Translate this page into:
Lower Limb Nodulo-ulcerative Lesion in Kidney Transplant Recipient – An Unusual Diagnosis
Address for correspondence: Dr. Pankaj Beniwal, 6, New Heera Bagh, Near Kalyan Dharmshala, Jaipur - 302 004, Rajasthan, India. E-mail: pankajbeniwal@hotmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
A 56-year-old kidney transplant recipient presented with a progressive cauliflower-like growth on the plantar surface of the right foot and on workup found to have chromoblastomycosis, which was successfully treated by antifungal agent and surgical excision with no recurrence. Chromoblastomycosis belongs to the heterogeneous group of subcutaneous mycoses. It is caused by various pigmented (dematiaceous) fungi, which gain entry into the skin via traumatic implantation. The case is of interest because it has so far not been reported from the northwest arid zone of India in kidney transplant recipients.
Keywords
Chromoblastomycosis
itraconazole
non-endemic zone
Introduction
Chromoblastomycosis is a subcutaneous fungal infection, which may be caused by a variety of pigmented (dematiaceous) fungi. The infection results from the traumatic implantation of the fungus into the skin. The disease is usually endemic in warm and humid climates and follows the same geographic prevalence in India, too. We would like to share a case report of chromoblastomycosis from Rajasthan, a non-endemic arid zone of India. The case responded favourably to oral itraconazole.
Case Report
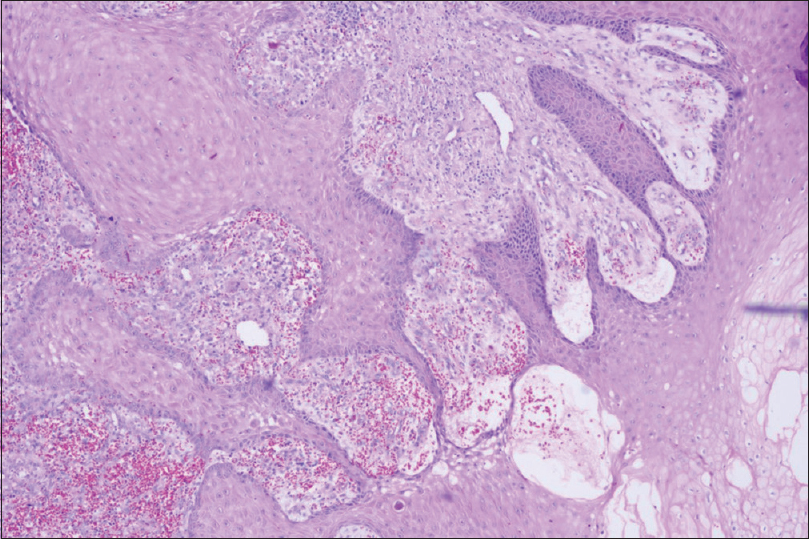
A 56-year-old male underwent successful live donor (spouse) kidney transplantation seven months ago. Induction was given with basiliximab. He was on triple immunosuppression (prednisolone, tacrolimus and mycophenolate mofetil). His clinical course was complicated by new-onset diabetes after kidney transplantation. He presented with a progressive ulcero-proliferative cauliflower-like growth on the plantar surface of the right foot after four months of kidney transplantation. Initially, it was a pea-like nodule which progressed to ulcerative cauliflower-like growth. The patient denied any trauma to that site or travel to an endemic area. Clinical evaluation revealed an ulcero-proliferative fungating lesion measuring 6 × 3.2 cm. The lesions comprised necrotic granulation tissue with an indurated and thickened margin [Figure 1]. There was foul-smelling discharge at places. There was no inguinal lymphadenopathy. The systemic examination was essentially normal. Routine haematological and biochemical parameters and X-ray of the chest were within normal limits. Serum creatinine increased from 1.2mg/dL to 2.8mg/dL. A routine urine examination was normal. Venereal disease research laboratory (VDRL) and enzyme-linked immunosorbent assay (ELISA) for HIV 1 and 2 were negative. HbA1c was 11.4%. USG Doppler of lower limb vessels was normal. The radiological examination did not reveal any bony involvement. The lesions were completely excised and sent for a histopathology examination. With haematoxylin and eosin stain, biopsy material revealed fungal hyphae with characteristic sclerotic bodies in dermis and epidermis [Figure 2]. They were darkly pigmented, thick-walled, round to polyhedral fungal elements that had undergone septation in multiple planes [Figure 3]. They were surrounded by connective tissue and neutrophilic inflammation. Epidermis showed pseudo-epitheliomatous hyperplasia and hyperkeratosis. The inflammatory infiltrate was primarily granulomatous with micro-abscesses.

- Noduloulcerative lesion at foot
- H&E:20x: Round to polygonal fungal elements with thick wall sclerotic bodies
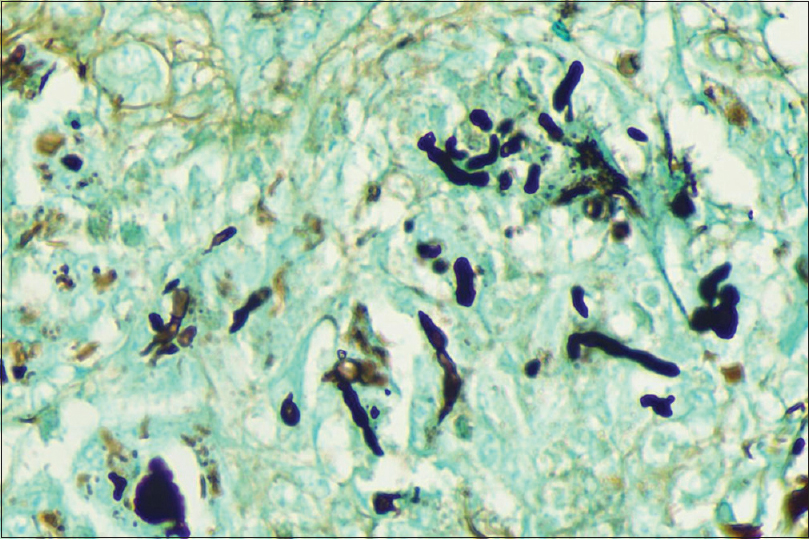
- GMS stain: 20x: silver stain highlights fungal elements including round thick walled sclerotic bodies
These findings are characteristic of chromoblastomycosis. Fungal culture was not done as sclerotic bodies and pseudo-epitheliomatous hyperplasia, highlighting the fungus, was considered sensitive and specific enough to give a diagnosis of cutaneous chromoblastomycosis. The patient was put on oral itraconazole, 100 mg twice daily along with insulin therapy. After 6 months of therapy, the wound healed well and there was no recurrence of the lesion.
Discussion
Chromoblastomycosis is a chronic fungal infection of the skin and subcutaneous tissues caused by dematiaceous or pigmented fungi that are implanted into the dermis from the environment.[1] There are many case reports from different parts of India.[2345] All of these studies show that chromoblastomycosis is prevalent in warm and humid conditions, which is essential for the growth of these fungi. These conditions exist primarily in the sub-Himalayan belt, western and eastern coasts, and southern India,[25] and these regions have been endemic for chromoblastomycosis. Dry climatic conditions do not appear to be favourable for the disease.[2] Diabetes has been reported to be the most common comorbidity in non-immunosuppressed patients.[6] Impaired chemotaxis function in patients with diabetes mellitus might make them prone to infection. Recently, chromoblastomycosis has been increasingly reported in immunosuppressed patients. However, only a few cases of chromoblastomycosis in kidney transplant recipients have been described so far in the global literature.[78910] The incidence of phaeohyphomycosis or chromoblastomycosis has been reported to be 0.54 cases per 100 kidney transplants.[11] What brings interest to this case is that this is probably the first case of chromoblastomycosis in kidney transplant recipients reported from the north-western arid zone of India.
The infection can be caused by a number of fungi, but the vast majority is caused by Fonsacaea pedrosoi and Cladosporium carrionii.[1] F. pedrosoi appears to be the most common etiological agent worldwide, as well as in cases reported from warm and humid regions of India.[121314]
Cutaneous chromoblastomycosis is a localized infection of the skin and subcutaneous tissues (rarely involve underlying bone) that clinically appear in the form of nodules, plaque-like, verrucous, cicatricial or tumorous growth. Ours was a case of cutaneous chromoblastomycosis exhibited noduloulcrative lesion.
Differential diagnoses include cutaneous tuberculosis and all the deep mycoses, including mycetoma, nocardiosis and malignancy. Diagnosis is made by the demonstration of fungus in the lesions. This is done definitively through a culture of causative species on Sabouraud's dextrose agar. However, an easier and more rapid method of diagnosis is bedside demonstration of sclerotic bodies in the KOH examination. Sclerotic or muriform bodies are thick-walled single cells or cell clusters seen as brown-coloured 'copper pennies'. These are pathognomonic for chromoblastomycosis. They can also be detected in routine H&E-stained biopsy specimens.
The therapeutic modalities include itraconazole 200 mg daily, with or without flucytosine (30 mg/kg QID); terbinafine 250 mg daily, and in extensive cases, intravenous amphotericin B. Combination therapy with itraconazole and terbinafine has been shown to be synergistic.[15] In our case too, chromoblastomycosis responded to itraconazole.
In conclusion, the physician should consider chromoblastomycosis in the differential diagnosis of noduloulcerative skin lesions in patients even in a non-endemic area. Our report emphasizes the need for awareness about this disease.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Deep fungal infections. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, eds. Fitzpatrick’s Dermatology in General Medicine (7th Ed). New York: Mc Graw Hill; 2008. p. :1833-5.
- [Google Scholar]
- Chromoblastomycosis in sub-tropical regions of India. Mycopathologia. 2010;169:381-6.
- [Google Scholar]
- Chromoblastomycosis in Kerala, India. Indian J Dermatol Venereol Leprol. 2012;78:728-33.
- [Google Scholar]
- Chromoblastomycosis in Taiwan: A report of 30 cases and a review of the literature. Med Mycol. 2018;56:395-405.
- [Google Scholar]
- Cutaneous chromomycosis in renal transplant recipients.Successful management in two cases. Arch Intern Med. 1985;145:1036-7.
- [Google Scholar]
- Chromomycosis in a European renal transplant recipient. Nephrol Dial Transplant. 1996;11:715-6.
- [Google Scholar]
- Chromomycosis due to Exophiala jeanselmei in a renal transplant recipient. Eur J Dermatol. 2003;13:305-7.
- [Google Scholar]
- Melanized fungal infections in kidney transplant recipients: Contributions to optimize clinical management. Clin Microbiol Infect. 2017;23:333e9-333e14.
- [Google Scholar]
- Chromoblastomycosis: A retrospective study of 325 cases on Amazonic region (Brazil) Mycopathologia. 1998;143:171-5.
- [Google Scholar]
- Chromoblastomycosis: A review of 100 cases in the state of Rio Grande do Sul, Brazil. J Am Acad Dermatol. 2001;44:585-92.
- [Google Scholar]
- Chromomycosis: A clinical and mycologic study of thirty-five cases observed in the hinterland of Rio Grande does Sul, Brazil? Am J Trop Med Hyg. 1976;25:132-5.
- [Google Scholar]
- Chromoblastomycosis in Nepal: A study of 13 cases. Indian J Dermatol Venereol Leprol. 2007;73:176-8.
- [Google Scholar]







