Translate this page into:
Nature’s Cure or Kidney Curse? The Nephrotoxic Potential of Indigenous Remedies
Corresponding author: Urmila Anandh, Department of Nephrology, Amrita Institute of Medical Sciences and Research Centre, Faridabad, India. E-mail: uanandh@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sethi J, Anandh U, Jha V. Nature’s Cure or Kidney Curse? The Nephrotoxic Potential of Indigenous Remedies. Indian J Nephrol. 2025;35:335-42. doi: 10.25259/IJN_321_2024
Abstract
Traditional medicine refers to a diverse range of health and healing practices used by Indigenous peoples that incorporate plants, animals, and the spiritual realm for the diagnosis and treatment of illness or maintenance of health and well-being. While these practices hold significant cultural value, there is growing evidence of potential nephrotoxicity associated with some traditional indigenous medicines (TIMs). In this review, we explore the various clinical manifestations of nephrotoxicity induced by TIMs. Nephrotoxicity can result from various factors, including the intrinsic toxicity of certain herbs, contamination with heavy metals, inappropriate dosages, and interaction with conventional medications. This review highlights the importance of monitoring kidney function in patients using TIMs and calls for increased awareness and regulation to ensure the safe use of these traditional therapies.
Keywords
Acute kidney injury
Herbal
Indigenous
Nephrotoxicity
Traditional medicines
Introduction
Disparities in healthcare access in the developing world often lead to the use of traditional medicines in the treatment of not only common ailments but serious medical conditions as well. These traditional medicines have been associated with nephrotoxicity but rarely documented in modern literature, as these alternative medical systems and therapies are more often prevalent in the remote areas of developing countries.1,2 Herbs are the most common constituent of these remedies and are often sourced locally and the medications prepared in-house.3 The World Health Organization (WHO) estimates that 80% of the population of Asian and some African countries presently use herbal medicine for some aspect of primary healthcare. In developing countries like India, 65% of rural communities still use a traditional form of medicine to fulfill their primary healthcare needs.4 The WHO and the Government of India recently signed an agreement to establish the WHO Global Centre for Traditional Medicine that aims to harness the potential of traditional medicine from across the world through modern science and technology. The National Rural Health Mission has also decided to mainstream the Ayurveda, Yoga, Naturopathy, Unani, Siddha, and Homeopathy (AYUSH) system of indigenous medicine to help meet the challenge of shortage of healthcare professionals and strengthen the delivery system of the healthcare service in India.5
These traditional medicines are cheap, accessible, natural, and considered relatively safer than modern medicines. However, with the increasing use of these medications, the incidence of nephrotoxicity is becoming increasingly apparent. It is estimated that traditional remedies account for up to 35% of cases of acute kidney injury (AKI) in the developing world.2 Even in developed countries, herbal medicines accounted for approximately 26% of all alternative medicine use.3 The true incidence of chronic kidney disease (CKD) secondary to herbal medicines is not known because of the challenges in the diagnosis of CKD in this subset of patients.3 In a survey from Africa, the prevalence of traditional medicine use among adults with CKD was 70.3%.6 A cross-sectional study from Taiwan showed that herbal therapy use was associated independently with the development of CKD.7
Various epidemiological studies and chemical examination of herbal medicines have led to the identification of the culprit chemical compound, as illustrated in cases of AA-associated Chinese herb nephropathy/Balkan nephropathy.8 Besides various organic acids and alkaloids, use of heavy metals (deliberately used for contamination during production) in traditional herbal medications have been implicated in nephrotoxicity.9 Renal syndromes associated with traditional indigenous medicines (TIMs) include dyselectrolytemia, Fanconi syndrome, AKI, rhabdomyolysis, CKD, nephrolithiasis, urothelial malignancy, proteinuric kidney disease, and lupus nephritis. Figure 1 depicts the different clinical syndromes caused by indigenous medicines.
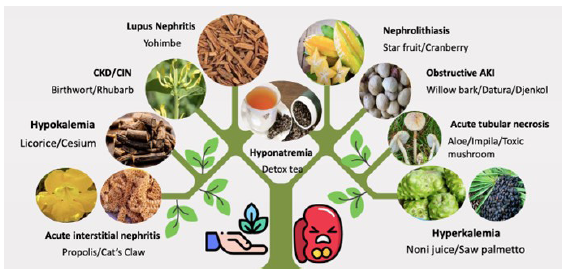
- Various kidney syndromes caused by traditional medicines. AKI: Acute kidney injury, CKD: Chronic kidney disease, CIN: Chronic interstitial nephritis.
Nephrotoxic Clinical Syndromes with Indigenous Medications
Electrolyte disturbances
Electrolyte disturbances can occur in the use of herbal medications. Unauthorized herbal juices can cause hyperkalemia, especially in patients with CKD. Use of noni juice (Morinda citrifolia) has been shown to cause hyperkalemia, because the herb contains a very high level of potassium (56.3 meq/L) similar to that of orange or tomato juice.10 Besides hyperkalemia, alternative medication use10–15 has been shown to cause other forms of electrolyte abnormalities [Table 1].
| Alternative product/herb | Electrolye/acid base abnormality | Indication of use |
|---|---|---|
| Glycyrrhiza glabara (licorice) | Hypokalemia/pseudoaldosteronism, hypertension, and metabolic alkalosis |
Chinese herbal tea marketed as cough suppressant Korean herbal tonic marketed for prostate cancer |
| Cesium chloride | Hypokalemia | Alternative and complementary cancer treatment |
|
Morinda citrifolia (noni juice) |
Hyperkalemia | Nutritional supplement |
| Serenoa repens (saw palmetto) | Hyperkalemia | Remedy for benign prostatic hyperplasia |
| Oolong tea (detox tea) | Hyponatremia | Weight loss supplement |
| Colon cleanser | Hyponatremia | Enema |
Fanconi syndrome
Fanconi syndrome was one of the earliest renal manifestations recognized with the use of Aristocholic Acid (AA), wherein the use of Chinese herbs leads to the clinical symptoms of hypokalemic periodic paralysis. A Chinese herbal remedy (Akebia 14) has been reported to cause reversible Fanconi syndrome. This medicine, marketed as herbal weight loss supplement, also contains high quantities of AA. Patients on these herbal remedies usually present with severe body pains, myopathy, and on evaluation have hypophosphatemia, hypouricemia, glucosuria, generalized aminoaciduria, and tubular proteinuria, the five cardinal symptoms of the Fanconi syndrome. Renal biopsy done in some of these reports has shown interstitial edema, focal tubular atrophy fibrosis, and glomerular ischemic damage. Usually, Fanconi syndrome is reversible when the herbal drug is withdrawn. In some cases, prolonged use of these herbs has led to progressive renal failure.16,17
Rhabdomyolysis
Rhabdomyolysis, secondary to the intake of herbal medications, have been reported in literature, especially with medications prescribed for weight loss. Case reports of increasing creatinine phosphokinase (CPK) associated with herbal medicines are also discussed in literature. Elevated CPK is indicative of muscle breakdown, which is the mechanism by which these herbal medications achieve weight loss.18 Many nonregulated herbal medications used for regulating menstrual cycles (Vitex) and alleviating some of the premenstrual symptoms have shown to cause rhabdomyolysis.19 In other instances, herbal drugs interact adversely with modern medicines and can cause rhabdomyolysis. CPK should be checked in all patients with muscle aches and pains in patients on herbal medications. In most cases, the muscle destruction reverses with the discontinuation of the traditional medicine. Rhabdomyolysis, caused by contaminated/substituted herbal hair dyes, can cause severe AKI and death. Physicians should be aware of the potential side effects of many herbal medicines and measure serum CPK enzyme for patients who admit using weight loss herbs and present with AKI.
Acute kidney injury
AKI is a common manifestation with the use of traditional medicines. The acute injury can manifest either as acute tubular necrosis or as acute interstitial nephritis. Indigenous medicines form the backbone for the treatment of common ailments like menstrual problems, fertility issues, malaria, typhoid, and more in developing nations. Treatment with these unregulated therapies often causes AKI. Around one-third cases of AKI are caused by the consumption of traditional medications.20,21 Similar situation exists in rural India where a majority of the population depend on traditional healers and therapies.21
AKI may be the only manifestation of the herbal medications. In certain cases, AKI is accompanied with hepatotoxicity, neurological manifestations, bleeding diathesis, and respiratory failure. Patients usually present with severe gastroenteritis, dehydration, and shock. AKI is usually consequent to severe intravascular volume depletion. These patients often have very high mortality.22 In other instances, AKI is secondary to the contamination of the traditional folk remedy with nephrotoxic chemicals. A classic example of AKI being secondary is the ingestion of “holy water.” This liquid is often laced with copper sulphate giving its distinct color which leads to intravascular hemolysis and AKI.23 Contamination with potassium bromide, potassium dichromate, aloe, phyllum resin, phenolphthalein, and carbon tetrachloride has also been reported in literature.24 Adulteration of traditional medicines happens during the process of manufacture. Many over-the-counter Chinese herbal and nutritional supplements are mixed with ephedrine, chlorpheniramine, sildenafil, steroids, fenfluramine, phenacetin, and so on and so forth. Ten percent of these supplements have undeclared drugs and heavy metals.25,26 This chemical adulteration is done to enhance the efficacy of the remedy, and in some instances, the contamination is unintentional. This accidental contamination of herbal medicines happens when these plants are grown in highly polluted soil.27
AKI can also develop if the traditional remedies are introduced into the human body in an unusual manner. Use of herbal enemas in Africa have been associated with acute renal failure. Herbal enemas are very popular, and members of the Zulu tribe often have three enemas a week. These practices cause colonic complications leading to dehydration, infection, bleeding, and shock. AKI is a common consequence.28
Occasionally, AKI is seen when the original herbal product is replaced with a natural substitute. Mixing henna with paraphenylenediamine in hair dye can cause negative effects. Severe allergic reactions and rhabdomyolysis is reported leading to AKI.29 In Morroco, hair is often dyed with a powder made from takaout el badia (made from the seeds of Tamaris orientalis). In situations of scarcity, the original powder is replaced with takaout roumia. Takaout roumia contains paraphenylenediamine which is responsible for rhabdomyolysis and AKI.30 This product is responsible for 10% of AKI in Morrocco.
Another common situation where AKI develops is when the patient simultaneously consumes modern medicines and traditional herbs. The interaction between the drugs sometimes leads to unexpected renal consequences. Use of cyclosporine and St John’s wort (derived from Hypericum perforatum) causes induction of cyclosporine metabolism. St John’s wort induces cytochrome P 450 enzyme, the enzyme responsible for cyclosporine metabolism. Low cyclosporine levels can precipitate allograft rejection and AKI.31
Artemisia herba (white wormwood) is used in folk medicine in many parts of Europe for its antihelmintic/antirheumatic properties. It can lead to AKI by osmotic nephrosis. Similarly, extracts of Euphorpbia paralias (sea spurge) is used in Europe and North Africa for treating cancer and infections. This herb can lead to AKI due to severe acute tubular necrosis.32
Besides herbs, animal products and extracts have been also implicated in the development of AKI.33–40 Common example is propolis, a resinous product sourced by honey bees to build their hives.This substance is used as an antiseptic anti-inflammatory agent, anesthetic, antioxidative, hepatoprotective substance in South America over the ages. Various chemicals like aromatic acids, esters, flavonoids, benzyl cinnamate, methyl cinnamate make up propolis, but it is difficult to pinpoint the guilty chemical compound responsible for AKI. Even though systemic toxicity secondary to use of propolis is rare, there are case reports of acute renal failure following propolis ingestion.41
Gall bladder extract of various fishes, especially carp, is commonly used in folk therapies in Asia (China, Taiwan, Hong Kong, Japan, South Korea, and India). The fish bile is used as a cough expectorant as well as for its antipyretic, antihypertensive and anti-allergic effects. Symptoms appear very early after ingestion of the offending bile, which includes watery diarrhea, jaundice, bradycardia,hypotension, and oligoanuria.The development of AKI is attributed to the cardiotoxicity of bile. Renal failure sets in within two days and often lasts for two to three weeks.42
Bile extract of sheep is also consumed for its medicinal value in Saudi Arabia. It is used as a treatment for diabetes mellitus. Use of sheep bile daily over weeks causes nausea and diarrhea. Intravascular volume depletion is responsible for the acute decline in kidney function. AKI is often associated with hyponatremia and metabolic encephalopathy.43 Cases declined after the intake of sheep bile was regulated by the government of Saudi Arabia.
Chronic kidney disease
Acute deterioration of renal function secondary to folk medicine is easy to recognize the progressive decline of renal function because the long-term consumption is often difficult to detect. Hence, the incidence of CKD secondary to herbal medicines is underreported. Despite the limitations in establishing causality, there are several reports of herbs which have been implicated in the development of CKD.3 The chronic decline can be because of parenchymal fibrosis or may be a manifestation of nephrolithiasis. Long-standing CKD can progress to the acquired cystic kidney disease or the offending medication can cause cysts de novo. An undesirable and unwanted consequence of herbal medicine-induced CKD is the development of urothelial carcinoma. The commonest and most well-researched herb leading to the development of CKD is AA, a toxic constituent of the Chinese herb nephropathy.
Besides AA, there are other herbs which have been associated with progressive irreversible deterioration of kidney function. Leaves of a creosote bush (Larrea tridentata) are commonly used as tea in North America, popularly known as chaparral tea. The roots and leaves are also marketed in the form of capsules and tablets. The active substance nordihydroguaiaretic acid is thought to have anticancer properties. Prolonged consumption of chaparral tea has led to the development of renal cysts and CKD.44,45 In the modern world, licorice (Glycyrrhiza glabra) is a common constituent of lozenges and its extract is commonly used in alleviating the symptoms of epigastric discomfort and heartburn. It is known to cause hypokalemia (apparent mineralocorticoid excess). Prolonged hypokalemia leads to the development of hypokaemic nephropathy (a form of progressive interstitial injury).46 Yohimbine, an extract from Pausinystalia yohimbe, is used as a folk remedy for erectile dysfunction. Use of this herbal extract causing a clinical illness similar to systemic lupus erythematosus and CKD has been reported in literature.47 Bladderwrack is a large brown algae (Fucus vesiculosus) used as food in Japan. In Europe, it is marketed as herbal medicine for the treatment of atherosclerosis, heartburn, constipation, bronchitis, emphysema, urinary tract disorders, anxiety, and blood cleansing. CKD has been reported when bladderwrack tablets are consumed long term.48 Similar manifestation of chronic decline of kidney function is noted when the Chinese herb rhubarb containing anthraquinone derivatives (Rhizoma rhei) is used as a slimming pill.49
The autopsy of the famous music composer Ludwig van Beethoven revealed the presence of papillary necrosis.50 Papillary necrosis was postulated to be because of the chronic intake of willow bark (Salix daphnoides). The bark contains salicin which is metabolized to a well-known prostaglandin inhibitor—salicylate. Chronic ingestion of salicylic acid is known to cause papillary necrosis (chronic analgesic nephropathy).
Traditional herbal supplements may contain ethylene or diethylene glycol-based solvents that may lead to chronic oxalate nephropathy.51 A thorough medication history should be obtained in patients with rapid decline of kidney function, even in the presence of known risk factors for CKD.
Chronic kidney disease of unknown etiology and herbal medications
In the last decade, clusters of cases with unexplained CKD were reported in various parts of the world (Central America, India, Sri Lanka, etc.).52,53 These clusters were often in hot tropical climates, which predominantly affected farmers. These groups were in the underdeveloped part of the world with limited access to state-of-the-art healthcare facilities. The cause of CKD of unknown origin is still not clear and appears to be multifactorial. The World Health Organization realizes that the relatively common use of herbal medications in these affected areas may be contributing in the decline of renal function and has recommended restricting the use of herbal medicines in these regions.54
Glomerular disease
Glomerular disease, secondary to the use of traditional Indian medications, has been reported in literature. The development of florid membranous nephropathy (MN) and minimal change disease (MCD), secondary to medicines prepared by practitioners of siddha and Ayurveda (a form of traditional medicine), has gained attention with the publication of reports in the last two years. These traditional healers combine herbs and inorganic chemical compounds such as sulfur and mercury in their medicinal preparations. The toxicity of these remedies is often because of the metal constituent. The drugs were used for a variety of indications like sinusitis, skin lesions, bronchitis, and breast cancer. These TIMs have been associated with neural epidermal growth factor-like 1 (NELL-1)-related membranous glomerulonephritis (MGN). Analysis of Swasa kalpa (a common Siddha medicine) showed higher than permissible mercury content.55 Previously, another report from India documented the development of MN in patients who were taking a herbo-mineral combination called rasagenthi mezhaku. The mercury content of this indigenous medication varied from 0.9% to 1.31%. The drug is available as 500 mg capsule and the prescribed dose is two tablets a day. The daily intake of two tablets a day led to a daily intake of 9–13.1 mg of mercury, which is much higher than the daily permissible limit (0.003 mg/day).56 Heavy metals are mixed with herbs in various folk remedies not only in India, but in other parts of the world as well. In some studies, the levels of nephrotoxic heavy metals are more than the safe limits as required by regulatory authorities.57
Lupus nephritis
Indigenous medicines have immunomodulatory potential. Use of these drugs has been associated with various autoimmune conditions. CKD with a lupus-like presentation has been reported.47 A recent report documents the development of lupus nephritis in a patient on herbal medicine. The patient was taking a drug called “super kidney” for diuresis. The unregistered drug contained ginseng, Plantaginis folium, orthosiphonis, Strobilanthi folium, and Retrofacti fructus. The patient’s clinical condition did not completely improve with the cessation of the offending drug and she required immunosuppressive treatment.58
Nephrolithiasis
Herbal medicines have been extensively researched for their antilithogenic potential. Some herbs when used inappropriately can cause both acute crystal-induced AKI and chronic nephrolithiasis. The most common example of crystal-induced tubular obstruction is secondary to the consumption of Djenkol beans—Archidendron pauciflorum (Djenkolism). Acute toxicity of Djenkol beans can cause hematuria and AKI.59 Djenkolic acid is a sulfur-rich cysteine thioacetal of formaldehyde and forms intratubular crystals in the distal tubule of the nephron. These crystals then form the nidus for renal calculi (Djenkolic acid stones) formation. Progressive urolithiasis causes obstructive uropathy and chronic interstitial nephritis.60,61 Another herbal medicine implicated in kidney stone formation is an appetizing fruit called star fruit (Averrhoa carambola). This fruit is used in the therapy of skin ailments and anxiety. Star fruit has very high levels of oxalic acid and can cause stones if consumed in large quantities.62 The Chinese medicinal herb Ma Huang-derived Ephedra sinica is used for the treatment of bronchitis and nasal congestion. The chemical constituent Ephedrine is widely used in modern medicines. It is not only a popular medicine in China but also in India, and is considered to be the “somarasa” in Rigveda. Consumption of Ma Huang in large quantities with very little water can cause renal stone formation.63,64 Cranberry (Vaccinium macrocarpon) juice is widely considered a popular home remedy for recurrent urinary tract infection in the modern world. However, regular use of the concentrate which has high levels of oxalic acid can potentially cause urolithiasis.65
Urothelial carcinoma
Urothelial malignancies happen when the transitional cell layer of the urinary tract mutate and multiply in an unregulated manner. Besides smoking, exposure to chemicals plays an important causative role. Environmental exposure of carcinogenic aromatic amines can happen when vulnerable individuals are exposed to various chemical industries. Other common and rarely appreciated mechanism is the contamination of the soil with these chemicals. Also in countries where herbal medication’s use is in vogue, bladder cancer has been caused by the mutations secondary to AA intake. The highest incidence of urothelial cancers in the upper urinary tract is in Taiwan, where herbal medicines containing AA are used extensively.66 The epidemiology of these cancers is remarkably similar to that noted in Balkan countries.67 This increase in the incidence of urothelial cancer in the last two decades in Taiwan is because of the replacement of original herbs with Aristolochia manchuriensis and Aristolochea fangchi.68 Urothelial carcinoma is often a late complication of AA intake and often manifests in patients who have developed end-stage kidney disease. Also, the continuous consumption of Chinese herbs by CKD patients on dialysis increases their risk of developing urothelial carcinoma.69 There are studies where urothelial cancer has developed relatively early in CKD patients who were not yet on dialysis.70 Over the last two decades, governments are imposing ban on Chinese herbal products containing AA as their mutagenic potential is becoming clearer. This regulatory practice is impacting the incidence of upper urothelial cancer favorably.71 The herbs and their constituents causing various clinical syndromes is summarized in Table 2.
| Herbal plant | Clinical manifestation | Indication of use |
|---|---|---|
| Acute kidney injury | ||
| Aloe capensis (cape aloe) | Abdominal pain, hemorrhagic gastroenteritis/acute tubular necrosis in biopsies | Hypertension, arthritis |
| Callilepis laureola (Impila) | Abdominal pain, diarrhea, acute tubular necrosis, oliguric AKI, hepatic dysfunction, hypoglycemia, metabolic acidosis | To induce fertility, to correct impotence, and to ward off “evil spirits” |
| Catha edulis (Khat) | Acute tubular necrosis | Khat leaf chewing is a local habit in some African populations. Also used as folk remedy for obesity and depression |
|
Colchicum autumnale (Meadow saffron) |
Gastroenteritis/multiorgan failure/hepatic injury/shock/ AKI | Used for acute gouty arthritis-Suicidal colchicine tablet overdose is the most common cause of colchicine poisoning |
| Glycyrrhiza glabara (Licorice) | Contains glycyrrhetinic acid- can lead to hypokalemia, rhabdomyolysis, ARF, pseudoaldosteronism | Cough remedy |
|
Amanita phalloides (Toxic mushrooms) |
Gastroenteritis, hepatic failure, AKI | Accidental ingestion, Anti-cancer, anti-inflammatory |
| Caprica papaya (papaya leave) | Severe mucositis and gastritis leading to severe dehydration causing pre-renal AKI | To increase platelet count in dengue fever |
| Tamaris orientalis (Takaout el badia) | Can lead to rhabdomyolysis and AKI | Henna for hair dyeing |
| Hypericum perforatum (St. John’s Wort) | Induces cytochrome P 450 enzyme-drug interactions and AKI | Used for depression and menopausal symptoms |
| Propolis (Honey bees product) | Acute interstitial nephritis | Used as antiseptic/anti-inflammatory agent and hepatoprotective substance in South America |
| Carp (Fish gall bladder extract) | Can lead to watery diarrhea, jaundice, bradycardia, hypotension, oligoanuria and AKI | Used in folk therapies in parts of Asia |
| Caesalpinia decapetala (Cat’s Claw) | Acute interstitial nephritis | A herbal remedy used in Peru as Anti-inflammatory drug for rheumatism, systemic lupus erythematosus, cirrhosis |
| Cerbera thevetia (Yellow Oleander) | Renal tubular necrosis | Used as folk remedy for heart conditions, asthma, epilepsy, cancer and painful menstrual periods |
| Cupressus funebris (Mourning Cypress) | Acute tubular necrosis, interstitial nephritis, and hemoglobin casts | Used as herbal remedy for bleeding piles and painful menstrual cycles |
|
Securidaca longepedunculata (Wild Wisteria) |
Contains salicylates-can cause ischemic renal damage/cortical necrosis and acute interstitial nephritis | Used as folk remedy for dysmenorrhea and venereal diseases |
|
Euphorbia paralias (Spurge) |
Tubular necrosis | Used as traditional medicine as an anti-inflammatory agent, a purgative and for its local anesthetic property. |
| Crotalaria laburnifolia (Bird flower) | Acute tubular injury | Used as Dysmenorrhea and Abortifacient |
| Obstructive AKI | ||
| Archidendron pauciflorum (Djenkol beans) |
Djenkolism- spasmodic suprapubic and/or flank pain, urinary obstruction and acute kidney injury |
Local delicacy in Southeast Asia |
| Sobi-Lobi (Datura) | Contains anticholinergic substances-urinary obstruction and AKI | Consumed for its hallucinogenic properties |
| Salix daphnoides (Willow bark) | The bark contains salicin, which is metabolized in the body to salicylate-Renal papillary necrosis | Used for pain/headache and inflammatory conditions in China and Europe |
| Chronic kidney disease | ||
| Aristolochia clematitis (Birthwort) | Chronic interstitial nephritis, renal tubular defects, urothelial malignancies | Treatment of Gastrointestinal colic, slimming regimen |
| Irvingia gabonensis (African Mango) | CKD-unknown mechanism | Used for weight reduction, diarrhea, dysentery |
| Lorrea tridentata (Chaparral) | Renal cystic disease-CKD | Herbal supplement marketed to treat colds, skin disorders, arthritis, bladder infections and cancer |
| Ephedra sinica (Ma-Huang) | Nephrolithiasis | Used for asthma, weight loss, sexual enhancement, and euphoria |
| Averrhoa Carambola (Star fruit) | Oxalate nephropathy/Nephrolithiasis, obstructive nephropathy | Traditional remedy for diabetes mellitus in Asian countries |
|
Vaccinium macrocarpon (Cranberry) |
Oxalate nephropathy/Nephrolithiasis, obstructive nephropathy | Used for reducing the risk of urinary tract infections |
|
Pausinystalia yohimbe (Yohimbe) |
Lupus nephritis | Used for erectile dysfunction, athletic performance and weight loss |
|
Fucus vesiculosus (Bladder wrack) |
Contains heavy metals-Chronic interstitial nephritis | Traditional herb used to treat reflux and heartburn |
| Rhizoma Rhei (Rhubarb) | Chronic interstitial nephritis | Traditional Chinese medication used to treat constipation/cold sores |
|
Echinacea spp. (Coneflower) |
Renal tubular acidosis | Herbal remedy for common cold, cough, bronchitis and upper respiratory infections |
AKI: Acute kidney injury, CKD: Chronic kidney disease, ARF: Acute renal failure
Challenges in diagnosis of kidney disease due to traditional medicines
The prevalence of CKD has significantly increased in India over the past two decades. In a recent cross-sectional study from India, almost two-thirds of CKD patients were on some form of alternative medicine, in which Ayurveda was the most common.72 Many individuals have a strong cultural or religious belief in the efficacy and safety of traditional medicines making them reluctant to disclose their use to healthcare providers. The clinicians mustactively seek information from their patients about the use of traditional/herbal drug remedies. Undocumented traditional medicine ingestion should always be considered when investigating a patient with unexplained kidney disease. There is ample evidence to suggest that traditional medicines that were once considered natural and nontoxic contain some unknown toxic ingredients that might cause renal injury.73,74 Public enlightenment is of utmost importance to educate the general population about the dangers posed by herbal remedies. Enforcing stringent regulations on the production and sale of traditional medicines can ensure better quality and safety standards.
As the popularity of herbal and traditional medicines continues to rise, the risks associated with their use cannot be overlooked. The concurrent use of traditional and modern medicines further complicates the landscape, posing challenges for diagnosis and treatment. Addressing this issue needs a multifaceted approach that includes enhancing public awareness about the potential risks, imposing strict regulatory frameworks, promoting better communication between patient and healthcare provider, and accessible/affordable healthcare services.
Conflicts of interest
There are no conflicts of interest.
References
- Natural medicines causing acute kidney injury. Semin Nephrol. 2008;28:416-28.
- [CrossRef] [PubMed] [Google Scholar]
- Acute kidney injury associated with the use of traditional medicines. Nat Clin Pract Nephrol. 2008;4:664-71.
- [CrossRef] [PubMed] [Google Scholar]
- Herbal medicines and chronic kidney disease. Nephrology (Carlton). 2010;15(Suppl 2):10-7.
- [CrossRef] [PubMed] [Google Scholar]
- ”WHO Establishes the Global Centre for Traditional Medicine in India.” allAfrica.com, 25 Mar 2022, Gale Academic OneFile.
- Mainstreaming of Ayurveda, Yoga, Naturopathy, Unani, Siddha, and Homeopathy with the health care delivery system in India. J Tradit Complement Med. 2015;5:116-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Herbal therapy is associated with the risk of CKD in adults not using analgesics in Taiwan. Am J Kidney Dis. 2007;49:626-33.
- [CrossRef] [PubMed] [Google Scholar]
- Traditional medicine practices among community members with chronic kidney disease in northern Tanzania: An ethnomedical survey. BMC Nephrol. 2015;16:170.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Balkan nephropathy: Evolution of our knowledge. Am J Kidney Dis. 2008;52:606-16.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mercury-associated nephrotic syndrome: A case report and systematic review of the literature. Am J Kidney Dis. 2013;62:135-8.
- [CrossRef] [PubMed] [Google Scholar]
- Noni juice (Morinda citrifolia): Hidden potential for hyperkalemia? Am J Kidney Dis. 2000;35:310-2.
- [CrossRef] [PubMed] [Google Scholar]
- A hidden cause of hypokalemic paralysis in a patient with prostate cancer. Support Care Cancer. 2004;12:810-2.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cesium-associated hypokalemia successfully treated with amiloride. Clin Kidney J. 2015;8:335-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- [A case of severe hypokalemia caused by a Chinese herbal remedy (Yokukansan) in an 81-year-old woman with dementia] Nihon Ronen Igakkai Zasshi. 2011;48:553-7.
- [CrossRef] [PubMed] [Google Scholar]
- Severe rhabdomyolysis following massive ingestion of oolong tea: Caffeine intoxication with coexisting hyponatremia. Vet Hum Toxicol. 1999;41:381-3.
- [PubMed] [Google Scholar]
- Symptomatic hyponatremia following Bowel preparation for Colonoscopy: A Case Report. J Nepal Med Assoc. 2020;58:938-40.
- [CrossRef] [Google Scholar]
- Reversible Fanconi syndrome after ingestion of a Chinese herbal ‘remedy’ containing aristolochic acid. Nephrol Dial Transplant. 2001;16:400-2.
- [CrossRef] [PubMed] [Google Scholar]
- An unusual cause of hypokalemic paralysis: Aristolochic acid nephropathy with Fanconi syndrome. Am J Med Sci. 2005;330:153-5.
- [CrossRef] [PubMed] [Google Scholar]
- Rhabdomyolysis in response to weight-loss herbal medicine. Am J Med Sci. 2004;327:356-7.
- [CrossRef] [PubMed] [Google Scholar]
- Rhabdomyolysis in an unsuspecting patient. J Community Hosp Intern Med Perspect. 2018;8:386-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Acute renal failure following the use of herbal remedies. East Afr Med J. 1991;68:993-8.
- [PubMed] [Google Scholar]
- Nephropathy associated with animal, plant, and chemical toxins in the tropics. Semin Nephrol. 2003;23:49-65.
- [CrossRef] [PubMed] [Google Scholar]
- Acute renal failure associated with the use of traditional folk remedies in South Africa. Ren Fail. 2005;27:35-43.
- [CrossRef] [PubMed] [Google Scholar]
- The “green water” syndrome: Copper-induced hemolysis and subsequent acute renal failure as consequence of a religious ritual. Am J Med. 1995;98:311-5.
- [CrossRef] [PubMed] [Google Scholar]
- A case of podophyllum poisoning with involvement of the nervous system. Br Med J. 1957;2:1155-7.
- [CrossRef] [PubMed] [Google Scholar]
- Adulteration of Chinese herbal medicines with synthetic drugs: A systematic review. J Intern Med. 2002;252:107-13.
- [CrossRef] [PubMed] [Google Scholar]
- Screening methods for drugs and heavy metals in Chinese patent medicines. Bull Environ Contam Toxicol. 2000;65:112-9.
- [CrossRef] [PubMed] [Google Scholar]
- Medicinal herbs: A potential source of toxic metal exposure for man and animals in India. Arch Environ Health. 2002;57:229-31.
- [CrossRef] [PubMed] [Google Scholar]
- [Rhabdomyolysis due to paraphenylenediamine (hair dye)—report of an autopsy case] Nihon Hoigaku Zasshi. 1990;44:469-74.
- [PubMed] [Google Scholar]
- Takaout induced acute renal failure. Semin uro nephrol pitie salpetriere. 2002;28:140-3.
- [Google Scholar]
- Alterations in cyclosporin A pharmacokinetics and metabolism during treatment with St John’s wort in renal transplant patients. Br J Clin Pharmacol. 2003;55:203-11.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Nephrotoxicity of herbal products in Europe—A review of an underestimated problem. Int J Mol Sci. 2021;22:4132.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Herbal remedy-associated acute renal failure secondary to Cape aloes. Am J Kidney Dis. 2002;39:E13.
- [CrossRef] [PubMed] [Google Scholar]
- Global hazards of herbal remedies: Lessons from Aristolochia: The lesson from the health hazards of Aristolochia should lead to more research into the safety and efficacy of medicinal plants. EMBO Rep. 2016;17:619-25.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Acute kidney injury in the tropics. Ann Saudi Med. 2011;31:451-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Chemistry, pharmacology, and toxicology of khat (catha edulis forsk): A review. Addict Health. 2011;3:137-49.
- [PubMed] [PubMed Central] [Google Scholar]
- Case report: Fatal poisoning with colchicum autumnale. Crit Care. 2004;8:R56-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Acute renal failure following hypokalemic rhabdomyolysis due to chronic glycyrrhizic acid administration. Intern Med. 1992;31:708-11.
- [CrossRef] [PubMed] [Google Scholar]
- Severe but reversible acute kidney injury resulting from Amanita punctata poisoning. Kidney Res Clin Pract. 2015;34:233-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Acute kidney injury, oral mucositis and gastritis as complications of ingestion of papaya leaf juice extract in a patient presenting with dengue fever. J Clin Sci Res. 2019;8:204-6.
- [CrossRef] [Google Scholar]
- Acute renal failure induced by a Brazilian variety of propolis. Am J Kidney Dis. 2005;46:e125-9.
- [CrossRef] [PubMed] [Google Scholar]
- Acute renal failure due to ingestion of the gallbladder of grass carp. Clin Nephrol. 1992;37:104-5.
- [PubMed] [Google Scholar]
- Hepatic and renal toxicity among patients ingesting sheep bile as an unconventional remedy for diabetes mellitus—Saudi Arabia, 1995. MMWR Morb Mortal Wkly Rep. 1996;45:941-3.
- [PubMed] [Google Scholar]
- Nephron obstruction in nordihydroguaiaretic acid-induced renal cystic disease. Kidney Int. 1979;15:7-19.
- [CrossRef] [PubMed] [Google Scholar]
- Cystic renal cell carcinoma and acquired renal cystic disease associated with consumption of chaparral tea: A case report. J Urol. 1994;152:2089-91.
- [CrossRef] [PubMed] [Google Scholar]
- Hypokalemic nephropathy. Kidney Int Rep. 2018;3:1482-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Yohimbine-induced cutaneous drug eruption, progressive renal failure, and lupus-like syndrome. Urology. 1993;41:343-5.
- [CrossRef] [PubMed] [Google Scholar]
- Fucus vesiculosus: A nephrotoxic alga? Nephrol Dial Transplant. 1998;13:526-7.
- [CrossRef] [PubMed] [Google Scholar]
- Acute renal failure associated with prolonged intake of slimming pills containing anthraquinones. Hong Kong Med J. 2006;12:394-7.
- [PubMed] [Google Scholar]
- Beethoven’s renal disease based on his autopsy: A case of papillary necrosis. Am J Kidney Dis. 1993;21:643-52.
- [CrossRef] [PubMed] [Google Scholar]
- Traditional medications mixed with ethylene glycol in a Nigerian patient on hemodialysis. Cureus. 2020;12:e6950.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Chronic renal failure in North Central province of Sri Lanka: An environmentally induced disease. Trans R Soc Trop Med Hyg. 2007;101:1013-7.
- [CrossRef] [PubMed] [Google Scholar]
- Uddanam nephropathy in India: A challenge for epidemiologists. Bull World Health Organ. 2017;95:848-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Rising of a global silent killer: Critical analysis of chronic kidney disease of uncertain aetiology (CKDu) worldwide and mitigation steps. Environ Geochem Health. 2023;45:2647-62.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Traditional indigenous medicines are an etiologic consideration for NELL1-positive membranous nephropathy. Kidney Int. 2022;102:1424-6.
- [CrossRef] [PubMed] [Google Scholar]
- Membranous nephropathy associated with indigenous Indian medications containing heavy metals. Kidney Int Rep. 2020;5:1510-4.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The heavy metal contents of some selected medicinal plants sampled from different geographical locations. Pharmacognosy Res. 2013;5:103-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Herbal medication triggering lupus nephritis – a case report. BMC Complement Med Ther. 2020;20:163.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Djenkol beans as a cause of hematuria in children. Nephron. 1997;76:39-42.
- [CrossRef] [PubMed] [Google Scholar]
- Djenkol bean as a cause of urolithiasis. Southeast Asian J Trop Med Public Health. 1978;9:427-32.
- [PubMed] [Google Scholar]
- Djenkol bean, djenkolic acid and djenkolism. J Med Assoc Thai. 1979;62:530-1.
- [PubMed] [Google Scholar]
- Mechanisms of star fruit-induced acute renal failure. Food Chem Toxicol. 2008;46:1744-52.
- [CrossRef] [PubMed] [Google Scholar]
- Ephedrine nephrolithiasis associated with chronic ephedrine abuse. J Urol. 1998;160:825.
- [CrossRef] [PubMed] [Google Scholar]
- Ma-huang strikes again: Ephedrine nephrolithiasis. Am J Kidney Dis. 1998;32:153-9.
- [CrossRef] [PubMed] [Google Scholar]
- Dietary supplementation with cranberry concentrate tablets may increase the risk of nephrolithiasis. Urology. 2001;57:26-9.
- [CrossRef] [PubMed] [Google Scholar]
- Prescription profile of potentially aristolochic acid containing Chinese herbal products: An analysis of National Health Insurance data in Taiwan between 1997 and 2003. Chin Med. 2008;3:13.
- [CrossRef] [PubMed] [Google Scholar]
- Endemic nephropathy: The case for chronic poisoning by aristolochia. Croat Med J. 2005;46:116-25.
- [PubMed] [Google Scholar]
- Complexities of the herbal nomenclature system in traditional Chinese medicine (TCM): Lessons learned from the misuse of Aristolochia-related species and the importance of the pharmaceutical name during botanical drug product development. Phytomedicine. 2007;14:273-9.
- [CrossRef] [PubMed] [Google Scholar]
- Increased risk of urinary tract cancer in ESRD patients associated with usage of Chinese herbal products suspected of containing aristolochic acid. PLoS One. 2014;9:e105218.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Invasive urothelial carcinoma after exposure to Chinese herbal medicine containing aristolochic acid may occur without severe renal failure. Nephrol Dial Transplant. 2003;18:426-8.
- [CrossRef] [PubMed] [Google Scholar]
- Reduction in the incidence of urological cancers after the ban on Chinese herbal products containing aristolochic acid: An interrupted time-series analysis. Sci Rep. 2019;9:19860.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence of use of complementary and alternative medicine in chronic kidney disease: A cross-sectional single-center study from South India. Saudi J Kidney Dis Transpl. 2019;30:185-93.
- [CrossRef] [PubMed] [Google Scholar]
- Nephrotoxicity and Chinese herbal medicine. Clin J Am Soc Nephrol. 2018;13:1605-11.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Nephrotoxicity of herbal medicine and its prevention. Front Pharmacol. 2020;11:569551.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]








