Translate this page into:
Prospective analysis of utility and feasibility of ambulatory blood pressure monitoring service in a pediatric nephrology set up
Address for correspondence: Dr. Rajiv Sinha, 37, G Bondel Road, Kolkata - 700 019, West Bengal, India. E-mail: rajivsinha_in@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Despite ambulatory blood pressure monitoring (ABPM) becoming standard of care in adult practice[1] as well as its strong recommendation in pediatric hypertension (HT) guidelines[23] there are very few reports on its utility and feasibility in children from emerging economy and none from Indian subcontinent.[4] We hereby present a prospective analysis of an ABPM service initiated in February 2012. Pediatric ABPM service was initiated with Welch Allyn 6100 monitor using appropriate blood pressure (BP) cuff sizes. It was offered to all children above 5 years of age with incidental (without any obvious underlying reason for HT) clinic blood pressure (CBP) persistently ≥95th percentile (p) but ≤99th p +5 mm Hg or as a standard of care for children with chronic kidney disease (CKD) (≥stage 3), post renal transplant (RTx), solitary kidney, renal scar, and post-op for coarctation of the aorta. The American Heart Association (AHA) recommendation[2] was taken as standard and ABPM limits were set accordingly. Height was used for estimating the ABPM limits or age if height was less than 120 cm.[23] Interpretation was as per AHA suggestions-normal: (CBP < 95th p, mean ABPM < 95th p and systolic load (SL) <25%), white coat hypertension (WCH): (CBP > 95th p, mean ABPM < 95th p and SL < 25%), masked hypertension (MH): (CBP < 95th p, mean ABPM > 95th and SL < 25%), pre-HT: (CBP > 95th p, mean ABPM < 95th p and SL > 25% but < 50%), ambulatory hypertension (AH): (CBP > 95th p, mean ABPM > 95th p and SL > 25%, but < 50%) and severe AH: (CBP < 95th p, mean ABPM < 95th p and SL > 50%). Until 31st March 2013; 69 children had ABPM (26% female) with the median age of 9.2 years (range 5-18). As per the AHA recommendation all of them had at least one reading per hour and the total number of readings were greater than 40 (median number of total reading was 52 with range 41-72). Sleep diary was used to ascertain day and night time. Underlying reason for undertaking ABPM and the outcome are shown in Figure 1. Incidental HT was the most common underlying reason. WCH was found in 27% (n = 19) of the total subjects and MH in 4% (n = 3). On analysis of utility; ABPM resulted in definite change in management in 36% of the cases (n = 25). Whereas WCH was detected in 19 children MH was detected in three cases (all three cases were of CKD including one post RTx). In addition, anti-hypertensive medications were increased in another three cases of known hypertensive wherein ABPM showed severe ambulatory HT although CBP was only around 95th percentile. In conclusion, similar to western literature[2] we also found a high incidence of WCH (27%) as well as MH (21% among CKD and RTx). Diagnosis of WCH does avoid further costly investigation as well as use of anti-hypertensive medications,[5] whereas diagnosis of MH can result in more effective control of BP, which is likely to result in improved renal outcome. Although small in numbers, our study supports the use of pediatric ABPM even in Indian circumstances and should encourage its increased utilization.
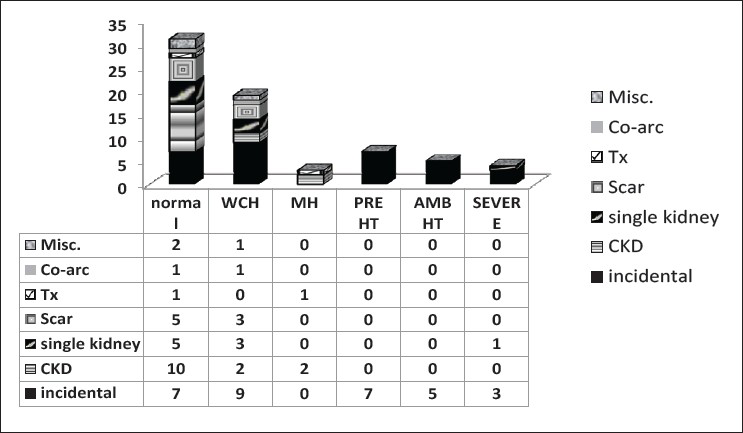
- Outcomes of the ambulatory blood pressure monitoring. ABPM = ambulatory blood pressure monitoring, CKD = Chronic Kidney Disease, Co – arc = co-arctation, HT = hypertension, MH= masked hypertension, Misc = miscellaneous, Tx = Renal transplant
References
- Ambulatory blood pressure monitoring in children and adolescents: Recommendations for standard assessment: A scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee of the council on cardiovascular disease in the young and the council for high blood pressure research. Hypertension. 2008;52:433-51.
- [Google Scholar]
- Management of high blood pressure in children and adolescents: Recommendations of the European Society of Hypertension. J Hypertens. 2009;27:1719-42.
- [Google Scholar]
- Home and ambulatory blood pressure to identify white coat and masked hypertension in the pediatric patient. Am J Hypertens. 2011;24:893-7.
- [Google Scholar]
- Cost-effectiveness of ambulatory blood pressure monitoring in the initial evaluation of hypertension in children. Pediatrics. 2008;122:1177-81.
- [Google Scholar]






