Translate this page into:
Prevalence and risk factors of hyperuricemia among kidney transplant recipients
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Hyperuricemia is common in renal transplant patients (RTRs), especially those on cyclosporine (CsA)-based therapy. We conducted a retrospective study to determine the prevalence of hyperuricemia and its risk factors among RTRs. A total of 17,686 blood samples were obtained from 4,217 RTRs between April 2008 and January 2011. Hyperuricemia was defined as an uric acid level of ≥7.0 mg/dl in men and of ≥6 mg/dl in women that persisted for at least two consecutive tests. Majority (68.2%) of RTRs were normouricemic. Hyperuricemia was more frequent in younger and female RTRs. On multivariate logistic regression, we found high trough level of cyclosporine to be a risk factor for hyperuricemia. In addition, female gender, impaired renal function, and dyslipidemia (hypercholesterolemia, hypertriglyceridemia, and elevated LDL) were also associated with higher probability of hyperuricemia. Hyperuricemia is a common complication after renal transplantation. Risk factors implicated in post-transplant hyperuricemia include high trough level of cyclosporine, female gender, renal allograft dysfunction, and dyslipidemia.
Keywords
Elderly
hyperuricemia
kidney transplantation
Introduction
Asymptomatic hyperuricemia is seen in 2.3 to 17.6% of general population in different studies.[1] Hyperuricemia is common in renal transplant patients, especially those on cyclosporine (CsA)-based immunosuppression with a high prevalence rate of 30 to 84%.[1–4] Renal allograft failure, use of diuretics, and obesity are other risk factors of hyperuricemia following renal transplantation.[256]
Although the impact of hyperuricemia after kidney transplantation on graft outcome has not been fully established, a small number of studies have suggested that an increased serum uric acid (SUA) level is a prognostic factor for the development of renal allograft impairment.[57–9] However, other investigators have not shown an adverse effect of post-transplant hyperuricemia on the graft survival.[11011]
There are a limited number of prospective studies with large number of kidney transplants that evaluate post-transplant hyperuricemia in literature. Therefore, we conducted a large retrospective observational study to determine the prevalence of hyperuricemia and its risk factors among 4,217 Iranian renal transplant recipients.
Materials and Methods
Participants
A retrospective observational study was conducted to assess the prevalence of hyperuricemia and its risk factors among 4,217 renal transplant recipients who were from 12 kidney transplant centers, at Tehran, Iran between April 2008 and January 2011. All laboratory tests such as serum uric acid (SUA) were measured in a single laboratory. In this period, 17686 blood samples were obtained from all patients. This study was approved by the Local Ethics Committee of Baqiyatallah University.
All the patients received triple immunosuppressive therapy:[1] CsA (targeting a trough level (C0) of 200 to 300 ng/ml for the first three months, 100 to 250 ng/ ml for the next 4 to 12 months, and 100 to 150 ng/ml thereafter);[2] mycophenolate mofetil (1–2 g per day) or azathioprine (1–2 mg/kg per day), and[3] prednisolone (initially 1mg/kg daily with tapering to 5–10 mg per day for 3 to 6 months).
The clinical and biochemical data gathered for this study were recipient and donor gender, donor source (living or deceased), serum creatinine (Cr) concentration, fasting blood sugar (FBS), CsA levels, hemoglobin (Hb) value, and lipid profile (triglyceride (TG), cholesterol (Chol), HDL-cholesterol and LDL-cholesterol).
Hyperuricemia was defined as an SUA level of ≥7.0 mg/dl in men and of ≥6 mg/dl in women that persists for at least two consecutive tests performed. Moderate to severe hyperuricemia is also defined as an SUA of ≥8.0 mg/dl.
Statistics
Statistical analyses were performed using SPSS for Windows, versions 17.0. Quantitative variables were expressed as mean ± SD, and results for the qualitative variables were expressed as frequencies and percentages. The Kolmogorov-Simirnov test showed that uric acid levels were not distributed normally; hence, Spearman’s correlation analysis was used to study correlations between SUA concentrations with numeric variable such as serum Cr, age of recipient, FBS, CsA levels, Hb value, TG, Chol, LDL, and HDL levels. Comparisons of qualitative data were performed by Chi-squared test. Multivariate logistic regression analysis was used to examine the influence of factors predisposing hyperuricemia. Variables which were significant at the P < 0.2 univariate level were included in the multivariate analysis. All the tests were two-tailed, and P < 0.05 were considered statistically significant.
Results
Population characteristics
The demographic data of all recipients with and without hyperuricemia are shown in Table 1. Patients with hyperuricemia were younger than individuals with normal SUA levels [Table 1]. The majority of cases were male (63%), whereas female gender was higher in the hyperuricemic group compared to cases with normal SUA concentration (P < 0.001). The mean time since transplantation was 5 ± 4 (median: 4.2) years. No significant difference was seen in age of the donor between both the groups Table 1. The majority of grafts came from living donors (84.6% unrelated and 7.8% related), whereas 7.6% of the patients received a deceased-donor graft. The rate of deceased kidney transplantation was higher in patients without hyperuricemia when compared to hyperuricemic recipients.
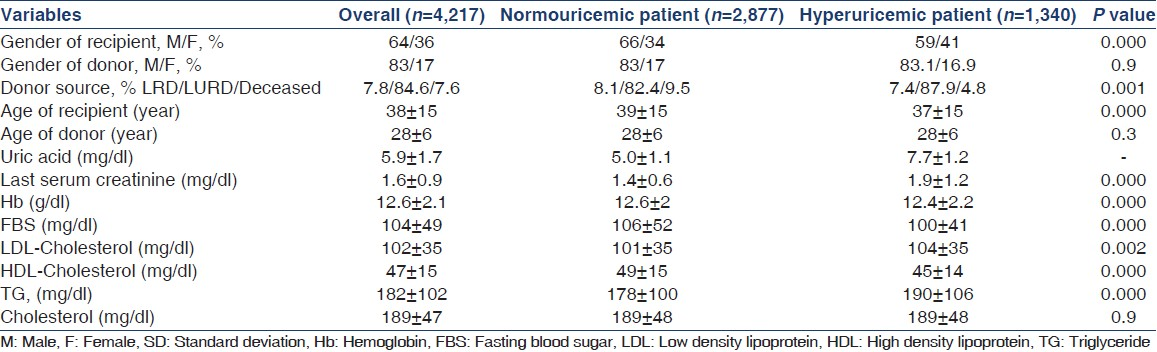
Of the 4,217 kidney transplant recipients, 2,877 (68.2%) were normouricemic and 1,340 (31.8%) were hyperuricemic. Moderate to severe hyperuricemia was seen in 572 (13.6%) patients. Although hyperuricemia frequently occurred in women (34% vs. 25%, P < 0.001), the rate of moderate to severe hyperuricemia was higher in men (15.5% vs. 10.3%, P < 0.001).
There was a significant relationship between SUA and serum Cr concentration (P = 0.0001). A significant relationship was also seen between SUA and CsA levels (P = 0.0001). Higher LDL-cholesterol, lower HDL-cholesterol, hypercholesterolemia, and hypertriglyceridemia were significantly associated with elevated SUA [Tables 1 and 2]. Diabetes mellitus was seen in 14.6% of the patients and no significant correlation was found between FBS and SUA levels (P = 0.5).
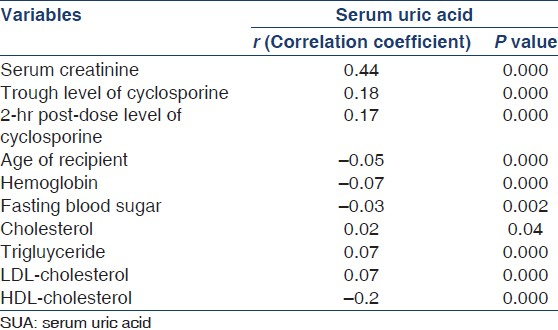
On multivariate logistic regression after adjustment for other factors, we found increased trough level of CsA to be associated with hyperuricemia. In addition, female gender, impaired renal function, and dyslipidemia (hypercholesterolemia, hypertriglyceridemia, and elevated LDL) were also associated with higher probability of hyperuricemia following kidney transplantation [Table 3].

Discussion
Hyperuricemia was a common finding among our kidney transplant recipients who received CsA and it accounted up to 32%, which is lower than a previous study (52%).[12] Other studies have reported its occurrence in 30–84% of renal transplant patients.[1–3] Min et al. showed a high prevalence of hyperuricemia at four years after renal transplantation (42%).[13] However, other studies reported that the prevalence of hyperuricemia following transplantation was higher (70–80%) than that reported in the present study.[47] Furthermore, we found that the female gender had more chance of hyperuricemia, which is opposite of findings of other reports that reported that male gender was an independent factor at multivariate analysis.[1314] Interestingly, men had more chance of moderate to severe hyperuricemia after renal transplantation in the current study.
At multivariate analysis, SUA level had correlation with blood CsA concentration in the present study. Most studies demonstrate that CsA is associated with hyperuricemia after kidney transplantation.[2491415] Immunosuppression with CsA is associated with a significantly higher incidence of hyperuricemia than with azathioprine,[12] and resolves upon withdrawal of the drug,[2] implicating CsA rather than the transplant procedure itself. Although CsA is widely used after solid organ transplantation over the long term, there is still no firm consensus on the best way to monitor CsA blood levels.[16] Lin et al. found a weak but significant relationship between cyclosporine trough concentration and SUA level.[2] Also, Balci et al. reported that in pediatric hematopoietic stem cell transplant patients, measurement of C2 levels as a standard practice did not provide an advantage over C0 monitoring.[17] However, it showed that the high prevalence of hyperuricemia was related to prolonged exposure to CsA rather than to its dose or serum concentration.[18] Similarly, other reports indicated that the high prevalence of hyperuricemia after renal transplantation was allied to prolonged use of CsA.[249] Hyperuricemia has been reported in cardiac allograft recipients who received CsA therapy and in non-transplant patients receiving CsA for autoimmune diseases. Tacrolimus, a calcineurin-inhibitor, also causes hyperuricemia.[4] On the other hand, hyperuricemia in a series of 196 surviving adult heart or heart/lung transplant recipients was not correlated with CsA level.[3] The exact pathogenesis of hyperuricemia in this setting is complex and not fully elucidated. It is postulated that the intra-renal vasoconstriction and decreased coefficient of glomerular ultrafiltration due to acute CsA nephrotoxicity would cause enhanced tubular urate reabsorption,[2] whereas the reduced renal mass associated with chronic CsA nephrotoxicity would eventually lead to a reduction in urate secretion.[2] A small series of 19 pediatric renal transplant recipients suggested that increase of CsA induced hyperuricemia.[19] Cyclosporine reduces the urinary clearance of uric acid; however, its mechanism is unknown and it may involve alteration in tubular transport.[9]
Hyperuricemia also exacerbates renal disease in animals with remnant kidneys or with chronic CsA toxicity.[20] The mechanisms of this injury may be uric acid-induced endothelial dysfunction, activation of the renin-angiotensin system, and the development of glomerular hypertension and renal vasoconstriction.[20] The prolonged hyperuricemia may be associated with chronic tubulointerstitial disease, afferent arteriolopathy, intrarenal vasoconstriction, and increased vascular resistance; hence, it might contribute to chronic CsA nephropathy.[21] The absorption of CsA was affected by SUA in kidney transplant patients and experimental rats. It suggests that transplant recipients with high SUA may have poor absorption of CsA.[22] There are studies showing that CsA reduces glomerular filtration rate and leads to hyperuricemia.[2] Nonetheless, decreased secretion of uric acid in the proximal tubules might also contribute to high SUA.[19]
In the current study, impaired allograft renal function was also associated with hyperuricemia. This finding is similar to those studies showing that hyperuricemia is a risk factor for renal allograft dysfunction.[57–9] Gerhardt et al.[8] showed a lower five-year graft survival in hyperuricemic patients (69%) compared to those with normouricemia (83%). Min et al., found that moderate to severe hyperuricemia after kidney transplantation was identified as a significant risk factor of renal allograft impairment and graft loss at multivariate analysis.[13] One small study also demonstrated that hyperuricemia was a risk factor for graft loss.[23] On the other hand, Akgul et al.[10] had results that were different from our findings, suggesting that hyperuricemia had no impact on the incidence of chronic allograft nephropathy within the first three years after transplantation. Gores et al.[1] also showed that there was no difference in serum creatinine levels between hyperuricemic and normouricemic patients. In fact, these short-term follow-up studies[110] have shown that hyperuricemia after renal transplantation had no adverse effect on the graft survival. Interestingly, a subanalysis of the Symphony study on 1,645 recipients reported a lack of any significant association between SUA levels and progression of renal dysfunction in the first three post-transplant years.[11] Higher serum creatinine concentrations were associated with elevated SUA levels; however, higher SUA values were not independently associated with deterioration of allograft renal function after renal transplantation.[11] Indeed, after correcting for baseline renal function, there was no relationship of renal allograft impairment in patients with higher SUA levels.[11]
The limitations of this study included its retrospective nature as well as the absence of long-term follow-up data. Moreover, other contributing factors such as body mass index of these patients should have been analyzed. Additional prospective randomized trials with a larger cohort of renal transplant patients are required to confirm the impact of increased CsA blood level as a risk factor for hyperuricemia, which was found in the present study. Moreover, to determine the cause and effect correlation of SUA and graft dysfunction, the advantageous effect of uric acid-lowering therapy should be evaluated in prospective randomized studies including a large cohort of recipients. Nevertheless, the data of this study are still reliable because of the huge sample size.
Conclusion
Hyperuricemia is a prevalent complication after renal transplantation. Several risk factors implicated in post-transplant hyperuricemia include increased trough level of CsA, female gender, renal allograft dysfunction, and dyslipidemia.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Hyperuricemia and gout among heart transplant recipients receiving cyclosporine. Am J Med. 1992;92:141-6.
- [Google Scholar]
- Renal transplant-associated hyperuricemia and gout. J Am Soc Nephrol. 2000;11:974-9.
- [Google Scholar]
- Small-bowel mucosal transglutaminase 2-specific IgA deposits in coeliac disease without villous atrophy: A prospective and randomized clinical study. Scand J Gastroenterol. 2005;40:564-72.
- [Google Scholar]
- Does uric acid have a pathogenetic role in graft dysfunction and hypertension in renal transplant recipients? Transplantation. 2005;80:1565-71.
- [Google Scholar]
- Influence of hyperglycemia and hyperuricemia on long-term transplant survival in kidney transplant recipients. Clin Transplant. 1999;13:375-9.
- [Google Scholar]
- Is uric acid a predictive factor for graft dysfunction in renal transplant recipients? Transplant Proc. 2007;39:1023-6.
- [Google Scholar]
- Uric acid levels have no significant effect on renal function in adult renal transplant recipients: Evidence from the symphony study. Clin J Am Soc Nephrol. 2009;4:1655-60.
- [Google Scholar]
- Moderate-to-severe early-onset hyperuricaemia: A prognostic marker of long-term kidney transplant outcome. Nephrol Dial Transplant. 2009;24:2584-90.
- [Google Scholar]
- Role of uric acid in post-renal transplantation hypertension. Transplant Proc. 2009;41:1634-6.
- [Google Scholar]
- Hyperuricemia is associated with the development of the composite outcomes of new cardiovascular events and chronic allograft nephropathy. Transplantation. 2008;86:652-8.
- [Google Scholar]
- Cyclosporine monitoring in organ transplantation: Do we need a new concept? Nephron Urol Mon. 2011;3:97-8.
- [Google Scholar]
- Cyclosporine level at the second hour in pediatric hematopoietic stem cell transplant patients. Exp Clin Transplant. 2011;9:329-35.
- [Google Scholar]
- Mechanisms of hyperuricemia in cyclosporine-treated renal transplanted children. Nephron. 1996;74:318-23.
- [Google Scholar]
- Hyperuricemia influences chronic cyclosporine nephropathy. Transplant Proc. 2008;40:167-70.
- [Google Scholar]
- Effect of plasma uric acid on pharmacokinetics of cyclosporine A in living-related renal transplant recipients and pharmacokinetic study in rats with experimental hyperuricaemia. J Clin Pharm Ther. 2010;35:323-32.
- [Google Scholar]
- The independent association between serum uric acid and graft outcomes after kidney transplantation. Transplantation. 2010;89:573-9.
- [Google Scholar]







