Translate this page into:
Pityriasis rubra pilaris and mesangial proliferative glomerulonephritis in a child: Association or coincidence?
Address for correspondence: Dr. S. Sarkar, Flat No. B/1, Jibantaru Apartment, North Jagtala, Maheshtala, Kolkata - 700 141, West Bengal, India. E-mail: sumantra.com@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Pityriasis rubra pilaris (PRP) is a group of uncommon, chronic dermatosis of juvenile or adult onset. It presents with scaling (pityriasis), reddish-orange patches (rubra), hyperkeratosis around hair follicle (pilus), and palmoplantar keratoderma. PRP may co-exist with various autoimmune disorders including dermatomyositis, vitiligo, and hypoparathyroidism.[123] Its association with the renal disorder is rare.
A 10-year-old boy presented with hematuria, oliguria, and anasarca for 4 weeks and few episodes of generalized tonic-clonic seizure for 2–3 days. There was no history of sore throat or skin infections prior to this illness. Other past medical history was noncontributory. His weight was 41 kg and height was 138 cm (50th percentile). His blood pressure was 126/80 mmHg. A few scaly, bilateral symmetrical, and nonitchy skin lesions were noted on elbows, knees, hands, and feet [Figure 1]. The investigation revealed 4+ urinary albumin and 18–20 red blood cells/hpf. The 24 h urine albumin was 2114 mg. His serum albumin was 1.8 g/dl and cholesterol was 302 mg/dl. Serum urea and creatinine were 39 mg/dl and 0.6 mg/dl, respectively. Antistreptolysin O titer on repeated occasion was low and C3 was 55.3 mg/dl (normal: 90–180 mg/dl), antinuclear factor was negative, partial thromboplastin, activated partial thromboplastin time was normal. Hepatitis B surface antigen, human immunodeficiency virus (HIV)-1, and HIV-2 were nonreactive. Ultrasonography whole abdomen revealed normal study. Electroencephalography revealed normal sleep records. Renal biopsy revealed an increase in mesangial cellularity and matrix along with fibrous crescents, patent capillary loops and no spikes or duplication in the basement membrane [Figure 2]. Biopsy from the skin lesion established the diagnosis of circumscribed juvenile type of PRP (type 4). His renal disease was treated with oral prednisolone and remission achieved after 2 weeks. The patient is on regular follow-up for last 2 years with no relapse of proteinuria until date. He is now under treatment of dermatologist for PRP.

- Typical skin lesions of circumscribed juvenile type of pityriasis rubra pilaris (type 4) on hands, knees, and feet
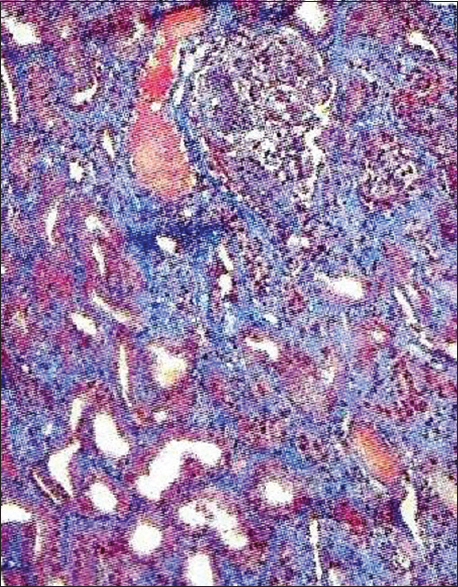
- Features of mesangial proliferative glomerulonephritis
PRP is an uncommon inflammatory and hyperproliferative dermatosis with no sex predilection. Both familial and acquired forms of PRP have been reported. It had a varied clinical progression and showed the varied rate of improvement with treatment. The etiology remains unknown. Emotional stress, microbial pathogens, trauma, Vitamin A deficiency, and light exposure may trigger PRP. Coexistence of PRP with other autoimmune disorders might be due to an abnormal immune response to antigenic triggers or microbial pathogens. Association of PRP with T-helper cell dysfunction has also been reported.[2] Association of renal disorders in case of PRP is extremely rare. An extensive search of literature could reveal only two case reports.[45] Both had membranous nephropathy. Mesangial proliferative glomerulonephritis co-existing with the specific subtype of circumscribed juvenile onset PRP (type 4) is hitherto unreported. It is not known whether there is underlying genetic cause for association of these two disorders or it is just a coincidence. Reporting of more such cases could stimulate future research to find out any association.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Dermatomyositis with a pityriasis rubra pilaris-like eruption: An uncommon cutaneous manifestation in dermatomyositis. Pediatr Dermatol. 2007;24:151-4.
- [Google Scholar]
- The clinical and histomorphological features of pityriasis rubra pilaris. A comparative analysis with psoriasis. J Cutan Pathol. 1997;24:416-24.
- [Google Scholar]
- Circumscribed juvenile-onset pityriasis rubra pilaris with hypoparathyroidism and brachyonychia. Cutis. 2006;77:218-22.
- [Google Scholar]
- A case of pityriasis rubra pilaris associated with membranous nephropathy. Australas J Dermatol. 2013;54:e1-3.
- [Google Scholar]
- A case of pityriasis rubra pilaris associated with rapidly progressive finger joint destruction. Nihon Rinsho Meneki Gakkai Kaishi. 2004;27:407-13.
- [Google Scholar]






