Translate this page into:
Perioperative Acute Myocardial Infarction in the First Deceased Kidney Transplantation Done in Bihar
Address for correspondence: Dr. Prit P. Singh, Department of Nephrology, Indira Gandhi Institute of Medical Sciences, Patna - 800 014, Bihar, India. E-mail: drprit@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor,
Patients with chronic kidney disease (CKD) are more likely to die from cardiac events than to develop end-stage Kidney disease (ESKD), reflecting the burden of cardiovascular disease in this population.[1] Kidney transplant recipients (KTR) are at greater risk of cardiovascular events especially in the perioperative period.[2] Here, we describe the first deceased donor kidney transplantation done in Bihar (March 2020) that was complicated with acute myocardial infarction (AMI) in the perioperative period.
A 51-year-old man, ESKD patient on maintenance hemodialysis for 2 years and treated successfully for Hepatitis-B infection, underwent deceased kidney transplantation. Routine pre-transplant workup, including electrocardiogram (ECG) and coronary angiography, was normal while 2D echocardiography showed mild concentric left ventricular hypertrophy.
Two hours after transplant surgery, he developed progressive shortness of breath and oxygen saturation dipped to 88%. His urine output decreased to100 ml per hour and blood pressure to110/80 mm Hg. ECG showed new-onset left bundle branch block (LBBB) with junctional rhythm [Figure 1]; however, troponin-T was negative. Other differential diagnosis considered was ischemic ATN with volume overload but new-onset ECG changes were more in favor of cardiac etiology. 2D echocardiography showed anterior wall hypokinesia of left ventricle with LVEF––54%. Chest X-ray was suggestive of pulmonary edema. In the setting of acute left ventricular failure, decreasing urine output and metabolic acidosis, the patient was given one session of hemodialysis. Twelve hours later, evaluation revealed increased levels of Troponin-I 275.1 pg/ml (normal value <26.2 pg/mL), serum CK-MB 7.33 ng/mL (normal value <6.22 ng/mL), and BNP 948.8 pg/ml (normal value <32.8 pg/mL). He was started on dual antiplatelet therapy and unfractionated heparin with activated clotting time monitoring. The patient improved symptomatically. On day three, blood Troponin-I (50 pg/mL), CK-MB (1.82 ng/mL), and BNP levels (297.97 pg/mL) showed significant decline and urine output was 4 liters/day. Patient tolerated regimen well, did not develop any bleeding manifestation and his stool for occult blood examination also was negative (done fifth post-operative day). Ten days later, he developed wound dehiscence which was managed with secondary suturing. The patient was discharged with normal allograft function (serum creatinine––0.9 mg/dL) and adequate urine output. In the next 6 months follow-up (last follow-up done on October 30, 2020), he was doing well with normal graft function.
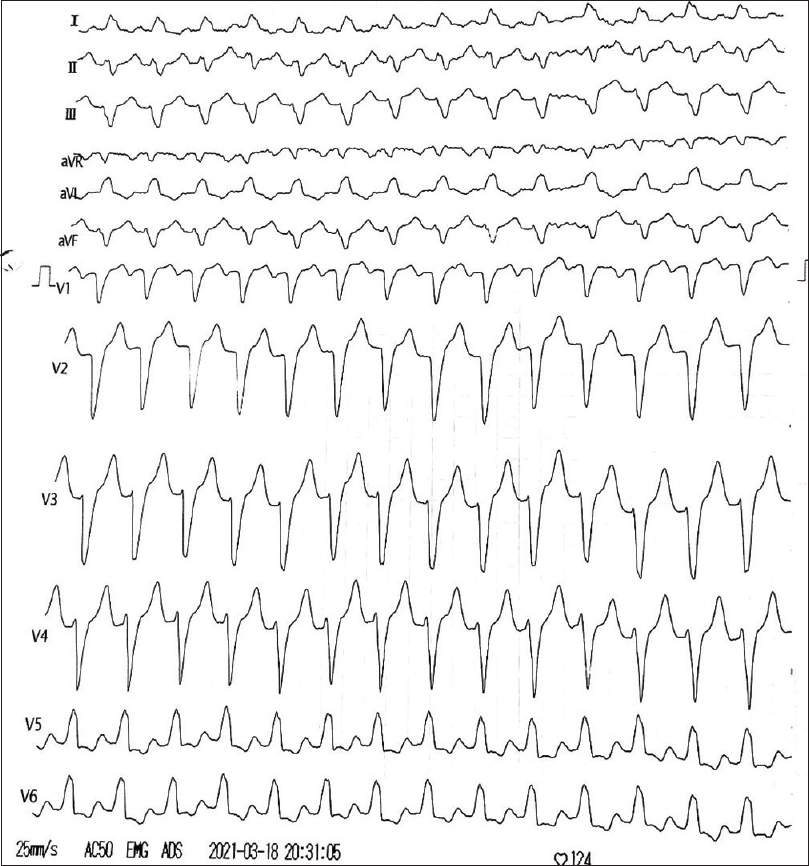
- ECG showing left bundle branch block
Kidney transplantation is associated with 17% risk reduction for myocardial infarction (MI) compared to patients in the waiting list. Risk of MI is highest during the perioperative period and its incidence decreases gradually after transplantation.[2] Perioperative myocardial infarction (MI) may occur despite having normal cardiac screening as seen in our patient. Non-cardiac surgery is associated with major cardiovascular complications and over 1 million patients are likely to have such a complication every year.[3] Devereaux et al. in their study showed that 65%–93% of patients with perioperative acute coronary syndrome (ACS) have no ischemic symptoms and 50% of cases of MI go unrecognized.[4] Moreover, only 14% of patients experience chest pain in MI leading to difficulty in diagnosis and failure of early treatment initiation leading to increased morbidity.[4]
The pathophysiology of perioperative MI is distinct from that of non-operative MI. Perioperative cardiac events might occur due to demand-mediated ischemia and/or plaque rupture. Mechanism include thromboembolic dynamic obstruction from atherosclerotic plaque rupture and imbalanced myocardial oxygen demand-to-supply in chronic CAD patients.[5] Perioperative MI is relatively more common for recipients of a deceased-donor kidney, compared with a living-donor kidney.[2] Our patient had ESKD due to chronic glomerulonephritis, which might have also increased the chances of AMI in the perioperative period despite having a normal pre transplant coronary angiogram.[1] Common findings of patients with AMI in the perioperative period are persistent hypotension, nausea, diaphoresis, and shortness of breath. Other findings include decreased oxygen saturation and ECG changes.
To conclude, high index of suspicion is required for diagnosing AMI in the perioperative period as ESKD patients may not have typical ischemic signs and symptoms. Optimal management of complications with good team effort leading to initial success helps in smoothly running a high stake program like deceased organ transplantation.
Declaration of patient's consent
The authors declare that appropriate consent was obtained from the patient for use of his clinical information and photographs. Patient understands that every effort will be taken to conceal his identity but anonymity can not be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We acknowledge the team spirit and support extended to us by Prof. P K Dube, Professor (Anaesthesiology), Dr Arvind Kumar, Additional professor, (Anaesthesiology); Dr Nirav Kumar, Additional Professor, Cardiology; and Dr Rohit Upadhyay Additional professor (Urology), IGIMS in managing the patient.
References
- Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296-305.
- [Google Scholar]
- Acute myocardial infarction and kidney transplantation. J Am Soc Nephrol. 2006;17:900-7.
- [Google Scholar]
- Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): A randomised controlled trial. Lancet. 2008;371:1839-47.
- [Google Scholar]
- Surveillance and prevention of major perioperative ischemic cardiac events in patients undergoing noncardiac surgery: A review. CMAJ. 2005;173:779-88.
- [Google Scholar]






