Translate this page into:
Meningioma in long-term survivor after renal transplantation
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
A 50-year-old man received a renal allograft from his brother in August 1999. He had 3 out of 6 human leukocyte antigen (HLA) match with two HLA-DR mismatches. The time since dialysis to transplantation was 18 months. He was immunosuppressed with prednisolone (10 mg/day), and azathioprime (2 mg/kg/day) with stable graft function (serum creatinine 1 mg/dl).
Twelve years after renal transplantation (RTx), he developed focal followed by generalized seizures. There was no history of fever/weight loss.
Laboratory investigations revealed normal complete blood count, liver function tests with no proteinuria. Enzyme-linked immunosorbent assays test for human immunodeficiency virus, hepatitis B surface antigen, and hepatitis C virus were negative. The polymerase chain reaction ruled out cytomegalovirus, herpes simplex virus, varicella zoster virus, Epstein-Barr virus (EBV) infection, human herpesvirus (HHV) 8, and human papiloma virus (HPV).
Magnetic resonance imaging (MRI) showed well-defined homogenously enhancing extra-axial space occupying lesion involving right parietal parasagital region adjacent to superior sagittal sinus with of possibility of meningioma [Figure 1]. Resection of tumor was performed by neurosurgeon. Gross examination revealed tumor brown to grey white colored friable tissue of size 3.5 cm × 3 cm. Histopathology [Figure 2] revealed benign meningotheliomatous tumor arranged in whorls and clusters maintaining lobular arrangement. The individual cells are round to polygonal with delicate round to oval nuclei, eosinophilic cutoplasm, and indistinct cytoplasmic boarders. The cells tended to elongation and streaming and showed globular hyaline, periodic acid-Schiff stain (PAS) positive inclusions (psedopsamoma bodies). Tumor cells were not infiltrating the bony tissue.
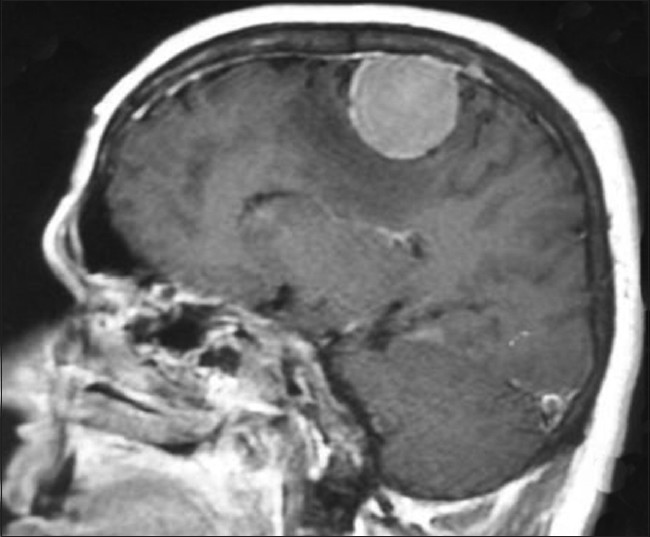
- Magnetic resonance imaging showed well defined homogenously enhancing extra-axial space occupying lesion involving right parietal parasagital region adjacent to superior sagittal sinus with possibility of meningioma
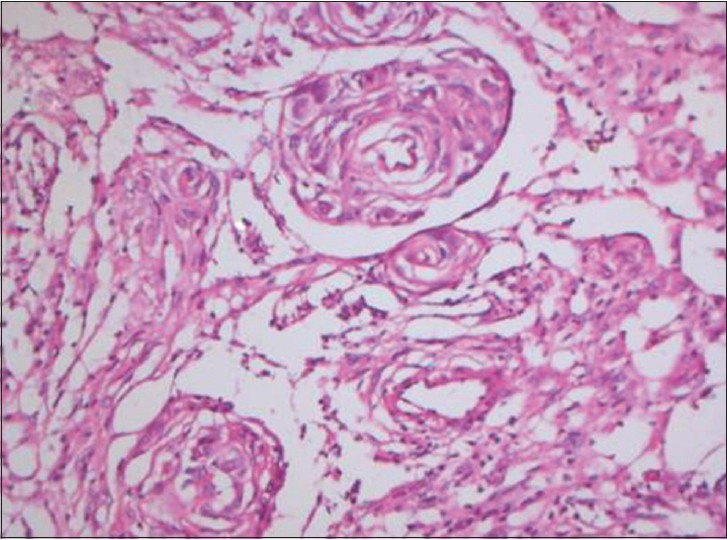
- Histopathology revealed benign meningotheliomatous meningioma
He showed good recovery, and was fully active, able to carry on all pre-disease performance without restriction. The Eastern Cooperative Oncology Group performance status was grade 0. He was able to carry on normal activity and to work; no special care needed. The Karnofsky performance status scale was 90. His seizure was controlled on oral phenytoin. Patient was asymptomatic with stable renal allograft function 1 year after surgery.
The high incidence of secondary malignancies among transplant recipients are due to extent and duration of immunosuppression (calcineurin inhibitors and azathioprine > sirolimus), viral infection (EBV, HHV 8, HPV, and Merkel cell polyomavirus), sun exposure, and pre-transplantation dialysis.[1–5] Among solid tumors, several cases of malignant brain tumors have been described but no benign tumors.[1–5]
To the best of our knowledge, this is the first reported case of meningiomas in after RTx. This report, thus adds the diagnosis of meningioma to the list of possible problems in long-term survivors.
References
- Spectrum of cancer risk among US solid organ transplant recipients. JAMA. 2011;306:1891-901.
- [Google Scholar]
- Effect of long-term immunosuppression in kidney-graft recipients on cancer incidence: Randomised comparison of two cyclosporin regimens. Lancet. 1998;351:623-8.
- [Google Scholar]
- Posttransplant lymphoproliferative disorders of the central nervous system after kidney transplantation: Single center experience over 40 years. Two case reports. Neurol Med Chir (Tokyo). 2010;50:1079-83.
- [Google Scholar]
- Primary cerebral lymphoma following+kidney transplant: A case report and review of the literature. Rev Med Chil. 1994;122:1294-7.
- [Google Scholar]
- Cancer in renal allograft recipients in Australia and New Zealand. Transplant Proc. 1977;9:1133-6.
- [Google Scholar]






