Translate this page into:
Percutaneous Transhepatic Vein Permcath: A Case Report
Address for correspondence: Dr. Prashant B. Malviya, Department of Nephrology, Apollo Hospital, Jubillee Hills, Hyderabad - 500 096, Telangana, India. E-mail: prashant_malviya37@yahoo.co.in
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
In patients with end-stage renal disease (ESRD), functional vascular access is like a lifeline. Among the patients undergoing hemodialysis, arteriovenous fistulas are done in most of them. However, in approximately 15% of these patients with multiple access failures, the use of tunneled dialysis catheters (TDC) for hemodialysis has become an integral component of treatment plans. Unfortunately, in many cases of multiple access failure, it is difficult to get proper access especially if problems with peritoneal dialysis also exist. The problems related to tunneled dialysis catheters are infections, thrombosis, hemorrhage, migration, dislodgement, leakage, kinking, and chronic venous stenosis. The progressive loss of venous access sites requires a systematic approach to alternative sites as it is important for patient survival. Herein, we present a case of ESRD with multiple access failures who was effectively managed with the placement of a percutaneous transhepatic vein permcath. Till date, there is very little data onsuch interventions from India.
Keywords
Complications
end-stage renal disease
permcath
transhepatic vein
tunneled dialysis catheters
vascular access
Introduction
Chronic kidney disease (CKD) is a major public health concern worldwide and also in India. The overall prevalence of CKD in India is around 10% with the most common cause of being diabetes.[12] In developed countries, hemodialysis (HD) is the mainstay of renal replacement therapy (RRT). In India, there are over 130,000 patients receiving dialysis, and the number requiring dialysis is increasing by about 232 per million population.[1] Given the increase in dialysis requirement, underlying comorbidities, and age more patients fall prey to problems like multiple vascular access failure. In the present study, we report a case of one such patient who had multiple vascular access failures coupled with peritoneal dialysis failure who underwent a transhepatic vein tunneled dialysis catheter (TDC) placement which is quite rare in the Indian scenario.
Case
A 31-year-old female had a severe post partum hemorrhage in her second pregnancy in April 2019 requiring transfusion of 8–10 units of blood. During her pregnancy, she had regular follow-ups to her obstetrician once a month and had normal blood pressure recordings throughout pregnancy. Post-delivery, her renal function deteriorated from a pre-pregnancy serum creatinine value of 0.9 mg/dL to 11.9 mg/dL with in 5 days. She was initiated on hemodialysis, initially through the right femoral vein followed by the right internal jugular vein. After 1 month, she underwent a renal biopsy which showed patchy cortical necrosis with 50% interstitial fibrosis and tubular atrophy (IFTA). Her renal functions never recovered and she was kept on maintenance hemodialysis. A left radio cephalic AV fistula was attempted but she had a primary fistula failure after which she underwent a tunneled dialysis catheter (TDC) placement in the right internal jugular vein (IJV). She had a series of access failures from right IJV to left IJV TDC, followed by right femoral, left femoral TDC, and a subclavian non-tunneled dialysis catheter. Peritoneal dialysis was attempted but she had poor outflow; redo peritoneal dialysis had similar results. Contrast-enhanced computed tomography (CECT) scan showed thrombosis in both internal jugular veins, both femoral veins, subclavian, and infrarenal inferior vena cava. Her thrombophilia workup showed normal homocysteine, protein C and S normal, and antithrombin 3 antibody negative. ANA profile and APLA workup were also negative.
In view of multiple vascular access failures and PD failure, infrarenal IVC thrombosis she underwent percutaneous transhepatic vein TDC placement. Under ultrasound guidance and local anesthesia, the Chiba needle was introduced in a hepatic vein via a percutaneous route through which guide wire was passed. Serial dilatation was done and access was secured with peel-away sheath. Palindrome catheter 14.5 F × 19 cm was secured under fluoroscopic guidance and tunneled for 5 cm. It was positioned with a catheter tip at inferior vena cava (IVC) – right atria junction [Figures 1 and 2]. Presently, she is on dialysis for 2 months, her uremic symptoms subsided, and the condition has improved [Figure 3]. The permcath is fully functional and yielding blood flow rates of 300–350 mL/min

- Hepatic vein permcath placement under fluoroscopy guidance

- X-ray showing tip of hepatic vein permcath in IVC
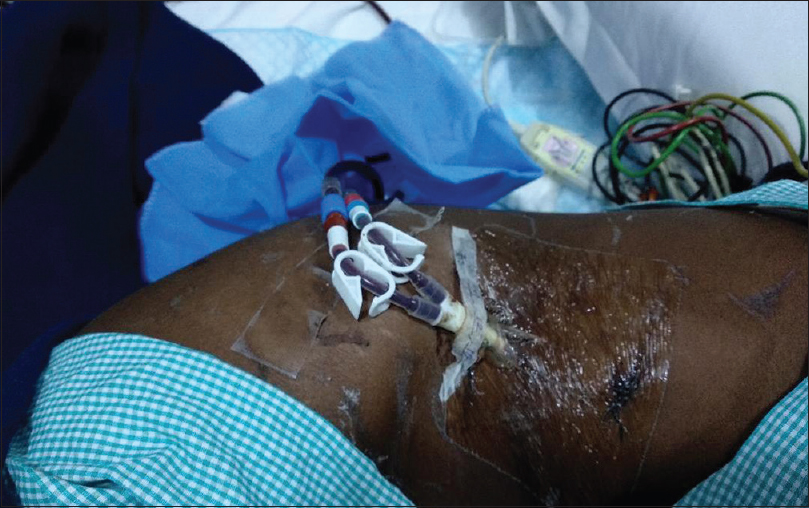
- Patient showing entry point of hepatic vein permcath
Discussion
There are three major types of vascular access: arteriovenous fistula (AVF), arteriovenous graft (AVG), and tunneled dialysis catheters (TDCs). In their article, Pereira et al. described a systemic approach and clinical practice algorithm for various access options for tunneled dialysis catheters [Table 1].[3]
| Conventional | Unconventional |
|---|---|
| Internal jugular vein (right/left) | External jugular vein |
| Femoral vein (right/left) | Translumbar inferior vena cava |
| Subclavian vein (right/left) | Hepatic vein |
The most commonly used sites of placement of TDC, in order of preference, are right internal jugular vein, left internal jugular vein, external jugular veins, and femoral veins. Rahman and Kuban elaborated unconventional routes of placement of dialysis catheters in patients who had occlusions of conventional veins including placing them through translumbar, transhepatic, and transrenal route.[4] The TDC placement via the translumbar approach into the inferior vena cava (IVC) is reliable as due to the large radius of the vein, thrombosis is rare.[5] In this patient, this approach was not used as she had a chronic thrombosis of the infra diaphragmatic portion of the IVC.
Po et al. first described the transhepatic approach when they reported a similar patient who had failed peritoneal dialysis and difficult vascular access requiring transhepatic vascular access which lasted for over 1 year.[6] Immediate complications associated with transhepatic vascular access include perihepatic hematoma and hepatic arterial injury, and long-term complications include catheter dislodgement/migration, catheter-related sepsis, and catheter thrombosis. Hepatic vein TDCs can result in liver hemorrhage in about 29% of the cases.[7] The relatively small size of the hepatic vein as compared to the IJ veins and IVC predisposes to thrombosis and stenosis of these veins. Kumar et al. presented a case report from Abu Dhabi in which patient who was undergoing long-term hemodialysis with hepatic vein permcath developed hepatic vein stenosis requiring balloon dilatation.[8] Catheter migration and displacement is commoner in the transhepatic approach as compared to the translumbar approach due to short distance between the right atrium, IVC and hepatic vein.[9] Coughing and abdominal distension also lead to catheter migration.[10]
Patency rate in the transhepatic approach in various studies has been reported from 24 days to 90 days. Stavropoulos et al. studied 36 transhepatic catheters and reported primary patency of just 24.3 days, the major reason being a high rate of late thrombosis.[11] Younes et al., in a study of 127 transhepatic catheters, reported much higher patency of 87.7 days.[12] When compared to the translumbar route, the transhepatic approach has a few advantages; there is less risk of bleeding and damage to surrounding structures. If bleeding occurs, it can easily be controlled by embolization. The transhepatic approach is easier in obese patients and can be performed even when the lower portion of the IVC is occluded.[13] Finally, translumbar TDC revisions are much more difficult than transhepatic TDCs due to retroperitoneal fibrosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conclusion
Transhepatictunneled dialysis catheter provides potentially viable access for a patient with exhausted access options. They possibly hold a slight edge over translumbar tunneled dialysis catheters.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Chronic kidney disease in India: A clarion call for change. Clin J Am Soc Nephrol. 2018;13:802-4.
- [Google Scholar]
- What do we know about chronic kidney disease in India:First report of the Indian CKD registry. BMC Nephrol. 2012;13:10.
- [Google Scholar]
- Vascular access for placement of tunneled dialysis catheters for hemodialysis: A systematic approach and clinical practice algorithm. J Clin Imaging Sci. 2015;5:31.
- [Google Scholar]
- Dialysis catheter placement in patients with exhausted access. Tech Vasc Interv Radiol. 2017;20:65-74.
- [Google Scholar]
- Difficult vascular access in a patient on chronic hemodialysis. Indian J Nephrol. 2019;28:2018-20.
- [Google Scholar]
- Analysis of early failure of tunneled hemodialysis catheters. AJR Am J Roentgenol. 2002;179:357-63.
- [Google Scholar]
- Central venous access: A primer for the diagnostic radiologist. AJR Am J Roentgenol. 2002;179:309-18.
- [Google Scholar]
- Percutaneous transhepatic venous access for hemodialysis. J Vasc Interv Radiol. 2003;14(9 Pt 1):1187-90.
- [Google Scholar]
- Transhepatic hemodialysis catheters: Functional outcome and comparison between early and late failure. J VascInterv Radiol. 2011;22:183-91.
- [Google Scholar]
- Percutaneous translumbar and transhepatic inferior vena caval catheters for prolonged vascular access in children. J Pediatr Surg. 1992;27:165-9.
- [Google Scholar]







