Translate this page into:
Proliferative glomerulonephritis causing acute renal failure in a child with Salmonella septicemia
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
An 11- year- old male presented with fever since 6 days, hematuria since 4 days, pain in abdomen and oliguria since 3 days. There was no dysuria, frequency or pyoderma in the recent past. Growth and development was normal. On examination, he was sick, febrile and hypertensive (BP 132/98 mm Hg). He had mild pallor, facial puffiness, pedal edema and mild hepatosplenomegaly.
Urine analysis showed 3 + proteinuria, 100-120 RBCs and 8-12 WBCs/hpf and red cell casts. FeNa was < 1 (0.82). The 24-h urine protein was 1.21 g/day (>40 mg/m2/24 hours). Serum creatinine was 7.1 mg/dl with serum albumin 2.7 g/dl and serum cholesterol 156 mg/dl. Ultrasonography abdomen showed bulky kidneys with increased cortical echogenicity and prominent pyramids.
Anti-streptolysin O (ASLO) titers were normal. C3 levels were 84 mg/dl (normal > 90 mg/dLdl). Urine culture showed no growth. Blood culture grew Salmonella typhi and Widal test was positive (“O” titers 1:160 and “H” titers 1:2560). Other investigations were normal.
In view of oliguric renal failure, the patient was started with hemodialysis and other supportive treatment. He required 2 weeks of hemodialysis. In view of persistent renal dysfunction and normal ASLO titers kidney biopsy was done, which revealed nine enlarged glomeruli showing mild increase in mesangial cellularity, extensive infiltration by neutrophils and no crescents. Tubules, interstitium and blood vessels were unremarkable. Features were suggestive of diffuse proliferative glomerulonephritis [Figure 1]. Immunoflorescence showed no deposits.
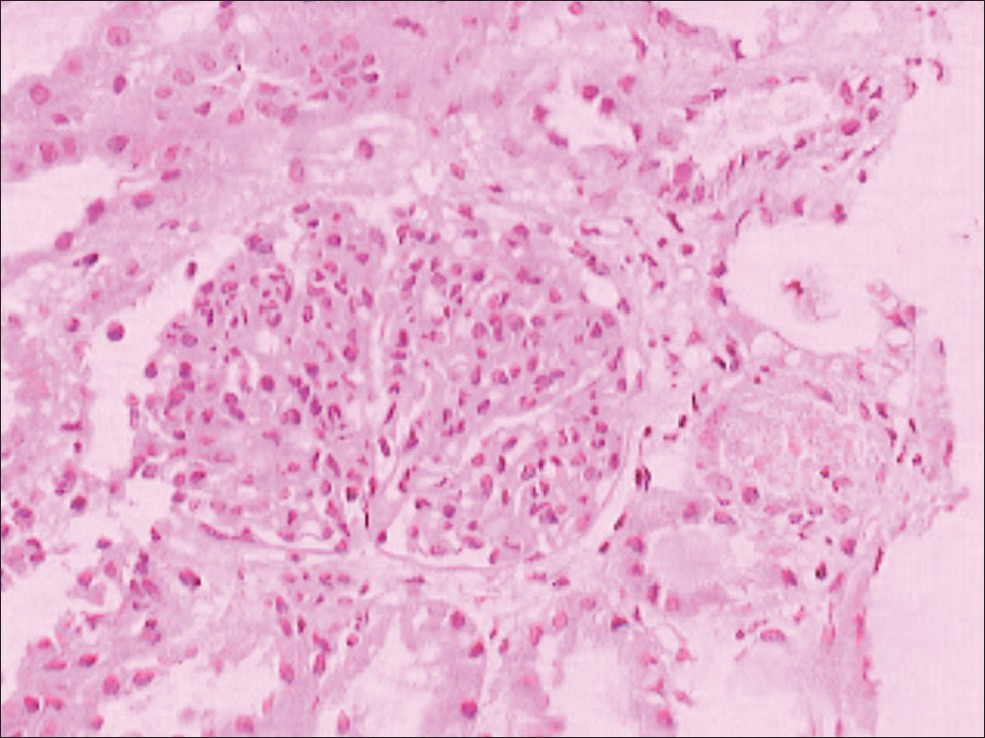
- Renal biopsy (Light microscopy) showing proliferative glomerulonephritis with increased mesangial cellularity and extensive neutrophilic infiltration in glomeruli
At discharge, the patient had serum creatinine of 1.3 mg/dl and was on one anti-hypertensive agent. Serum creatinine and C3 levels came to normal after 4 weeks. Microscopic hematuria and hypertension took 6 months to resolve, while proteinuria resolved completely after 1 year.
Renal involvement with enteric fever is noticed only in 2–3% of the cases. The common complications of typhoid related to the urinary tract include cystitis, pyelitis, pyelonephritis and mild proteinuria.[1] Different mechanisms can lead to renal involvement in typhoid fever. Dehydration not managed correctly may lead to acute tubular necrosis. Other renal manifestations like Immunoglobulin A (IgA) nephropathy, hemolytic uremic syndrome and Henoch- Schonlein purpura may also occur. Acute interstitial nephritis and acute tubular dysfunction secondary to Salmonella typhimurium has been reported in children and adults either in isolation or with schistosomiasis.[2] Renal failure secondary to rhabdomyolysis has also been reported.
Glomerulonephritis is uncommon.[3] Immune complex glomerulitis, with deposition of immunoglobulins and C3 globulin, is seen in these patients. Salmonella Vi antigen was also found in the glomerular capillary wall, suggesting the direct role of Salmonella typhi in the pathogenesis of the glomerular lesion.[4] The present case showed diffuse proliferative glomerulonephritis in renal biopsy. Buka et al., showed patients with typhoid nephritis compared to post- streptococcal glomerulonephritis (PSGN) have edema for prolonged periods before admission, are likely to be febrile and have splenomegaly. C3 levels are lower in PSGN patients (P < 0.01),[5] findings similar to this case.
References
- Nephritis and cerebellar ataxia: rare presenting features of enteric fever. J Postgrad Med. 2000;46:184-6.
- [Google Scholar]
- Acute renal tubular dysfunction in association with Salmonella enteritidis. Indian Pediatr. 2004;41:395-6.
- [Google Scholar]
- Acute renal failure likely due to acute nephritic syndrome associated with typhoid fever. Intern Med. 2005;44:1074-7.
- [Google Scholar]






