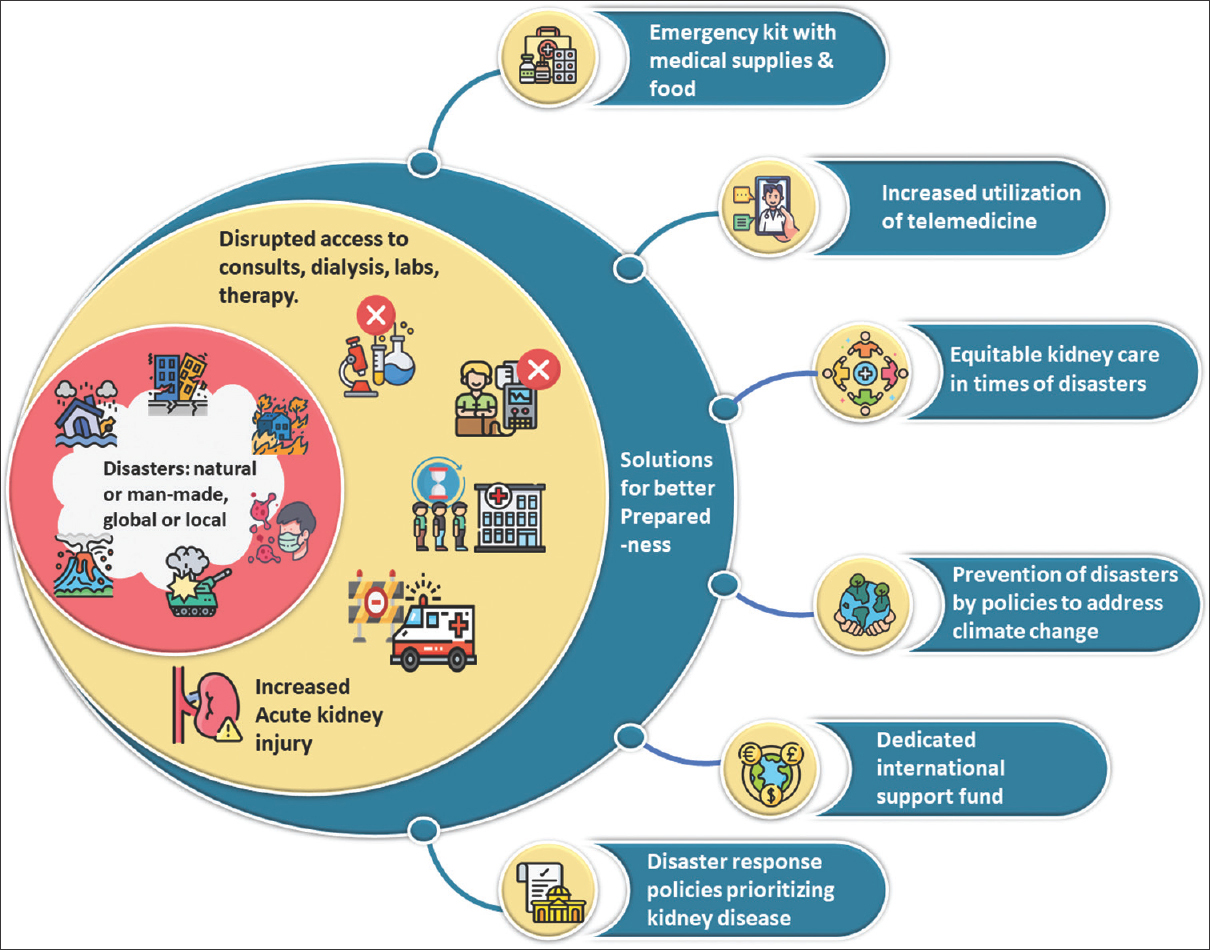
- Important challenges and solutions for patients with kidney diseases during disastrous events
References
- A-single number for advocacy and communication worldwide more than 850 million individuals have kidney diseases. Nephrol Dial Transplant. 2019;34:1803-5.
- [Google Scholar]
- Natural disasters in the Americas, dialysis patients, and implications for emergency planning: A-systematic review. Prev Chronic Dis. 2020;17:E42. doi:10.5888/pcd17.190430
- [Google Scholar]
- Safeguarding dialysis services during the COVID-19 pandemic. Nat Rev Nephrol. 2021;17:569.
- [Google Scholar]
- The adverse effect of COVID pandemic on the care of patients with kidney diseases in India. Kidney Int Rep. 2020;5:1545-50.
- [Google Scholar]
- Climate change and kidney disease threats and opportunities. Kidney Int. 2017;92:526-30.
- [Google Scholar]
- The impact of war on the health system of the Tigray region in Ethiopia: An assessment. BMJ Glob Health. 2021;6:e007328. doi:10.1136/bmjgh-2021-007328
- [Google Scholar]
- Lifesaving care for patients with kidney failure during the War in Ukraine 2022. Clin J Am Soc Nephrol. 2022;17:1079-81.
- [Google Scholar]
- Preparing for the unexpected, supporting the vulnerable—A perspective from Lebanon and Sri Lanka. Kidney Int Rep 2023 doi:https://doi.org/10.1016/j.ekir.2023.01.022
- [Google Scholar]
- Floods, landslides and COVID-19 in the Uttarakhand State, India: Impact of Ongoing Crises on Public Health. Disaster Med Public Health Prep. 2022;16:2279-82.
- [Google Scholar]
- A-Unified citywide dashboard for allocation and scheduling dialysis for COVID-19-patients on maintenance hemodialysis. Indian J Nephrol. 2022;32:197-205.
- [Google Scholar]






