Translate this page into:
Transition of Kidney Care at 18: Challenges and Practical Solutions for India
-
Received: ,
Accepted: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Health-care transition (HCT) from pediatric-centered to adult-oriented health-care setting is more than a simple transfer of care. It is a carefully planned movement specially tailored for the needs of adolescents and young adults (AYAs). Similar to other chronic diseases, the need for HCT for AYAs with kidney disease has been well established by the International Society of Nephrology (ISN) and the International Pediatric Nephrology Association (IPNA) consensus statements since 2011. However, successful HCT in India and other low- and middle-income countries (LMICs) has been limited. Undertaking the HCT program in India requires involvement of many stakeholders, that is, AYAs, parents/caregivers, health-care providers, and the health-care system. In this article, we discuss the need for HCT, the challenges faced during the transition, and the recommended models for HCT in kidney care. We focus on the unique challenges faced in India and conclude with practical suggestions to implement HCT in our setting.
Keywords
Adolescents and young adults
chronic kidney disease
health-care transition
kidney transplantation
transition clinic
Introduction
Health-care transition (HCT) has been defined as the “purposeful, planned movement of adolescents and young adults (AYAs)” with chronic physical and medical conditions from child-centered to adult-oriented health-care systems.[1] Therefore, the scope of HCT extends beyond a simple transfer and encompasses a long-term coordinated passage that prepares the AYAs to accept responsibility for their disease and learn self-management in the adult unit.[2]
Who Needs Transition of Care?
In terms of neurodevelopment, the AYA years encompass a broad age span (14–24 years), during which brain maturation and development continue.[3] This period marks a dual shift for AYAs with a chronic illness: one from childhood to maturity with ongoing physical, psychological, emotional, and sexual changes and another in health care, from pediatric to adult treatment. During this era, parental/caregiver power over medical decision-making is transferred to patient autonomy, granting AYAs the responsibility for their own health care.
Is There a Need for a Transition of Kidney Care?
As in other chronic diseases, the importance of HCT in AYAs with kidney disease has become apparent as a growing number graduate from pediatric nephrology units to adult nephrology services. More easily accessible care by pediatric nephrologists results in improved survival rates of 85%–90% among AYAs with chronic kidney disease (CKD)/kidney failure, which is better than survival rates in adults with the same condition.[4] It is widely recognized that this age group has a high risk of nonadherence, leading to increased rejections and graft loss in renal transplant recipients.[56] From an adolescent perspective, HCT assumes great importance. Adolescents must leave behind the secure and familiar world of pediatric nephrology units where parental supervision is the rule, their immaturity is understood, and decision-making is not expected. When AYAs enter the adult nephrology units, they find busier clinics, less time for interaction with the medical team, and are expected to take up full responsibility for their health and well-being. Transition care supports this process by providing a structured approach to negotiating these changes and by empowering AYAs to cross the bridge effectively.
Do HCT Clinics Improve the Clinical Outcomes?
Studies have compared the outcomes of AYAs cared for in specialized transition clinics versus historical outcomes before the establishment of HCTs. The results have been compelling. In Canada, Prestidge et al.[7] evaluated the outcomes of 33 posttransplant patients who were only transferred and 12 who were “formally transitioned”. The incidence of death/allograft loss was 24% within 2 years post-transfer in those who were just “transferred,” compared to no death/allograft loss in the transitioned cohort. They also found that providing transition clinics was economically feasible. Similarly, a quality improvement report by Harden et al.[8] from the UK compared the outcomes of transplant recipients observed at two points in time. In the early period where the transfer was only by a referral letter, 67% experienced graft failure after transfer and 33% had late acute rejection. In the later period where patients were seen in a joint transition clinic and were followed up in a young adult clinic after the transfer, there were no graft failures and no late acute rejections at a median of 26 months of follow-up, and the transplant survival of the formally transitioned group was favorable compared to historical controls (log-rank test, P = 0.015). These results stood true in both studies after adjusting for possible risk factors including differences in medical care at different time points. However, these studies were nonrandomized and only measured short-term outcomes.
Patient-centered outcomes are important in assessing the effectiveness of a transition program. In a survey of AYAs with kidney disease who had transitioned from pediatric care, 88% felt that having a transition appointment and meeting the adult care providers in the pediatric setting was valuable.[9] McQuillan et al.[10] compared the outcomes of kidney transplant recipients before and after the establishment of a transition clinic and found that attendance at the clinic had significantly improved adherence, in addition to renal function. A survey by Tong et al.[11] on a newly established young adult renal clinic showed that the clinic also encouraged self-management, optimism, emotional resilience, satisfaction, and engagement with health-care services. Thus, the literature supports the need for a planned HCT of AYAs in terms of clinical as well as patient-centered outcomes.
To address this need, a consensus viewpoint on ideal clinical management of the transition of AYAs with kidney disease was developed by an expert panel and was endorsed by councils of both the International Society of Nephrology (ISN) and the International Pediatric Nephrology Association (IPNA) in 2011.[12] Despite the publication of HCT guidelines, its global application in clinical practice has been inadequate.[131415] A systematic review of transition practices in adolescent kidney transplant recipients showed a lack of uniformity in the transition models followed by 12 different centers.[16]
Challenges of Applying HCT Models to Low-Resource Settings
In low- and medium-income countries (LMICs), HCT is challenging because there has been a rapid increase in the number of AYAs transitioning to adult renal services. In LMICs, the provision of HCT is relatively recent with only a few published transition models, mostly focused on AYAs living with human immunodeficiency virus (HIV).[17] A recent review on adolescent HCT in LMICs reflected a lack of formal policy for HCT for diseases other than HIV.[18] A survey of transition of kidney transplant recipients in European countries found that adherence to 2011 ISN–IPNA guidelines correlated directly with a gross national income, putting LMIC patients at a disadvantage.[13] This emphasizes the need for HCT resources and perhaps explains their limited application in low-resource settings. There has been only one HCT model described for kidney diseases from South Africa, which will be described in detail below.[19]
Does India have HCT Clinics for Kidney Diseases?
India has one of the largest adolescent populations in the world.[20] Although there are a few studies on HCT in HIV patients and a small pilot study on children with chronic diseases, there are none on the transition of kidney care.[2122] This is probably because HCT occurs informally with widely varying transition practices depending on the type of medical center, the volume of clinical load, and the level of interdepartmental coordination.
HCT Process: Stakeholder Roles and Challenges Encountered
A successful HCT requires participation and coordination among all stakeholders: AYA, family, pediatric, adult health professionals, and the health-care system. Removing barriers to transition requires understanding and addressing challenges involving each stakeholder. Figure 1 shows the challenges encountered by each stakeholder during the process of transition.

- Challenges to a successful transition. Each circle represents the challenge that each stakeholder faces/contributes to the process of transition. AYA = adolescent and young adult
Adolescents and young adults
AYA is at the heart of the HCT process. Any change in medical caregivers is difficult for adolescents, and AYAs with CKD face additional challenges. These include cognitive deficits, learning disabilities, memory deficits, low self-esteem, poor self-body image due to short stature, high-risk behavior, anxiety, and depression, with the prevalence of depression reportedly as high as 10%–35%.[232425] They not only have a lower intellectual and academic functioning compared to healthy peers, but also have poor social functioning which interferes with their coping skills.[2627] Nonadherence is another primary concern, especially involving transplant recipients at the time of transfer and generally in all patients less than 25 years of age.[528] Nonadherence increases the risk of rejection and graft loss,[5629] and the period of transition is associated with a high risk of graft failure.[30] Hesitance to transfer is another challenge: studies on AYAs with kidney diseases have reported this emotional attachment to the pediatric nephrology unit and anxiety about transferring.[3132]
Family
The family’s role in HCT cannot be overemphasized. The interplay of multiple social and economic factors in the family, including family functioning, family size, parental education and awareness, and financial constraints, all have direct relevance to the success of HCT. A resistance to transition is seen, not only among the AYAs but also among parents. A recent study showed that mothers were reluctant to leave the pediatric nephrology unit and they found the transition more challenging than the AYAs.[31] This is because, in addition to leaving the comfort of familiarity of the pediatric unit, the mothers have an enormous task of relinquishing the role of a primary caregiver and transferring the responsibility of disease management to the young adults themselves.
Pediatric nephrologist
It remains the pediatrician’s responsibility as the primary health provider to introduce this concept to the patient and family and follow through with the actual transition process. Interrupted follow-up, difficulties in interdepartmental coordination, lack of supporting professionals, and different approaches to treatment in the pediatric and adult settings contribute to challenges faced by a pediatrician.[33]
Adult nephrologist
Although pediatric nephrologists have been the focus of transition recommendations, the role of adult nephrologists as “receiving providers” has become more evident in recent years.[1234] Pediatric kidney diseases are different from adult-onset conditions. Although glomerular diseases (chronic glomerulonephritis, steroid-resistant nephrotic syndrome) are the most common causes of adolescent-onset CKD, congenital abnormalities of the kidney and urinary tract (CAKUT) and hereditary nephropathies are the most common causes of childhood-onset CKD. Adult nephrologists may be relatively unfamiliar with handling these conditions and may have limited experience in managing issues such as growth, sexual maturation, and psychological and educational needs. Interactions with pediatricians and overlapping shared care over years were perceived to be vital for a successful transition by German nephrologists.[35]
Health-care system
HCT needs time, money, and a workforce. Rigid health-care systems contribute in many ways to these barriers. A nationwide study among nephrologists in Germany pointed out that logistical, financial, and institutional constraints were the main barriers to transition.[35] Efforts should be made to make room for changes in the existing health-care framework to incorporate HCT.
Unique Challenges to HCT in India
The challenges in establishing HCT in India are inherently complex. There are very few hospitals with existing pediatric and adult renal service units that can cross-refer patients. At most centers, the adult nephrology unit gets references for pediatric CKD directly from outside centers, limiting the physical interaction between caregivers. Although there is a handover of relevant medical knowledge, the sheer volume of clinical work could deter a one-to-one interaction between the pediatrician, adult nephrologist, social worker, support professional, AYA, and family. The physical distance between the pediatric and adult nephrology clinics could also contribute to the gap. Some centers may not have computerized medical records entirely, restricting access to old records and information. Another barrier is the loss of follow-up of children and their families, which is a unique problem observed in Indian pediatric transplants.[36] Also, there is no accepted uniform age for transfer to the adult unit, with some centers transferring as early as 12 years of age. Despite all these barriers, the number of patients being transitioned in each hospital is small, and a joint effort by both units to focus on these patients and ensure a smooth transition, we think, will not overwhelm the hospital’s clinical capacity.
Transition models from HICs advocate a gradual, but complete transfer of responsibility to the AYAs. It is encouraged for parents to “step back.” Due to cultural and traditional differences, in India, parents play a major part in the continued management of their children’s illness, even beyond 18 years of age. This said, AYAs, who are usually better educated than their parents, do start to take a primary interest in the process and must be encouraged in this direction. In our country, it is impractical and counterproductive to completely exclude parents. Hence, a working transition model should be parent inclusive and focus on “transitioning parents” in addition to AYAs. Health insurance and its discontinuity pose major problems during the transition and contribute to the loss of follow-up of AYAs in HICs. This might not be particularly applicable to India, at least as of present. Teenage pregnancy, sexually transmitted diseases, drug abuse, and teenage violence, though present, may not be as daunting a problem to us. The real challenges are economic and social constraints, lack of awareness, and illiteracy.
Models of HCT in Existence/Recommended
The ISN–IPNA 2011 consensus statement has laid down five key components of the transition process: the individualized transition process that leads up to the transfer, transition clinics, the actual transfer to adult care, and continuity of care in the adult unit at “young adult clinics.” The transition process begins with introducing the concept of transition in early adolescence (12–14 years). Transition clinics should be attended by pediatric nephrologists, adult nephrologists with special training in pediatric CKD 4–5, and pediatric and adult specialty nurses. Leading physicians with a particular interest in the transition process are referred to as “transition champions,” while those who manage the transition’s steps are referred to as “transition coordinators.” The statement recommends the use of “TR(x)ANSITION” scale to assess readiness for transition and monitor its progress.[37] Once transferred to the adult setting, AYAs are cared for in “young adult clinics,” which consist of an adult nephrologist, a nurse, and support staff (youth workers/social workers). The consensus statement emphasizes multidisciplinary engagement, interdepartmental collaboration, group sessions, and peer support. The recommendations outline the ideal transitional care. However, the authors note that many statements lack documented evidence, and that it may be difficult to attain the recommended standards of care, particularly in settings with limited resources. Nonetheless, the statement might provide a foundation for developing locally relevant proposals.
A pilot study from South Africa deserves a special mention as it demonstrates the feasibility of establishing an economical adolescent service in a resource-limited setting. The adolescent nephrology setting was meant to be a bridge between pediatric and adult units and was co-designed based on the needs of AYAs with kidney disease assessed by a questionnaire. Based on the unmet needs expressed by the AYAs, pilot workshops were conducted for CKD patients and transplant recipients less than 25 years of age. The adolescent clinic which was run twice monthly had two parts. The first was a friendly, open platform for AYAs and parents and was aided by a social worker and a patient mentor (CKD patients less than 30 years). Practical life skills and challenges like sexual health, drug abuse, and adherence were openly discussed. The second part was the clinic which was run by an adult nephrologist, a senior renal fellow, a medical registrar, and an attending pediatric nephrologist from a children’s hospital.[19]
A Practical Approach to HCT in India: Implementing HCT in India
The necessity for a formal HCT in India is obvious, despite the lack of comprehensive research on the topic, with the exception of a small pilot study by Menon et al.[22] on AYAs with chronic diseases, which reaffirmed the need for a transition clinic. Before anything else, it would be beneficial to undertake a nationwide survey to examine the current practices of transition and identify the gaps and challenges that are specific to our country.
-
Transition clinic
We suggest setting up a weekly or bimonthly combined outpatient “transition clinic” for AYAs aged 16–18, leading up to the actual transfer to the adult unit at 18 years of age. This would be run by a dedicated team of pediatric and adult nephrologists, dieticians, transplant coordinators, dialysis nurses/technicians, social workers, and visiting specialists like urologists and transplant surgeons. This clinic would care for AYAs transferred from pediatric care and those who present directly to the adult nephrology units. The latter would particularly be relevant to our country as most of the referrals are of this form. Regardless of the transition clinic, there should be continued interaction of both units at all times. Figure 2 gives the role of each stakeholder in the transition process, and Figure 3 describes the timeline of the transition.
-
Specific role of health providers
2.1. Pediatric team
The pediatric team should be responsible for preparing and counseling the AYA and family for HCT, starting from early adolescence. Even before the transition clinics, they should ensure informal visits of AYAs and families to the adult nephrology outpatient clinic and dialysis center. Pediatricians should prepare and maintain a transition checklist that is updated by both teams at each transition clinic [Table 1] and a transition summary at the time of transfer. We suggest that a renewable and portable medical record like the “nephrology medical passport” that can be carried in a wallet can be made available to the patient, with diagnosis, management, and contact details in it, as it can be helpful when access to electronic records is not available.[37] After transfer, they should collect feedback from AYAs and continue to offer consults as required.
2.2. Adult team
We suggest that adult physicians in the transition team should take a special interest in HCT. One among them can receive training in managing AYAs with childhood-onset kidney diseases and function as the “lead transition physician” who coordinates and oversees the transition. We suggest there should be compulsory rotations of adult nephrology trainees in pediatric units and vice versa.
2.3. Role of supporting professionals
Social workers can facilitate discussion on financial sources and insurance, arrange school/peer support, provide occupational counseling, and look into real-life problems resulting in loss of follow-up or nonadherence. Addressing psychosocial and financial issues in the family, jointly as a team, would ease the process, as pediatricians are familiar with the long-standing issues in each family.
2.4. Specific nephrology issues
At the clinic, specific issues can be dealt with jointly: vascular access and its complications; the choice of versus; evaluation and follow-up of donors; decisions of living versus deceased kidney donors; assessment of the need and interpretation of genetic analysis; assessment of the risk of posttransplant recurrence; fine-tuning of drug dosing; and management of extrarenal complications, side effects and toxicity of immunosuppressants, drug interactions, pretransplant urological issues, and sexual and reproductive health issues.
2.5. AYA and family
AYA and parents should be aware, counseled, and ready for the transition. The “TR(x)ANSITION” scale is a 32-point questionnaire of 10 domains (Type of chronic health condition, Rx/Medications, Adherence, Nutrition, Self-management skills, Issues of reproduction, Trade/School, Insurance, Ongoing Support, New health-care provider)[3839] that is scored based on AYA’s level of knowledge. The total scores can be used to monitor the transition and the sub-scores to identify and address barriers. “Peer mentoring” has been shown to improve the quality of life in CKD patients.[40] Few AYA volunteers with CKD/transplant recipients can be invited to lead in this effort. For an AYA, social media, the internet, and smartphone are essential parts of everyday life. An interesting study conducted to assess “mobile health readiness” found that CKD patients on dialysis were ready and capable in mobile health.[41] The benefit of using computer-based education on immunosuppressant adherence has been demonstrated among lung transplant recipients.[42] Such a “mobile health” initiative should be utilized through apps, websites, and emails to promote adherence, further knowledge base, and encourage AYAs to learn self-management skills.
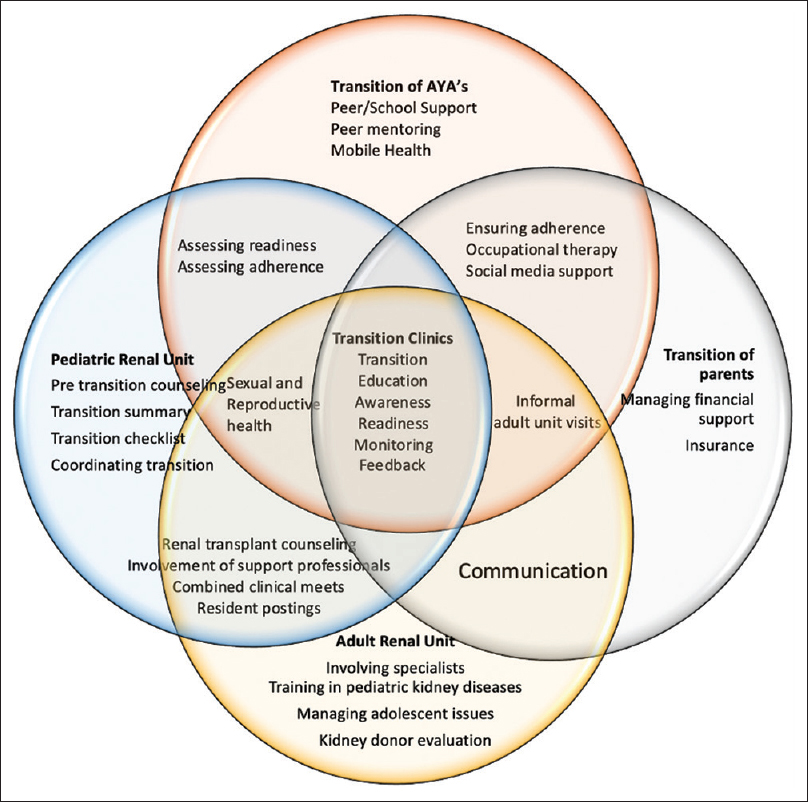
- Transition model. Each circle represents the role and responsibility of each stakeholder in the process of transition. AYA = adolescent and young adult

- Transition model. The figure describes the timeline of transition from conception to completion with the role of each participant at different times. AYA = adolescent and young adult
| Name: | ||
| Gender: | ||
| Age: | ||
| School: | ||
| Medical issues including primary diagnosis: | ||
| Current pediatric nephrologist: | ||
| Hospital: | ||
| Current medications: | ||
| Age at diagnosis of kidney disease: | ||
| Age and year of initiation of transition: | ||
| To be filled by the “transition team” | ||
| Readiness for transition | Yes | No |
| Is the AYA counseled for transition? | ||
| Is the AYA willing for transition? | ||
| Are parents counseled for transition? | ||
| Are parents willing for transition? | ||
| Have informal visits of AYA/parents to the adult unit taken place? | ||
| Anticipated barriers to transition: | ||
| Interrupted follow-up------------------------------------------------------------------------ | ||
| Nonadherence-------------------------------------------------------------------------------- | ||
| Lack of interest------------------------------------------------------------------------------- | ||
| Financial-------------------------------------------------------------------------------------- | ||
| Social----------------------------------------------------------------------------------------- | ||
| Others----------------------------------------------------------------------------------------- | ||
| Transition planning and monitoring | Yes | No |
| Has a transition plan been made? | ||
| If yes, details: ----------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------- | ||
| Is the family part of any support group? | ||
| Has the TR(x)ANSITION scale been used? | ||
| If yes, scores:------------------------------------------------------------- | ||
| Has a “transition summary” been provided? | ||
| Tick the participants involved in the transition care process: | ||
| AYA, parents/family/caregivers, pediatric nephrologist | ||
| Adult nephrologist, social worker, transplant coordinator | ||
| Peers, specialists (urologist, transplant surgeon, pediatric surgeon, dialysis nurse/technician) | ||
| Transfer of kidney care | ||
| Age and year of transition completion | ||
| Adult nephrologist: | ||
| Hospital: | ||
AYA=adolescent and young adult, TR(x)ANSITION - Type of chronic health condition, Rx/Medications, Adherence, Nutrition, Self-management skills, Issues of reproduction, Trade/School, Insurance, Ongoing Support, New health-care provider
Conclusion
HCT of AYAs with kidney diseases is the need of the hour. Good transition practices will improve patient outcomes and ease care for adult nephrologists. The way forward in the Indian clinical setup would involve identifying barriers to transition, formally educating trainees about transition, and bridging the different cultures of care: pediatric, adolescent, and adult by improving interdepartmental coordination, multidisciplinary involvement, formation of transition clinics, and, most importantly, instilling a patient-centric approach in everyday clinical practice.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Transition from child-centered to adult health-care systems for adolescents with chronic conditions. A position paper of the society for adolescent medicine. J Adolesc Health. 1993;14:570-6.
- [Google Scholar]
- Transitional care: Transferring adolescents from paediatric to adult renal units. Br J Ren Med. 1996;1:24-6.
- [Google Scholar]
- Trends in treatment and outcomes of survival of adolescents initiating end-stage renal disease care in the United States of America. Pediatric Nephrol. 2006;21:1020-6.
- [Google Scholar]
- Adherence to the immunosuppressive regimen in pediatric kidney transplant recipients: A systematic review. Pediatr Transplant. 2010;14:603-13.
- [Google Scholar]
- Heightened graft failure risk during emerging adulthood and transition to adult care. Pediatric Nephrology. 2015;30:567-76.
- [Google Scholar]
- Utility and cost of a renal transplant transition clinic. Pediatr Nephrol. 2012;27:295-302.
- [Google Scholar]
- Bridging the gap: An integrated paediatric to adult clinical service for young adults with kidney failure. BMJ. 2012;344:e3718. doi:10.1136/bmj.e3718
- [Google Scholar]
- Assessing success in transitioning of young adults from pediatric to adult kidney practice. BMCNephrol. 2020;21:8. doi:10.1186/s12882-019-1665-7
- [Google Scholar]
- Benefits of a transfer clinic in adolescent and young adult kidney transplant patients. Can J Kidney Health Dis. 2015;2:45. doi:10.1186/s40697-015-0081-6
- [Google Scholar]
- Patient perspectives of a young adult renal clinic: A mixed-methods evaluation. Nephrology. 2015;20:352-9.
- [Google Scholar]
- Transition from pediatric to adult renal services: A consensus statement by the International Society of Nephrology (ISN) and the International Pediatric Nephrology Association (IPNA) Kidney Int. 2011;80:704-7.
- [Google Scholar]
- Survey on management of transition and transfer from pediatric- to adult-based care in pediatric kidney transplant recipients in Europe. Transplant Direct. 2018;4:e361. doi:10.1097/TXD.0000000000000798
- [Google Scholar]
- Survey on health care transition services in pediatric nephrology. Clin Exp Nephrol. 2018;22:206-7.
- [Google Scholar]
- Transition of adolescent and young adult patients with childhood-onset chronic kidney disease from pediatric to adult renal services: A nationwide survey in Japan. Clin Exp Nephrol. 2016;20:918-25.
- [Google Scholar]
- Transitional care models in adolescent kidney transplant recipients-A systematic review. Nephrol Dial Transplant 2022:gfac175. doi:10.1093/ndt/gfac175
- [Google Scholar]
- Barriers and facilitators to the successful transition of adolescents living with HIV from pediatric to adult care in low and middle-income countries: A systematic review and policy analysis. AIDS Behav. 2019;23:2498-513.
- [Google Scholar]
- Paediatric to adult healthcare transition in resource-limited settings: A narrative review. BMJ Paediatr Open. 2021;5:e001059. doi:10.1136/bmjpo-2021-001059
- [Google Scholar]
- Adolescent nephrology: An emerging frontier for kidney care in sub-Saharan Africa. Nephrology. 2017;22:933-9.
- [Google Scholar]
- Healthcare needs and programmatic gaps in transition from pediatric to adult care of vertically transmitted HIV infected adolescents in India. PLoS One. 2019;14:e0224490. doi:10.1371/journal.pone. 0224490
- [Google Scholar]
- Need and feasibility of a transition clinic for adolescents with chronic illness: A qualitative study. Indian J Pediatr. 2020;87:421-6.
- [Google Scholar]
- Neurocognitive functioning of children and adolescents with mild-to-moderate chronic kidney disease. Clin J Am Soc Nephrol. 2011;6:1824-30.
- [Google Scholar]
- High depression rates among pediatric renal replacement therapy patients: A cross-sectional study. Pediatric Transplant. 2019;23:e13591. doi:10.1111/petr. 13591
- [Google Scholar]
- Depressive symptomatology in children and adolescents with chronic renal insufficiency undergoing chronic dialysis. Int J Nephrol. 2011;2011 doi:10.4061/2011/798692
- [Google Scholar]
- Health-related quality of life of children with mild to moderate chronic kidney disease. Pediatrics. 2010;125:e349-57.
- [Google Scholar]
- Brief report: Intellectual and academic functioning in pediatric chronic kidney disease. J Pediatr Psychol. 2007;32:1011-7.
- [Google Scholar]
- Non-compliance and transfer from paediatric to adult transplant unit. Pediatr Nephrol. 2000;14:469-72.
- [Google Scholar]
- Association between age and graft failure rates in young kidney transplant recipients. Transplantation. 2011;92:1237-43.
- [Google Scholar]
- Graft failure and adaptation period to adult healthcare centers in pediatric renal transplant patients. Transplantation. 2011;91:1380-5.
- [Google Scholar]
- Transition from a renal paediatric clinic to an adult clinic: Perspectives of adolescents and young adults, parents and health professionals. J Child Health Care 2021:136749352110284. doi:10.1177/13674935211028410
- [Google Scholar]
- Transitioning adolescents to adult nephrology care: A systematic review of the experiences of adolescents, parents, and health professionals. Pediatr Nephrol. 2020;35:555-67.
- [Google Scholar]
- An interdisciplinary approach to optimize the care of transitioning adolescents and young adults with CKD. Blood Purif. 2021;50:684-95.
- [Google Scholar]
- Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011;128:182-200.
- [Google Scholar]
- Barriers to the successful health care transition of patients with kidney disease: A mixed-methods study on the perspectives of adult nephrologists. Children. 2022;9:803. doi:10.3390/children9060803
- [Google Scholar]
- Low renal transplantation rates in children with end-stage kidney disease: A study of barriers in a low-resource setting. Pediatr Transplant. 2021;25:e13867. doi:10.1111/petr. 13867
- [Google Scholar]
- Toward evidence-based health care transition: The health care transition research consortium. Int J Child Adolesc Health. 2011;3:479-86.
- [Google Scholar]
- The health care transition research consortium health care transition model: A framework for research and practice. J Pediatr Rehabil Med. 2014;7:3-15.
- [Google Scholar]
- https://www.med.unc.edu/transition/transition-tools/starx-questionnaire/
- Effect of peer mentoring on quality of life among CKD patients: Randomized controlled trial. Kidney Dis. 2021;7:323-34.
- [Google Scholar]
- The mobile health readiness of people receiving in-center hemodialysis and home dialysis. Clin J Am Soc Nephrol. 2021;16:98-106.
- [Google Scholar]
- Conventional vs. tablet computer-based patient education following lung transplantation--A randomized controlled trial. PLoS One. 2014;9:e90828. doi:10.1371/journal.pone. 0090828
- [Google Scholar]







