Translate this page into:
Membranous nephropathy as a rare renal manifestation of IgG4-related disease
Address for correspondence: Dr. Anila Abraham Kurien, Center for Renal and Urological Pathology, AL 190, 1st Street, 12th Main Road, Anna Nagar, Chennai - 600 040, India. E-mail: anila_abraham08@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
IgG4-related disease, a newly described immune-mediated disorder with tissue infiltration of IgG4-positive plasma cells, has been reported in nearly every organ. In the kidney, it manifests as IgG4-related tubulointerstitial nephritis (TIN) but may also present as membranous nephropathy. We report a patient with IgG4 renal disease who had membranous nephropathy as well as TIN.
Keywords
IgG4 related disease
membranous nephropathy
secondary membranous nephropathy
Introduction
IgG4-related disease (IgG4-RD) is a recently described multisystemic immune-mediated disorder characterized by tissue infiltration of IgG4 positive plasma cells. It has been described in nearly every organ system of the body.[1] In the kidneys, it usually manifests as IgG4-related tubulointerstitial nephritis (IgG4 TIN). There has been occasional case reports of glomerular diseases associated with IgG4-RD.[2] Membranous nephropathy was the most frequently reported glomerular lesion in IgG4-RD. IgA nephropathy/Henoch-Schonlein purpura and membranoproliferative glomerulonephritis are other[234] glomerular diseases. Other renal lesions related to IgG4 disease included ureteral inflammatory pseudotumor, retroperitoneal fibrosis causing hydronephrosis and chronic sclerosing pyelitis.[2]
We describe a patient of IgG4-RD with membranous nephropathy as well as associated IgG4 TIN with advanced renal dysfunction. To the best of our knowledge, this is the first case report from India. Our case illustrates that IgG4-related membranous nephropathy is a distinct form of secondary membranous nephropathy.
Case Report
A 54-year-old man, a known diabetic for 6 years presented with a 2 week history of pedal edema, puffiness of the face and generalized body swelling. Clinical examination revealed severe anemia, pedal edema, ascites and bilateral pleural effusion. His blood pressure was 120/80 mmHg. There was no jaundice, cyanosis or lymphadenopathy. Systemic examination did not reveal any organomegaly, any particular area of tenderness, or any evidence of peripheral neuropathy or focal neurological deficit. History was negative for arthralgia, arthritis, any skin rash, abdominal pain and hemoptysis. Urine routine examination showed 3+ proteinuria with bland urinary sediment. 24-h urine protein was 8.3 g and serum creatinine was 7.4 mg/dl. Patient had hemoglobin of 6.3 g/dl. Peripheral blood smear showed normochromic normocytic red blood cells. Total and differential leukocyte counts and platelet count were normal. Coagulation profile was normal. Liver function test revealed total bilirubin of 1.2 mg/dl, SGPT of 19 IU/L, SGOT of 24 IU/L and ALP of 152 IU/L. Total protein was 7.1 mg/dl and albumin of 3.8 mg/dl. Ultrasonography abdomen did not show hepatosplenomegaly; pancreas was normal, there were no intra-abdominal or retroperitoneal mass, right kidney was 9.8 cm, left kidney was 10.6 cm, with normal echotexture and preserved corticomedullary differentiation. His serum protein electrophoresis study was normal. Patient's serum tested negative for hepatitis B surface antigen, antibodies for hepatitis C virus and human immunodeficiency virus-I/II. Antinuclear antibody, anti-neutrophilic cytoplasmic antibody (pANCA and cANCA) and anti-glomerular basement membrane (GBM) antibody were negative. Serum complement levels were normal (C3 = 104 mg/dl and C4 = 29 mg/dl).
A clinical diagnosis of primary idiopathic glomerular disease was considered as the patient did not have any evidence of diabetic retinopathy or neuropathy. The syndromic diagnosis was rapidly progressive renal failure. The patient was put on IV methyl prednisolone and his urine output improved gradually. A kidney biopsy was done and examined by light, immunofluorescence and electron microscopy. By light microscopy, there were 10 glomeruli, 6 of which were globally sclerotic. The capillary loops were thickened and the basement membranes showed spike formation and pinhole lesions on methenamine silver stain [Figure 1]. Endocapillary or mesangial hypercellularity, crescent formation or fibrinoid necroses were not observed. There was diffuse, severe interstitial fibrosis with a moderate chronic inflammatory cell infiltrate containing numerous plasma cells [Figure 2]. Immunofluorescence study revealed global granular GBM staining for IgG (+3), C3 (+2) and both kappa and lambda light chains (+2). Granular focal tubular basement membranes staining for IgG (+3) was also noted. Electron microscopic evaluation showed subepithelial electron-dense deposits, confirming the diagnosis of membranous nephropathy.
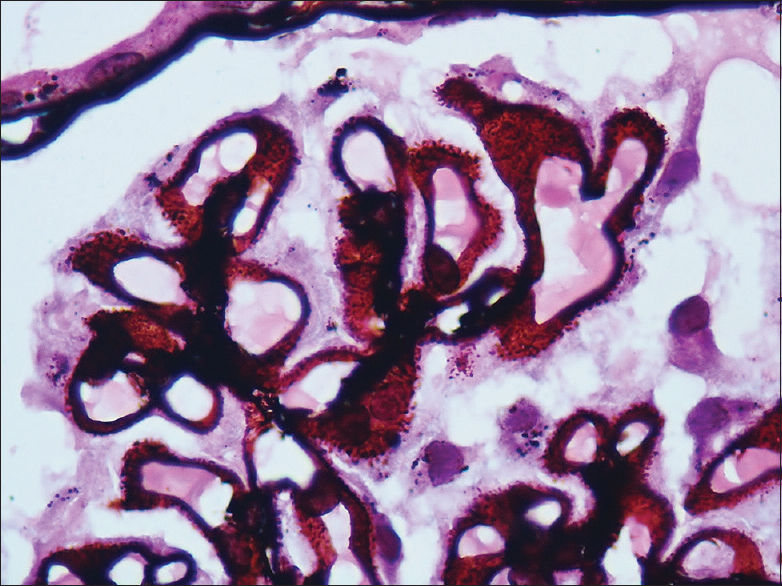
- Glomerular basement membrane shows spike formation on methenamine silver stain
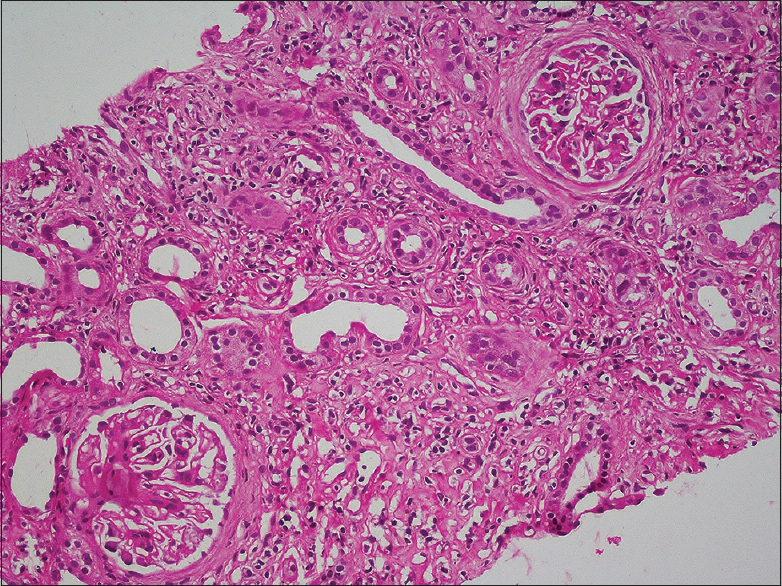
- Chronic inflammatory cell infiltrate containing numerous plasma cells in a fibrotic interstitium (H&E stain)
Immunohistochemical stain for IgG4 showed numerous positive areas, many with more than 30 plasma cells positive for IgG4/high power field (hpf) [Figure 3]. The current consensus is that presence of >10 cells/hpf is diagnostic of IgG4-RD.[2] Immunostaining for antiphospholipase A2 receptor (PLA2R) antibody was performed [Figure 4]. It was negative in this patient, consistent with a secondary etiology for membranous nephropathy. A diagnosis of IgG4-related membranous nephropathy and IgG4 TIN was made. Serum IgG4 level and IgG4/IgG ratio done subsequently were elevated, confirming the diagnosis. Non-contrast computed tomography scan of abdomen was normal. Steroid therapy was continued for 3 months but was tapered off in view of worsening diabetes. His creatinine stabilized at around 3.5 mg/dl.
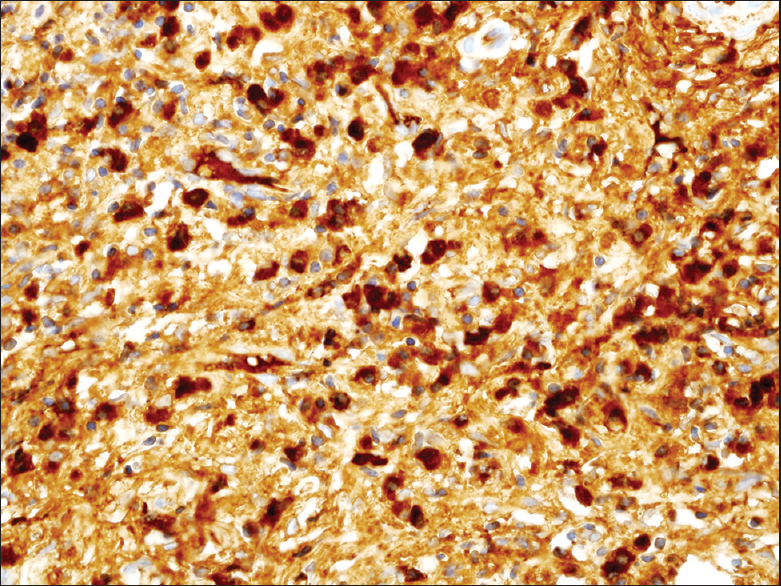
- IgG4 immunostaining shows positive plasma cells in the interstitium
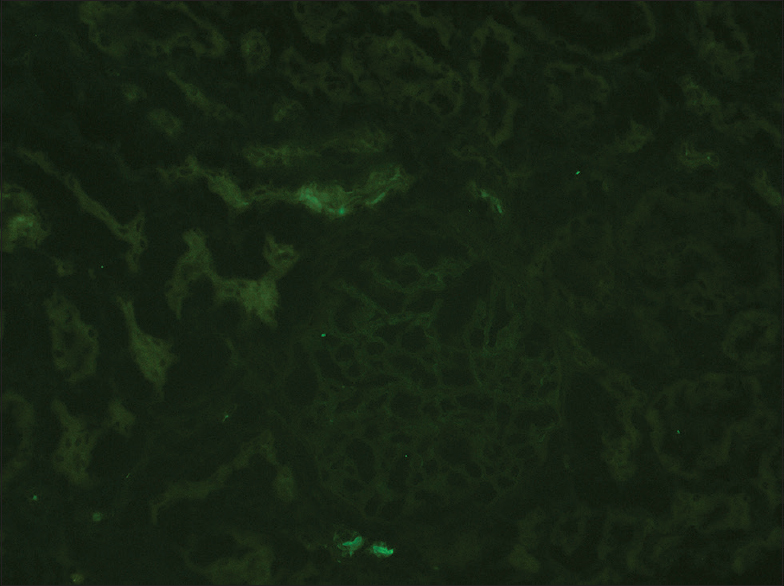
- Negative immunostaining for antiphospholipase A2 receptor antibody
Discussion
Membranous nephropathy may be primary or secondary to a variety of causes. One of the major causes of primary membranous nephropathy is the development of antibodies against a podocyte antigen, M-type PLA2R.[5] Autoimmune disease, infections, neoplasms and drugs are the main etiologic factors of secondary membranous nephropathy. Recently, a series of published literature suggested that IgG4-RD is another systemic disease, which is an etiological factor for secondary membranous nephropathy.[6] In 2011, the international symposium on IgG4-RD in the nomenclature consensus statement termed membranous nephropathy secondary to IgG4-RD as “IgG4-related membranous nephropathy”.[7] Anti-PLA2R antibody staining is a useful marker for differentiating primary from secondary membranous nephropathy in adults.[8] Anti-PLA2R antibody staining was negative in this patient, as is expected in a case of secondary membranous nephropathy. Work up on our patient did not reveal any evidence of underlying autoimmune disease, infection or malignancy. No drug history was elicited. Considering a background of secondary membranous nephropathy, we attribute it to IgG4-RD because the following diagnostic criteria were fulfilled.[9]
-
Clinical criteria of nephrotic syndrome with renal dysfunction
-
High serum IgG4 level and high IgG4/IgG ratio
-
Histological picture of membranous nephropathy confirmed by electron microscopy study along with interstitial fibrosis and dense infiltration of IgG4 positive plasma cells.
The etiopathogenesis of membranous nephropathy developing in the setting of IgG4-RD is unclear. A hypothesis put forward by Fervenza et al. is that the proliferating plasma cells produce IgG4 that is autoreactive against podocyte antigens.[10] Kuroki et al. also showed that type 2 helper T-cell cytokines cause IgG4 production by increasing and stimulating B-cells in membranous nephropathy as well as in other IgG4-related sclerosing lesions.[11]
Patients with IgG4 TIN and membranous nephropathy usually have other organ involvement.[412] A unique feature of this case is that there was no clinical, radiological or histologic evidence of systemic involvement, and the IgG4-RD was limited to the kidney. In the largest case series of IgG4 membranous nephropathy, 7 out of 9 patients had evidence of other organ involvement.[6] The two remaining patients in the series who did not have systemic disease had typical features of IgG4 TIN on biopsy, similar to our patient. Our case along with the previously published cases[313] suggests that membranous nephropathy is one of the renal manifestations of IgG4 disease, distinct from IgG4 TIN.
The indication for biopsy in our patient was acute renal failure with proteinuria. We suggest that in the presence of nephrotic range proteinuria with IgG4 TIN on biopsy, the possibility of associated IgG4-related membranous nephropathy must be considered.
Conclusions
Membranous nephropathy is one of the renal manifestations of IgG4 disease. IgG4-related membranous nephropathy adds to a newly recognized form of secondary membranous nephropathy. The possibility of associated IgG4-related membranous nephropathy must be considered in the presence of proteinuria in patients with IgG4 TIN on biopsy.
Source of Support: Nil
Conflict of Interest: None declared.
References
- IgG4-related disease: A cross-sectional study of 114 cases. Am J Surg Pathol. 2010;34:1812-9.
- [Google Scholar]
- Membranous nephropathy associated with IgG4-related systemic disease and without autoimmune pancreatitis. Clin Nephrol. 2009;71:173-8.
- [Google Scholar]
- Membranous nephropathy: A rare renal manifestation of IgG4-related systemic disease. Clin Nephrol. 2012;77:321-8.
- [Google Scholar]
- M-type phospholipase A2 receptor as target antigen in idiopathic membranous nephropathy. N Engl J Med. 2009;361:11-21.
- [Google Scholar]
- Membranous glomerulonephritis is a manifestation of IgG4-related disease. Kidney Int. 2013;83:455-62.
- [Google Scholar]
- Recommendations for the nomenclature of IgG4-related disease and its individual organ system manifestations. Arthritis Rheum. 2012;64:3061-7.
- [Google Scholar]
- Determination of primary versus secondary membranous glomerulopathy utilizing phospholipase A2 receptor staining in renal biopsies. Mod Pathol. 2013;26:709-15.
- [Google Scholar]
- Are classification criteria for IgG4-RD now possible. The concept of IgG4-related disease and proposal of comprehensive diagnostic criteria in Japan? Int J Rheumatol. 2012;2012:357071.
- [Google Scholar]
- IgG4-related tubulointerstitial nephritis with membranous nephropathy. Am J Kidney Dis. 2011;58:320-4.
- [Google Scholar]
- Th2 cytokines increase and stimulate B cells to produce IgG4 in idiopathic membranous nephropathy. Kidney Int. 2005;68:302-10.
- [Google Scholar]
- Membranous nephropathy associated with IgG4-related disease. Am J Kidney Dis. 2011;58:272-5.
- [Google Scholar]
- Membranous nephropathy with repeated flares in IgG4-related disease. Clin Kidney J. 2013;6:204-07.
- [Google Scholar]







