Translate this page into:
Post COVID Vaccination (COVAXIN™ -BB152 V) Pauci-immune Crescentic Glomerulonephritis
#Both authors contributed equally.
Address for correspondence: Dr. Abhyuday S. Rana, Department of Nephrology and Renal Transplant Medicine, Medanta -The Medicity, Sector 38, Gurguram - 122001, Haryana, India. E-mail: dr.abhirana@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Coronavirus disease 2019 (COVID-19) pandemic is responsible for widespread morbidity and mortality. The vaccination against the severe acute respiratory syndrome coronavirus 2 (SARS-COV-2) infection, the cause of the COVID-19 pandemic, is currently ongoing across the globe. Rapid vaccination is of paramount importance to mitigate this pandemic. Although considered safe in general, these vaccines have their share of rare adverse events. We report a case of antineutrophil cytoplasmic antibody (ANCA)-associated pauci-immune crescentic glomerulonephritis 15 days post 2nd dose of a killed COVID-19 (COVAXIN™ -BB152 V) vaccine. We hypothesize that vaccination triggered a systemic immune response in a susceptible patient to develop ANCA-associated vasculitis (AAV), leading to rapidly progressive glomerulonephritis (RPGN).
Keywords
Adverse event
ANCA vasculitis
autoimmunity
COVAXIN
COVID vaccination
Case Report
A 67-year-old South-Asian female presented to us with complaints of lassitude and swelling over feet 2 weeks after receiving her second dose of the COVAXIN™ (BB152 V) vaccine on May 14, 2021. A week after these symptoms, she was evaluated and found to have serum creatinine of 2.8 mg/dl; however, she did not receive any specific evaluation or treatment outside. Her condition continued to worsen and she developed progressive nausea, decrease in appetite, increase in swelling, and breathlessness over the next week. Her serum creatinine increased to 4.8 mg/dl for which she was admitted with us for further evaluation.
Her medical history included hypertension for the last 10 years for which she was on tablet losartan 50 mg once a day. She had no allergies and denied history of taking alternate medications, painkillers, or illicit drug use in the recent past. Her baseline creatinine was 1.2 mg/dl in December 2020. On admission, she had an elevated BP of 170/100 mm Hg, and her physical examination revealed bilateral pitting pedal edema and fine crackles over bilateral lower lung fields. The initial laboratory results showed creatinine of 6.4 mg/dl, blood urea level of 117 mg/dl, sodium 131 mmol/l, potassium 6.2 mmol/l, bicarbonate 17.4 mEq/l, hemoglobin 7.7 g/dl, total leucocyte count of 8.09 × 103/uL, and platelet count of 277 × 103/uL. Urinalysis revealed 2+ proteinuria and microscopic hematuria (35-40 RBC/HPF) with a spot urine protein creatinine ratio of 3.32 gm/gm. Renal ultrasound reported normal-sized kidneys with normal cortico-medullary differentiation and no hydronephrosis. In view of hyperkalemia and congestive features, she underwent urgent hemodialysis after insertion of a non-tunneled hemodialysis catheter.
A working diagnosis of RPGN was made. Her viral serology (Anti-HCV, HBsAg, and HIV) were negative, and complement levels (C3, C4) were normal. Additional serologic workup showed positive perinuclear ANCA with antibody titers of 100 AU/ml to Myeloperoxidase (MPO). Her Proteinase 3 antibody and anti-glomerular basement membrane antibody were negative; she was started on pulse steroid (intravenous methylprednisolone 500 mg) and underwent a USG-guided percutaneous kidney biopsy.
Kidney biopsy [Figure 1] in a single linear core had 6 glomeruli of which 5 revealed crescents (3 cellular, 1 fibrocellular, and 1 fibrous) and necrotizing lesion with fibrinoid necrosis in crescentic glomeruli along with moderate Interstitial fibrosis and tubular atrophy (25%–30%). Immunofluorescence was negative for complement, immunoglobulins, and light chain (Kappa and Lambda) confirming the diagnosis of pauci-immune glomerulonephritis [Figure 2].
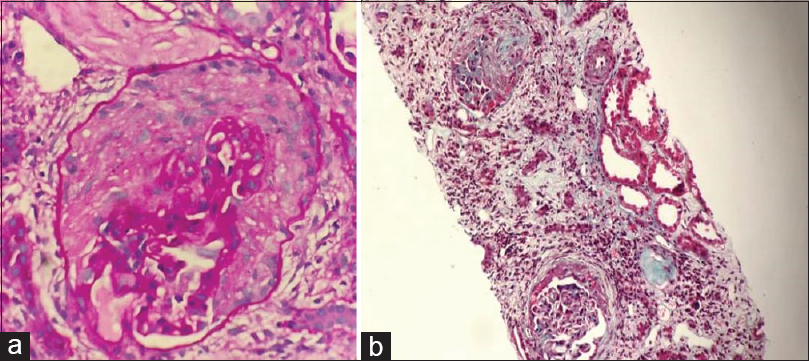
- (a) Glomerulus showing cellular crescent occupying 3/4th of the area. PAS stain, high power (40×). (b) Tubular atrophy with interstitial fibrosis with adjoining tubules showing compensatory dilatation and periglomerular fibrosis. Mason trichrome stain – medium power (20×).
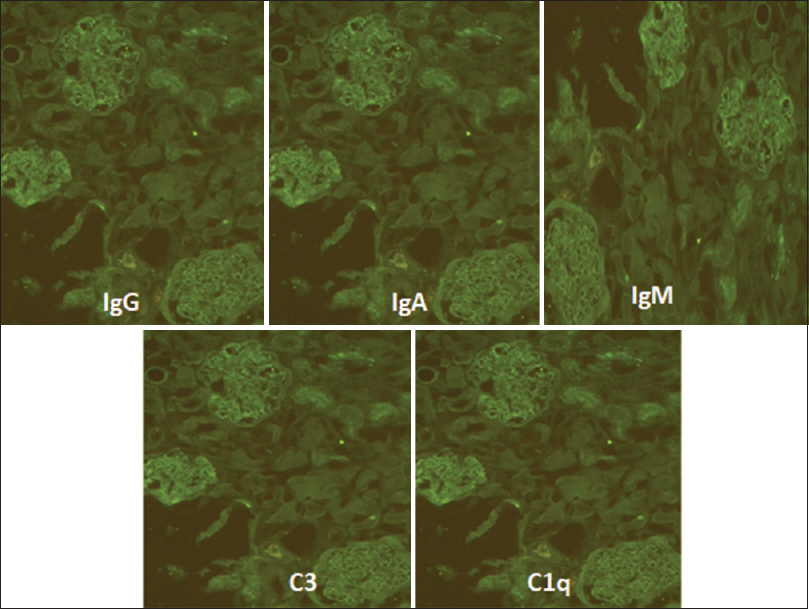
- Immunofluorescence negative for complements and immunoglobulins. Low power (10×).
Based on serologic and biopsy findings, a diagnosis of ANCA-associated pauci-immune crescentic glomerulonephritis was made. Intravenous cyclophosphamide at a dose of 10 mg/kg was given after completing pulse MP for 3 days. The patient received two more dialysis and then her urine output improved and kidney function stabilized. Currently, she is dialysis independent, on oral prednisone, and has received the 2nd dose of cyclophosphamide 2 weeks after the first dose. Her last serum creatinine on follow-up (1-month post-diagnosis) was 3.8 mg/dl [Table 1].
| Laboratory parameters | Day of admission | At 1st dose of Cyclophosphamide | At 2nd dose of Cyclophosphamide |
|---|---|---|---|
| Blood urea (mg/dl) | 117 | 128 | 88 |
| Creatinine (mg/dl) | 6.4 | 6.1 | 3.8 |
| Sodium/Pottasium | 131/6.2 | 136/4.2 | 138/4.4 |
| Hemoglobin (g/l)/Total leukocyte count (×103/l) | 7.7/8.09 | 8.1/9.3 | 9.8/6.7 |
| Urine routine | 3+ Proteinuria | 3+ Proteinuria | 2+ Proteinuria |
| 30-40 RBC | 30 RBC | 20 RBC | |
| Urine Protein estimation (UPCR – gram/gram) | 3.32 | - | 2.3 |
| HIV, HbsAg, Anti HCV | Negative | - | - |
| C3, C4 | 90, 38 | - | - |
Discussion
COVAXIN® (BB152 V) is India's indigenous COVID-19 vaccine, which is developed by Bharat Biotech in collaboration with the Indian Council of Medical Research (ICMR) and the National Institute of Virology (NIV). The vaccine is developed using Whole-Virion Inactivated Vero Cell-derived platform technology and has shown good efficacy against all variants of coronavirus in phase 2 and phase 3 trials.[12]
ANCA glomerulonephritis has been known to occur with certain medications such as hydralazine, procainamide, sulfadiazine, and other drugs, and is usually associated with moderately high anti-myeloperoxidase-O titers;[3] however, this patient denies history of taking any such drug. ANCA vasculitis has previously been reported after influenza vaccination[4] and during the course of this report, we found two more case reports of denovo ANCA vasculitis post vaccination, although it was after an mRNA vaccine and was positive for PR3 ANCA instead.[56]
The exact mechanism by which vaccinations trigger autoimmune disease yet remains unproven. Molecular mimicry, polyclonal activation, or the induction of systemic or local proinflammatory states are the proposed mechanism.[7] In this case, the temporal association suggests an immune response to the vaccine as a potential trigger. Enhanced immune response to adjuvants used in inactivated vaccines after a second dose could be responsible for triggering MPO antibodies. Patient's IgG antibodies to SARS-CoV-2 directed against the spike protein using indirect chemiluminescence immunoassay (CLIA) were >400 AU/ml at the time of admission.
In this report, we described a case suggesting a temporal relationship between COVID vaccination and MPO-AAV presenting as RPGN. This is the first report of this rare adverse event post inactivated COVID vaccine. Further research is needed to evaluate this potential causal relationship. While the pandemic is an ongoing challenge for patients and physicians, research into vaccine response and their side effects continues. It is likely that additional cases of vaccination-induced vasculitis will come up given the massive scale of global vaccination. In general, COVID vaccines are considered to be safe however clinicians should be aware of this rare phenomenon.
Declaration of patient consent
The patient consented to access health records both in respect of the current study and any further research that may be conducted in relation to it.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Safety and immunogenicity clinical trial of an inactivated SARS-CoV-2 vaccine, BBV152 (a phase 2, double-blind, randomised controlled trial) and the persistence of immune responses from a phase 1 follow-up report. 2020. medRxiv. doi: https://doi.org/10.1101/2020.12.210.20248643
- [Google Scholar]
- Efficacy, safety, and lot to lot immunogenicity of an inactivated SARS-CoV-2 vaccine (BBV152): A, double-blind, randomised, controlled phase 3 trial. 2021. medRxiv. doi: https://doi.org/10.1101/2021.060.30.21259439
- [Google Scholar]
- Drug-induced glomerular disease: Immune-mediated injury. Clin J Am Soc Nephrol. 2015;10:1300-10.
- [Google Scholar]
- ANCA-associated vasculitis following influenza vaccination: Causal association or mere coincidence? J Clin Rheumatol. 2009;15:289-91.
- [Google Scholar]
- De novo vasculitis after mRNA-1273 (Moderna) vaccination. Kidney Int. 2021;100:474-6.
- [Google Scholar]
- ANCA glomerulonephritis post Moderna COVID-19 vaccination. Kidney Int. 2021;100:473-4.
- [Google Scholar]
- Vaccination and autoimmune disease: What is the evidence? Lancet. 2003;362:1659-66.
- [Google Scholar]







