Translate this page into:
NELL-1 Associated Membranous Nephropathy - A Case Series from India
Corresponding author: Vaibhav Tiwari, Department of Nephrology, Sir Ganga Ram Hospital, New Delhi, India. E-mail: drvt87@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sharma Y, Jain A, Gupta P, Tiwari V, Gupta A, Bhargava V, et al. NELL-1 Associated Membranous Nephropathy - A Case Series from India. Indian J Nephrol. doi: 10.25259/ijn_326_23
Abstract
Neural epidermal growth factor-like 1 (NELL-1) is responsible for a substantial proportion of cases of PLA2R-negative primary membranous nephropathy (MN). To investigate the occurrence, association, and treatment responses, we carried out this ambispective study. In the study, nine (10%) of all patients with MN at our center were found to be NELL-1 positive. On follow up, all patients recieved immunosuppression (steroids, cyclophosphamide or rituximab). Five patients were in complete remission, while one patient had partial remission, two patients had a progressive decline in kidney function, and one patient was lost to follow-up early. No link was found with malignancies, traditional Indian medicines or infection.
Keywords
NELL-1
Membranous nephropathy
nephrotic syndrome
MN
glomerulonephritis
Introduction
Neural epidermal growth factor-like 1 (NELL-1) is the antigen responsible for approximately 16% of cases of PLA2R-negative primary membranous nephropathy (MN).1 Research on the role of this antibody concerning its correlation with other diseases, particularly cancers, its reaction to immunosuppressive therapy, and its impact on kidney health is still in the early stages. To investigate the occurrence, characteristics, associations, and treatment responses, we examined prospective data up to September 2022 and retrospective data from January 2018 to March 2021 on all histologically confirmed MN. We employed immunohistochemistry to apply specific antibodies to detect the NELL-1 antigen in renal tissue.
Case Series
Over a period of 5 years, of the 90 patients with MN seen at our center, nine (10%) patients were detected with NELL-1 MN. Out of nine patients, six were males and three were females. The median age was 39 years [Table 1]. The baseline median urine protein creatinine ratio (UPCR) was 4.71 g/g (range: 1.02-10.71), median serum albumin was 2.95 g/dL, and creatinine levels varied between 0.61 and 9.39 mg/dL, with the median value recorded at 1.26 mg/dL. Out of nine patients, one had MN secondary to lupus nephritis. None of our patients had been identified with any malignancy or had taken indigenous medicines. One patient was dual positive for PLA2R and NELL-1 antigen. On histopathology, all patients had thickening of glomerular capillary basement membrane with argyrophilic epimembranous spikes in five of the nine cases. No segmental sclerosis was seen in any of the cases. IgG was the most consistent immunoglobulin on immunofluorescence [Table 2]. IgG deposit was diffuse and granular in all cases along the glomerular capillary basement membrane [Figure 1]. NELL-1 staining pattern was also diffuse, and granular deposits were noted along the glomerular capillary basement membrane [Figure 2]. The follow-up period was 1-42 months (median: 13 months). At the end of the study, five patients were in complete remission (UPCR <300 mg/g), while one patient had partial remission (UPCR >300 mg but >50% reduction from the baseline), two patients had a progressive decline in kidney function (>50% increase in the creatinine from the baseline), and one patient was lost to follow-up early.
| Age | Baseline (UPCR g/g) | Baseline albumin (g/dL) | Baseline creatinine (mg/dL) | Treatment | Follow up duration (months) | Follow up UPCR (g/g) | Albumin (g/dL) | Creatinine (mg/dL) | Outcome |
|---|---|---|---|---|---|---|---|---|---|
| 52 | 2.1 | 1.71 | 1.26 | MMF + Steroids | 17 | 1.1 | 2.44 | 2.2 | KD |
| 59 | 5.6 | 2.66 | 0.95 | Rituximab | 42 | 0.06 | 4.56 | 0.84 | CR |
| 53 | 10.71 | 1.71 | 1.27 | Cyclophosphamide + Steroids | 36 | 7.05 | 2.44 | 1.97 | KD |
| 26 | 2.1 | 3.6 | 1.46 | Rituximab | 13 | 0.58 | 3.67 | 1.53 | PR |
| 53 | 1.02 | 1.89 | 1.33 | Steroids | 1 | 1.029 | 1.37 | 2.92 | Loss to follow-up |
| 33 | 6.7 | 3.2 | 9.39 | Steroids | 4 | 0.06 | 4.2 | 0.68 | CR |
| 34 | 4.71 | 3.5 | 0.61 | Rituximab | 13 | 0.24 | 4.0 | 0.50 | CR |
| 35 | 3.2 | 3.2 | 0.78 | Rituximab | 9 | 0.07 | 4.49 | 0.9 | CR |
| 39 | 7.39 | 2.95 | 0.74 | Rituximab | 15 | 0.21 | 3.5 | 1.32 | CR |
MMF: Mycophenolate Mofetil, UPCR: urine protein creatinine ratio, KD: Progressive kidney decline, CR: complete remission, PR: partial remission. NELL-1: Neural epidermal growth factor-like 1
| Light microscopy | IgG | IgM | IgA | C1Q |
|---|---|---|---|---|
| Membranous nephropathy with acute interstitial nephritis, Lupus nephritis (ISN/RPS class V). | 3+ | 1+ | – | 3+ |
| Membranous nephropathy | 2+ | – | – | – |
| Membranous nephropathy | 3+ | – | – | – |
| Membranous nephropathy | – | – | – | – |
| Early Membranous nephropathy with acute interstitial nephritis. | 3+ | 1+ | – | 1+ |
| Membranous nephropathy with acute interstitial nephritis. | 3+ | 2+ | – | – |
| Membranous nephropathy | 3+ | – | – | – |
| Membranous nephropathy | 3+ | – | – | – |
| Membranous nephropathy | 3+ | – | – | – |
IgG: Immunoglobin G, IgM: Immunoglobulin M, Ig A: Immunoglobulin A, C1Q: Complement component 1q, ISN/RPS: Indian Society of Nephrology/Renal Pathology Society, NELL: Neural epidermal growth factor
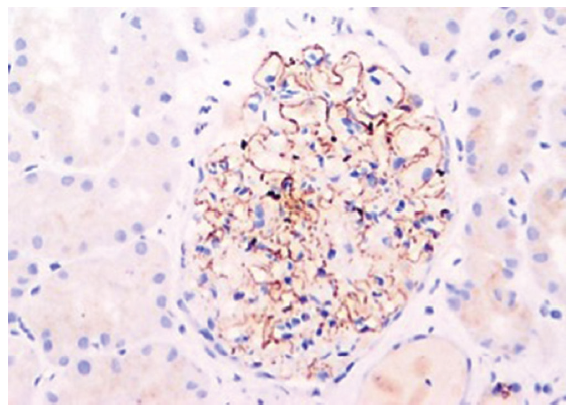
- NELL-1 antigen demonstration by immunohistochemistry (Original magnification x200). NELL-1: Neural epidermal growth factor-like 1
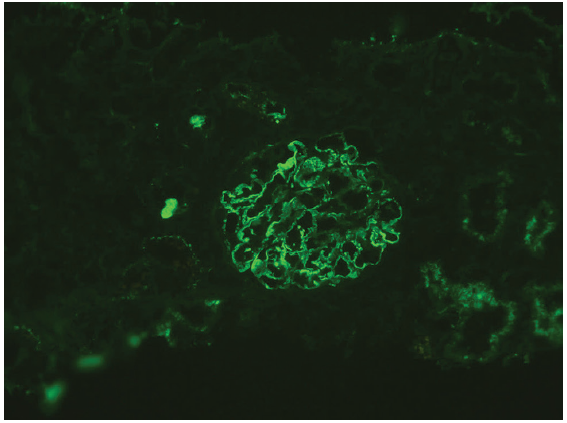
- NELL-1 staining on immunofluorescence (Original magnification x200). NELL-1: Neural epidermal growth factor-like 1
Discussion
NELL-1 encodes a protein kinase C-binding protein, which is expressed in the kidney tubules and rarely in the glomeruli.2 It can also be expressed in malignancy-associated secondary MN patients.
In Sethi et al. study, 29 NELL-1-associated MN cases had a mean age of 63 years, while Caza T et al. larger study had 91 cases with a mean age of 66.8 years and a male predominance.1,3 Our study differs, with a younger mean age of 42.66 years, potentially accounting for the lower malignancy rates. The significance of the link between NELL-1 and various diseases needs further study. Sethi et al. reported associations with cancers and autoimmune conditions, but our patient with NELL-1 and lupus nephritis had no such history, suggesting unique profiles in our cohort.4
Concurrent AIN with MN is rare, with only one case among 594 patients in Chen T et al.’s study.5 However, we found three NELL-1 MN cases with AIN, none related to known triggers. Prior research has not delineated an increased incidence of AIN in MN. Consequently, further investigations are imperative to ascertain whether the observed correlation is incidental or indicative of a causative linkage.
In our study, five out of nine patients were treated with rituximab. Four of these patients achieved complete remission, while one saw partial improvement. In contrast, a patient on cyclophosphamide and steroids did not improve. Patients with AIN treated only with steroids had varied outcomes: one reached complete remission, while another was lost to follow-up. Supporting these findings, a Chinese study with 15 NELL-1 MN patients observed 92% remission with immunosuppressive therapy (steroids + cyclophosphamide or cyclosporine) over 25 ± 21 months.6 In addition, a Japanese study found similar success in remission with immunosuppression (steroids or steroids + cyclophosphamide).7 This collective evidence suggests that immunosuppression is generally effective against NELL-1-associated MN.
One patient of MN was dual positive for PLA2R and NELL-1 antigen. Till now, only a single case has been reported in the literature.8 The significance of dual positivity on presentation or course is yet to be determined.
Conclusion
Notably, we found no links with malignancies, traditional Indian medicines, or infections. It remains uncertain whether these findings are serendipitous or attributable to distinct environmental and genetic factors inherent to the Indian population. To clarify the correlation of NELL-1-associated MN with these elements within the Indian demographic, an expansion to larger patient cohorts is necessary.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
References
- Neural epidermal growth factor-like 1 protein (NELL-1) associated membranous nephropathy. Kidney Int. 2020;97:163-74.
- [CrossRef] [PubMed] [Google Scholar]
- Cloning and characterization of two novel human cDNAs (NELL1 and NELL2) encoding proteins with six EGF-like repeats. Genomics. 1996;38:273-6.
- [CrossRef] [PubMed] [Google Scholar]
- NELL1 is a target antigen in malignancy-associated membranous nephropathy. Kidney Int. 2020;99:P967-76.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The many faces of NELL1 MN. Clin Kidney J. 2023;16:442-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Acute kidney injury in idiopathic membranous nephropathy with nephrotic syndrome. Ren Fail. 2021;43:1004-11.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Neural epidermal growth factor–like 1 protein–positive membranous nephropathy in chinese patients. Clin J Am Soc Nephrol. 2021;16:727-35.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence of neural epidermal growth factor-like 1- and exostosin 1/exostosin 2-associated membranous nephropathy: A single-center retrospective study in Japan. Sci Rep. 2022;12:2967.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Neural epidermal growth factor-like 1 protein-positive membranous nephropathy in Chinese patients. Clin J Am Soc Nephrol. 2021;16:727-35.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







