Translate this page into:
Lipofuscin Deposition in the Kidney: Damaging or Deceiving?
Corresponding author: Vinay Rathore, Department of Nephrology, All India Institute of Medical Sciences (AIIMS), Tatibandh, Raipur, India. E-mail: vinayrathoremd@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Saha AK, Rathore V, Sharma A, Pathak NM. Lipofuscin Deposition in the Kidney: Damaging or Deceiving? Indian J Nephrol. doi: 10.25259/IJN_101_2025
Abstract
Lipofuscin is an intracellular deposit comprising proteins and lipids that accumulate with aging. Lipofuscin deposition in native human kidneys is rarely reported. A 51-year-old hypertensive female suffering from chronic kidney disease presented with unexplained GFR deterioration. Kidney biopsy revealed extensive golden-brown lipofuscin pigment deposition in renal tubules.
Keywords
Chronic kidney disease
Intracellular deposits
Lipofuscin
Native kidneys
Introduction
Lipofuscins are oxidized lipid and protein complexes that accumulate during cellular senescence and tissue aging. They are considered non-pathogenic and an oxidative tissue damage and aging marker.1 Lipofuscin deposition in native kidneys is rarely reported in the literature. We present a 51-year-old female with chronic kidney disease (CKD) whose kidney biopsy revealed extensive golden-brown lipofuscin pigment deposition in tubular epithelial cells.
Case Report
A 51-year-old female with hypertension for five years, well-controlled by Telmisartan (40 mg) and CKD for the last three years, presented with a sudden serum creatinine increase from 1.8 mg/dL (eGFR=34 mL/min/1.73 m2) to 5.4 mg/dL (eGFR=9 mL/min/1.73 m2) over 15 days.
She denied using over-the-counter drugs, herbal products, and analgesics or having fever, dysuria, diarrhea, and vomiting during this period. Physical examination revealed an average build with a 21 kg/m2 BMI and 128/82 mm Hg BP. The physical examination was unremarkable.
Investigations revealed 10.2 g/dL hemoglobin, 7800 cells/mm3 total leukocyte count, and 2.4 L/µL platelet count. Serum electrolytes revealed 137 meq/L sodium, 4.2 meq/L potassium, and liver function tests were within normal limits. The serum albumin was 3.8 gm/dL. Urine microscopic examination did not reveal any active urinary sediments. She revealed an 800 mg/day 24-hour urinary protein excretion. Anti-nuclear antibody was negative. C3 and C4 were normal. Serum protein electrophoresis and immunofixation did not show any monoclonal proteins.
Renal biopsy showed golden-brown pigment material accumulation in tubular epithelial cytoplasm [Figure 1a], which stained negative for hemosiderin by pearls stain [Figure 1b]. Glomeruli were unremarkable, and direct fmmunofluorescence studies were negative.
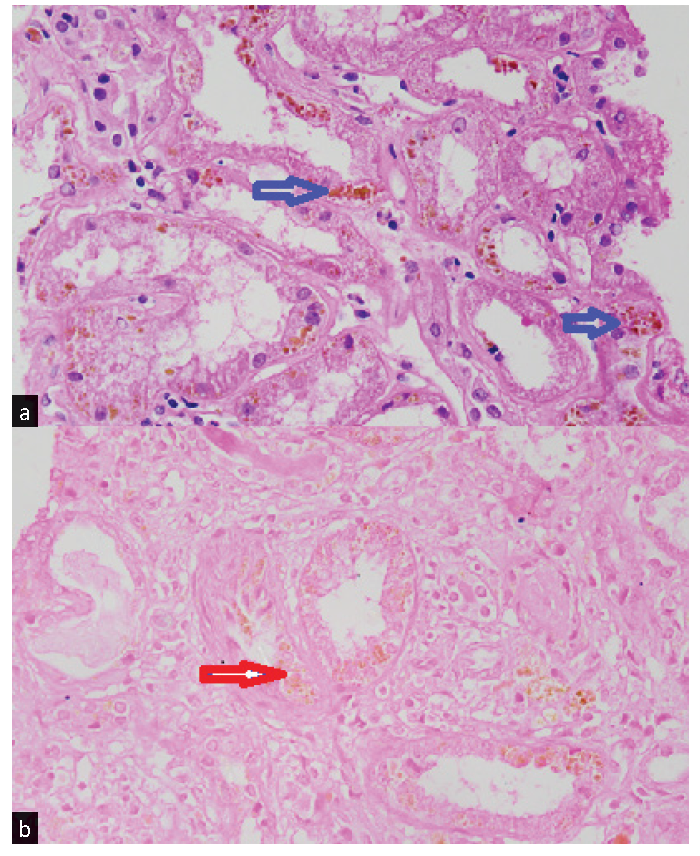
- (a) Histopathology of the renal biopsy specimen showing accumulation of golden-brown pigment material in the cytoplasm of many tubular epithelial cells (blue arrows). (b): Negative Pearls staining for hemosiderin of the golden-brown pigment (red arrow).
An inductively coupled plasma mass spectrometry (ICP-MS) analysis of serum for heavy metals revealed normal arsenic, cadmium, mercury, lead, and aluminum levels. The patient was managed with intravenous hydration, and her creatinine improved to 2.1 mg/dL.
She was discharged with Vitamin E (600 IU twice a day) supplementation. Serum creatinine after 1 month was reduced to 1.9 mg/dL. The 18-month follow-up showed 2.1mg/dL serum creatinine and 785 mg/day proteinuria.
Discussion
Lipofuscin pigment comprises proteins and lipids from cell membrane breakdown, which may accumulate due to slowing lysosomal function or because of altered lipid peroxidation.2 These deposits have also been described in solid organ transplants like kidney allografts and, more commonly, in heart transplants.3 Lipofuscin deposition in native human kidneys has been very rarely reported in literature.
Golden-brown pigment in the kidney tissue can be due to lipofuscin, hemosiderin, melanin, or formalin pigment artifact deposition. Out of these, hemosiderin and formalin pigment (Formalin-Heme complex) artefact stain positive with Pearls technique4 due to the presence of iron and melanin and do not stain with PAS.5 Considering the deposit was PAS positive and Pearls negative, it was diagnosed as lipofuscin.
Lipofuscin deposition is considered a manifestation of cellular aging. The deposition can increase under cellular oxidative stress. Various pathogenic effects have been described in the literature, which include decreased lysosomal degradation efficiency of newly autophagocytosed material, increased biomolecule oxidation within lipofuscin, and toxic product and reactive oxygen species formation causing tissue damage.6 Despite the described theoretical mechanism, the pigment is largely considered non-pathogenic except in a few conditions like Hermansky-Pudlak syndrome, lysosomal storage disorders, and neurodegenerative diseases.2
There is no definite evidence establishing lipofuscin’s role in kidney injury. However, CKD and acute kidney injury causing oxidative stress can increase deposition and decrease lipofuscin removal from the kidney. In the index case, lipofuscin deposition in the kidney was probably secondary to oxidative stress due to kidney damage. The acute rise in the index case was possibly due to acute tubular injury, the cause of which could not be ascertained despite extensive workup. The renal functions improved with intravenous hydration and returned to the baseline.
In conclusion, evidence to prove lipofuscin’s role in causing kidney injury is still lacking despite having several theoretical mechanisms. The pigment may be deposited in the kidney tissue of older individuals and those with CKD. Clinicians should be aware of the possibility of encountering such findings on biopsy specimens and should be careful before assigning them as pathogenic due to the dearth of evidence for the same.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
References
- Lipofuscin granule accumulation requires autophagy activation. Mol Cells. 2023;46:486-95.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A patient with unexpected golden brown tubular staining. Kidney360. 2024;5:631-2.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A case report on lipofuscin deposition in a graft biopsy two years after kidney transplantation: An insignificant bystander or a pathogenic benefactor? BMC Nephrology. 2019;20:376.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Team MH. Perls’ / Prussian blue staining for iron stores protocol. Available from: https://myhematology.com/red-blood-cells/perls-prussian-blue-staining/2023 [last accessed on 5 Mar 2025].
- Staining properties of melanin and lipofuscin pigments. Am J Clin Pathol. 1986;86:556-7.
- [CrossRef] [PubMed] [Google Scholar]
- Lipofuscin, its origin, properties, and contribution to retinal fluorescence as a potential biomarker of oxidative damage to the retina. Antioxidants (Basel). 2023;12:2111.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]








