Translate this page into:
Comparison of Overhydration with Ambulatory Hypertension in Pediatric Chronic Peritoneal Dialysis: A Prospective Observational Study
Corresponding author: Arpana Aprameya Iyengar, Department of Pediatric Nephrology, St Johns Medical College Hospital, Bangalore, Karnataka, India. E-mail: arpanaiyengar@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Reddy S, Iyengar AA. Comparison of Overhydration with Ambulatory Hypertension in Pediatric Chronic Peritoneal Dialysis: A Prospective Observational Study. Indian J Nephrol. doi: 10.25259/IJN_275_2024
Abstract
Background
Overhydration (OH) and hypertension are frequently encountered in children on chronic peritoneal dialysis and contribute to cardiovascular morbidity and mortality. The assessment of OH by bedside tools and its association with blood pressure needs to be addressed in children on continuous ambulatory peritoneal dialysis (CAPD). This prospective study was undertaken in children on CAPD to detect OH by lung ultrasound (OH-LU) and bioimpedance vector analysis (OH-BIVA) and to assess the association of OH with ambulatory blood pressure (ABPM).
Materials and Methods
Clinically stable children aged 5–18 years on CAPD were subjected to OH-LU, OH-BIVA, and ABPM at enrollment and short-term follow-up (<12 weeks). Children were categorized as OH-BIVA based on the position of the vector on a reference graph derived from 50 healthy children. Presence of >5 B-lines was defined as OH-LU. Uncontrolled ambulatory hypertension (UH) included systolic, diastolic, or mean arterial pressures ≥95th percentile.
Results
Fifteen children (aged 10.3 ± 2.1 years, eight girls) on CAPD for 40.3 ± 29.1 months were studied. The burden of OH-LU and OH-BIVA at enrollment was 33% and 20%, respectively, while 73% had UH. At the end of the study (median 8 (6,12) weeks), a reduction in OH-BIVA was observed in 33.3%, 40% by OH-LU with an 18% reduction in UH. There was no significant association between OH-BIVA or OH-LU and UH at enrollment or follow-up.
Conclusion
In clinically stable children on CAPD, the commonly observed UH was not associated with OH measured by BIVA or LU at baseline and during short-term follow-up.
Keywords
Overhydration
Ambulatory hypertension
Pediatric peritoneal dialysis
Bioimpedance vector analysis
Lung ultrasound
Introduction
Hydration status is a major determinant of cardiovascular morbidity and mortality in children on dialysis.1,2 Establishing an optimal target weight is a critical component of the dialysis prescription, as over- or underestimation of the target weight could have deleterious consequences. In the pediatric population, target weight has traditionally been ascertained based on blood pressure (BP) control and the presence of clinical signs of overhydration (OH).3
In children on chronic peritoneal dialysis (CPD), including automated peritoneal dialysis (APD) and chronic ambulatory peritoneal dialysis (CAPD), OH is encountered in 30–45%.4,5 This may not reflect the true prevalence as adequate assessment of OH in children is hampered by the absence of reliable, accurate, and objective tools as well as the lack of high-quality evidence supporting newer techniques. Adjusting CPD prescription based on clinical assessment of hydration status, despite being the most frequently used method, is subjective, inconsistent, and has significant limitations.6
Gold standard dilution methods for measuring body fluid volumes are invasive, cumbersome, expensive, and impractical in routine clinical practice. Lung ultrasound (LU) and bioimpedance analysis (BIA) are objective tools that have been shown to be superior to clinical evaluation and comparable to gold standard methods for assessment of hydration status in adult patients on dialysis.7,8 The main difference between these tools lies in the fluid compartment being analyzed. LU primarily detects extravascular lung volume, while BIA provides information regarding intracellular fluid (ICF), extracellular fluid (ECF), and total body water (TBW).7 Bioimpedance spectroscopy (BIS), has similar efficacy as BIA for hydration status evaluation in patients with kidney failure.4
The measurements of TBW and ECW by BIA are based on predictive equations derived from healthy adult Caucasians and confounded by tissue hydration, limiting their use in children. These shortcomings of BIA are overcome by bioimpedance vector analysis (BIVA), a variant of BIA, which is a qualitative and semiquantitative graphical representation of resistance (R) and reactance (Xc), with an added advantage of combined tracking of hydration and nutritional status.9 These graphs play an integral role in adjusting target weight and have a proven efficacy in reducing mortality in adult patients on HD and CPD.10
There is limited evidence for the utility of these tools to detect subclinical OH in children on CPD and also a lack of validated reference BIVA graphs for children.11 Uncontrolled hypertension (UH), hypertension requiring >2 antihypertensive medications, associated with cardiovascular morbidity and mortality, is reported in 75–90% of children on CPD.12 Ambulatory blood pressure monitoring (ABPM) is the gold standard for detecting and monitoring hypertension in children on CPD.13
Management of hypertension in children on dialysis usually begins with addressing volume status. Although hypertension is considered as one of the universal clinical indicators of OH, there is ambiguity regarding the relationship between OH and hypertension in children on dialysis.4
It is imperative to identify bedside tools to assess OH in children on CPD and establish the relationship between hypertension and OH, ensuring appropriate modification to dialysis prescriptions and antihypertensive medications. The objectives of this study were to assess the burden of OH and UH, and to determine the association of OH (detected by BIVA or LU) with UH (by ABPM) in children on CAPD at baseline and short-term follow-up within three months.
Materials and Methods
A prospective observational study was conducted in children aged 5–18 years on CAPD on regular follow-up at the CKD clinic in St Johns Medical College Hospital, a tertiary pediatric nephrology center, from March to September 2021.
Clinically stable children on CAPD for more than one month were included, while those with clinical OH (defined below), metallic implants like nails, stents, or prostheses, amputees, or non-compliant with assessment and follow-up were excluded from the study. The study was approved by the Institutional Ethics Board (IEC 85/2021) and informed consent and assent (when applicable) were taken at enrollment.
Eligible children on CAPD were recruited and subjected to the assessment of OH by BIVA (OH-BIVA), OH by LU (OH-LU), and 24-hour ABPM monitoring. These measurements were repeated at one follow-up visit within 12 weeks of enrollment. The study protocol is depicted in Figure 1. The standard CAPD prescription, as decided by the treating team, consisted of 1.5% or 2.5% glucose-based bags with a dwell volume of 800–1200mL/m2 and an average duration of 12–24 hours. Treatment changes were based on the clinician’s judgment as per the standard of care. Analysis was undertaken in only those children who completed the follow-up measurements.
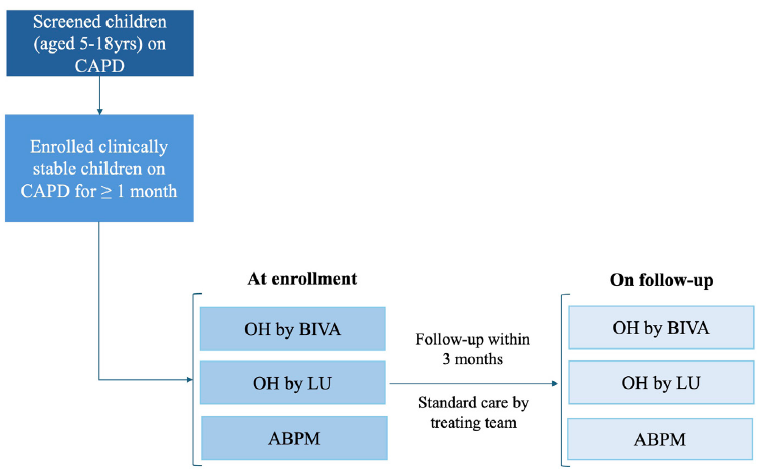
- Study protocol. ABPM: Ambulatory blood pressure monitoring, BIVA: Bioimpedance vector analysis, CAPD: Chronic ambulatory peritoneal dialysis, LU: Lung ultrasound, OH: Overhydration.
Sample size estimation
As no previous available literature exists comparing OH-BIVA and/or OH-LU and ambulatory hypertension in children, our sample size was based on the number of children on CAPD at our center. The expected number of patients encountered during our study period of six months (including follow-up), based on a study undertaken in children on CPD with BIS monitoring, was estimated at 15, calculated for precision of 5% and power of 80%.14
Data collection
At enrollment, clinicodemographic information, including details of native kidney disease, CAPD prescription, and antihypertensive medications were documented. Residual kidney function (RKF) was categorized as preserved if the 24-hour urine output was ≥150mL/day. Laboratory parameters like kidney function tests, hemoglobin, and serum albumin were also noted.
Study protocol
All enrolled children were examined by the researcher for the presence of clinical signs of OH on the day of performing BIVA and LU. Presence of signs of OH like weight gain of 7% from baseline, hypertension, edema, raised jugular venous pressure, tachycardia, gallop, basal crepitations, and hepatomegaly were recorded. Children with ≥3 of the above signs were classified as clinical OH. Weight, height, waist, and hip circumference were recorded using standard protocols.
At the follow-up visit within 12 weeks, changes to CAPD prescription, RKF, and biochemical parameters were recorded. Repeat measurement of anthropometric parameters and clinical examination for signs of OH was performed.
Assessment of OH-BIVA
A multifrequency BIA was performed using the Bodystat Quadscan 4000 (version 5/12, Bodystat Ltd., Douglas, British Isles) by the researcher, with strict adherence to the criteria established by the National Institutes of Health Technology Assessment Conference Statement.15
Single frequency bioimpedance measurements at 50 kHz were taken after the abdomen was drained, with the child in supine position using nonrecyclable gel electrodes placed on the dorsal surfaces of the right hand and foot, in accordance with the standard tetrapolar electrode placement. Values with less than 85% quality were discarded, and the mean of two sequential readings was used for analysis. The two vector components of R and Xc were normalized by the child’s height (R/h and Xc/h) and standardized as bivariate Z-score (where Z stands for the standard normal deviation), that is, zR/h and zXc/h. These zR/h and zXc/h values were plotted on reference BIVA plots created from healthy control subjects.
Creation of Gender-Specific Reference BIVA plots
To increase the robustness of the study and overcome limitations for the lack of pediatric Indian reference BIVA plots, gender-specific reference graphs were created. BIA measurements were taken in 50 healthy children (age and sex matched), 26 (52%) boys with mean (±SD) age of 10 ± 3.4 years.
Indices of zR/h and zXc/h were computed and gender-specific BIVA plots were constructed using R-programming software (R core team, GNUGPLv2, ww.rproject.org). Three tolerance ellipses were created representing the 50th, 75th, and 95th percentiles. OH, decreased body cell mass, dehydration, and increased body cell mass constituted the four quadrants formed.
In accordance with the clinically validated studies in adults and children, the position of the vector in the left lower quadrant beyond the 75th tolerance ellipse was defined as OH-BIVA.16,17
Assessment of OH-LU
After BIA was performed, OH-LU was assessed by the same trained researcher using a portable bedside machine (GE Logiq e portable ultrasound, US) with the linear 5.1–12.5 MHz probe. The validated 14-zone method of chest examination was followed and the total number of B-lines in all zones were recorded.18 The presence of >5 B-lines was defined as OH-LU.19
BP Measurement
Office BP and ABPM
Children were characterized as having significant clinical hypertension if the average systolic blood pressure (SBP) and/or diastolic blood pressure (DBP) for age, sex, and height were above the 95th percentile despite the maximum dosage of ≥2 antihypertensive medications.20 Ambulatory BP was recorded using the validated ABPM Monitor (Spacelabs 90217), a compact automated oscillometric device. Device placement and interpretation of ABPM was done according to the 2022 American Heart Association ABPM guidelines.21 Appropriate size ABPM cuff was applied to the nondominant arm and readings were obtained once every 20 minutes throughout the day and night. The study was considered valid if there was at least one valid reading per hour, and >40 readings were noted in the 24-hour period. UH was defined as average SBP, DBP, or mean arterial pressure (MAP) above the 95th percentile.21
The outcomes studied were the association of OH with UH in children on CAPD over 12 weeks of follow-up.
Statistical analysis
The data analysis was performed using STATA software (StataCorp. 2019. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC). Categorical data was presented using frequency and percentages, while continuous data was described using either mean ± standard deviation (SD) or median [Interquartile range (IQR)]. Chi-square test and independent t-test were used to study the association of OH-BIVA and OH-LU, with clinical parameters influencing hydration like age, type of native kidney disease, RKF, CAPD vintage, serum albumin for categorical, and continuous data, respectively. Association between OH (OH-BIVA or OH-LU) and UH at baseline and follow-up was assessed using Chi-square test. P-value less than 0.05 was considered as significant.
Results
Twenty-five children were screened over six months, of whom six had clinical OH and were excluded. Nineteen children who were clinically stable were enrolled. Among these children, 15 [mean (±SD) age 10.3 ± 2.1 years, eight (53%) girls] completed the follow-up measurements and were included for analysis. The median (IQR) weight at baseline and follow-up was 21.4 (18.2, 23.2) kg and 22.15 (18.5,24) kg, respectively. The cause of kidney failure was of glomerular etiology in eight (53%). Preserved RKF was seen in seven (47%). The mean (±SD) duration on CAPD was 40.3 ± 29.1 months. Other clinical and sociodemographic details are shown in Table 1.
| Clinical details of cases | N = 15 |
|---|---|
| Serum albumin, g/dL | 3.2 ± 0.7 |
| Baseline assessment | |
| Hours on CAPD per day | 16.0 ± 2.7 |
| Ultrafiltration volume, mL | 746.7 ±181.7 |
| Significant clinical hypertensiona | 8 (53.3%) |
| Average number of antihypertensive medications | 3.2 |
| Bioimpedance measure, ohm | |
| Resistance | 851.1 ± 173.8 |
| Reactance | 50.7 ± 22.9 |
| Phase angle | 2.7 ± 0.9 |
| Mean arterial pressure on ABPM | 92 ± 14.1 |
| Uncontrolled ambulatory hypertension | 11 (73.3%) |
| Follow-up assessment | |
| Follow-up [Median (IQR)] weeks | 8 (6,12) |
| Hours on PD per day | 17 ± 2.8 |
| Ultrafiltration volume, mL | 860 ±186.3 |
| Clinical OHb | 1 (6.7%) |
| Significant clinical hypertensiona | 7 (46.7%) |
| Average number of antihypertensive medications | 3.3 |
| Bioimpedance measure, ohm | |
| Resistance | 820.5 ± 165.0 |
| Reactance | 46.4 ± 16.2 |
| Phase angle | 3.3 ± 1.2 |
| Mean arterial pressure on ABPM | 91 ± 15.7 |
| Uncontrolled ambulatory hypertension | 9 (60%) |
| Details of controls | N = 50 |
| Weight [Median (IQR)], kg | 29.3 (23.9, 41.5) |
| Height, m | 1.4 ± 0.2 |
| Bioimpedance measures, ohm | |
| Resistance | 727.3 ± 119.0 |
| Reactance | 56.6 ± 12.2 |
| Phase angle | 4.4 ± 1.1 |
aSignificant clinical hypertension defined as systolic or diastolic blood pressure >95th percentile for age, gender, and height on maximum dosage of ≥2 antihypertensive medications, b Clinical OH defined by presence of at least three of the following: weight gain of 7% from baseline, hypertension, edema, raised jugular venous pressure, tachycardia, gallop rhythm, basal crepitations, and hepatomegaly. ABPM: Ambulatory blood pressure monitoring, CAPD: Continuous ambulatory peritoneal dialysis, IQR: Interquartile range, SD: Standard deviation
Burden of OH and hypertension at baseline and follow-up
In the study cohort, OH-BIVA was noted in three (20%), while five (33.3%) had OH-LU (one [6.7%] had OH-BIVA and OH-LU). Eight (58%) children in the cohort had significant clinical hypertension. UH was seen in 11 (73%). The proportion of children with OH-BIVA, OH-LU, significant clinical hypertension, and UH at baseline and follow-up is shown in Figure 2. The median (IQR) duration of follow-up was eight (6,12) weeks. During the follow-up assessment, clinical OH was seen in one (6.7%). OH-BIVA was seen in two (13%) and OH-LU was noted in three (20%) (one [6.7%] had OH-BIVA and OH-LU). The BIVA plots of the study population at baseline and follow-up are shown in Figure 3. Of the three children (two girls, one boy) with OH-BIVA at baseline, two continued to remain overhydrated while one was noted to have a reduction in OH. The tracking of hydration status is depicted in Figure 4. Significant clinical hypertension was seen in seven (47%) while UH was confirmed in nine (60%).
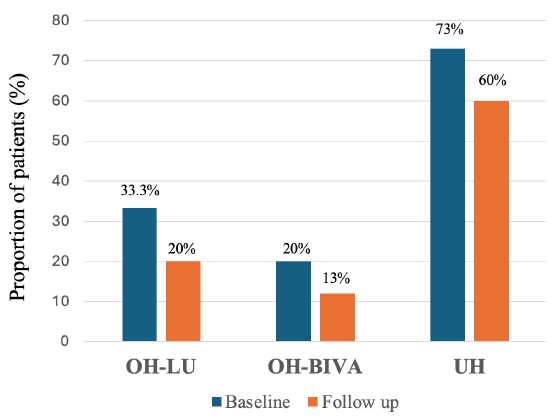
- Burden of overhydration (OH) and uncontrolled ambulatory hypertension (UH) at baseline and follow-up. The proportion of children with OH by lung ultrasound (OH-LU) and bioimpedance vector analysis (OH-BIVA) and UH at baseline (blue bars) and follow-up (orange bars) are shown.
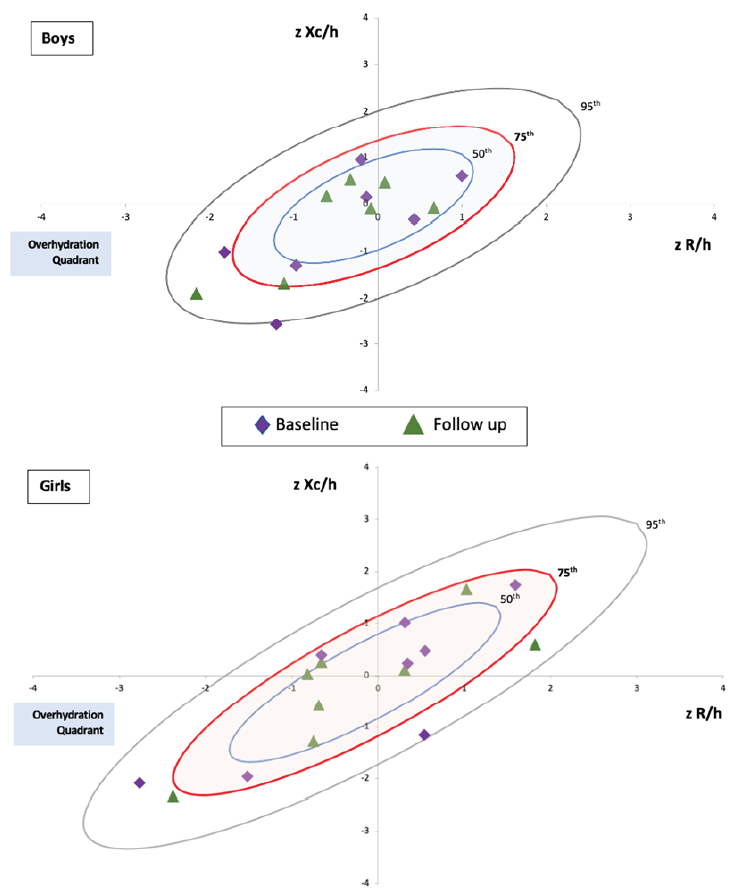
- Bioimpedance vector analysis (BIVA) graphs of the study population at baseline and follow-up. The bioimpedance measurements of resistance (R) and reactance (Xc) indexed to height (h) and standardized to bivariate z-scores (zR/h and zXc/h) of the study population at baseline (purple diamond) and follow-up (green triangle) plotted on the gender-specific reference graphs (upper panel: boys, lower panel: girls). The vector in the left lower quadrant beyond the 75th tolerance ellipse was defined as overhydration (OH) by BIVA.
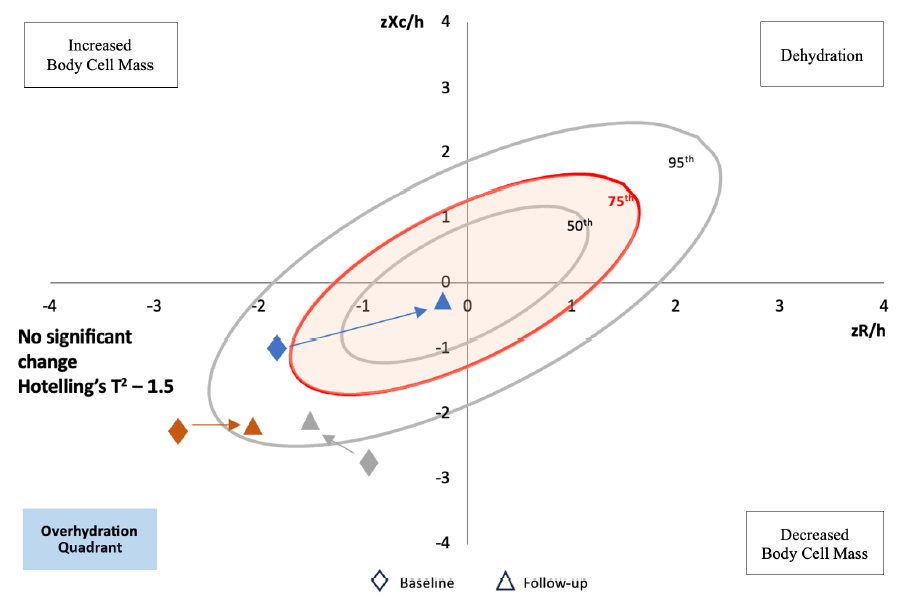
- Tracking overhydration status by the bioimpedance vector analysis (BIVA). The figure shows the BIVA reference graph with the four quadrants: overhydration (OH), decreased body cell mass, dehydration, and increased body cell mass. Standardized bivariate resistance indexed to height (zR/h) is plotted on the x-axis and standardized bivariate reactance indexed to height (zXc/h) on the y-axis. The vector in the left lower quadrant beyond the 75th tolerance ellipse was defined as OH by BIVA. The figure depicts the change in hydration status among the three patients who were OH by BIVA at baseline (diamond). The hydration status at follow-up (within three months) is represented by a triangle. Patient 1 (blue) had an improvement in hydration status at follow-up (lengthening of vector moved within the 75th tolerance ellipse), while patient 2 (red) and patient 3 (grey) continued to remain overhydrated (beyond the 75th tolerance ellipse). No significant vector displacement at follow-up was noted (T2: 1.5).
Modification to treatment was seen in nine (60%), based on the clinician’s judgment, of whom all had a change in CAPD prescription (change in the concentration of CAPD fluid from 1.5% to 2.5% and shortened cycles in five, addition of icodextrin in four) while only one had a change in antihypertension medications (increased dose of enalapril).
In those who had a modification to treatment made, six (67%) showed improvement in OH status while only one (11%) demonstrated well-controlled ambulatory hypertension. In the overall cohort at follow-up, the reduction in OH-BIVA was 33.3% and OH-LU was 40%, while reduction in UH was in 18% of children.
Association between OH-BIVA or OH-LU and UH
There was no significant association between OH and UH at baseline or follow-up [OH-BIVA and UH (20% vs 73%, p = 0.23; 13% vs 60%, p = 0.5, respectively), OH-LU and UH (33.3% vs 73%, p = 0.34; 20% vs 60% p = 0.4, respectively)].
Discussion
Identifying bedside tools to detect subclinical OH and studying the association of OH with UH is critical in children on dialysis. This prospective study in children on CAPD showed that OH and UH were frequently encountered. There was no significant association between OH-BIVA or OH-LU with UH at baseline and short-term follow-up (three months).
In children on CPD, OH is a hidden and pervasive complication and appropriate volume control is one of the key goals of therapy.4-6 The key component of an effective dialysis prescription is defining the target weight, which is a challenging task as clinical assessment of OH is often inaccurate and unreliable.5,22 There is strong evidence to support the use of BIA and LU for assessment of hydration status in adult dialysis patients.23-27 The newer bioimpedance device, BIS, has been studied in children on dialysis and demonstrated valuable in detecting OH.14,28,29 However, BIVA is more cost effective and easily available compared to BIS. The other advantages of BIVA include the ability to pictorially track hydration and nutrition status, perform measurements with minimal training and negligible interobserver difference.9,16,30 In adults on maintenance dialysis, the role of BIVA to guide prescriptions to reduce OH has been validated, including in the Indian population.31,32 There is limited data available on BIVA in children on dialysis. The lack of specific reference graphs may also hinder the correct interpretation of BIVA in children. In previous studies from our center, BIVA aided in targeting dry weight in children on HD and reflected OH better than the clinical assessment in children on CAPD.33,34
Subclinical OH is known to improve patient’s quality of life and long-term cardiovascular outcomes.2,35 In this study, both BIVA and LU detected subclinical OH. In addition, the creation of more robust reference graphs helped in assessing and tracking hydration status, highlighting the utility of BIVA as a valuable bedside tool to target dry weight in children on HD and CPD. The discrepancies in the prevalence of OH identified by BIVA and LU could be attributed to the difference in body compartments analyzed.5,6 Thus, the information provided by combining these tools should be considered complementary to clinical signs in the assessment of hydration status.
There was a lack of association between OH and UH in children on CAPD. UH is associated with left ventricular hypertrophy and cardiac dysfunction, which contributes to poor patient outcomes.36 The commonly practiced “volume first strategy” of managing hypertension may not be beneficial in all, as BP measurements are not solely determined by intravascular volume. Targeting dry weight based on BP control also carries the risk of aggressive and unjustified ultrafiltration, leading to intradialytic hypotension, loss of RKF, and myocardial stunning.4 In this study, despite improvement in OH at follow-up, a majority continued to have UH, suggesting that other causes of hypertension need to be explored. The multifactorial etiology of hypertension in children on dialysis include volume-independent factors such as vascular stiffness, congestive heart failure, underlying kidney disease, sympathetic overactivity, and the involvement of renin-angiotensin-aldosterone system.
Similar findings of lack of association between OH and UH in dialysis patients have been reported earlier. In a study of 639 adult APD patients, van Biesen et al. noted that 30–40% had systolic hypertension, despite normo-or underhydration.37 Only a few studies have investigated the association between OH and hypertension in the pediatric dialysis population. In a study by Zaloszyc et al. of 23 children on chronic HD, hypertension (clinic BPs >95th percentile) was seen in 45.3% with normal hydration (by BIS) and BP normalized in only 50% of them following dialysis.1 Allinovi et al. reported that among13 children on dialysis (eight on APD), hypertension (clinic BPs >95th centile) diagnosed in 36% was not associated with OH (BIS and LU).6 Eng et al. observed that 25% of high BP measurements (clinic SBP >90th percentile) were not accompanied by OH (BIS) in their study of 20 children on dialysis (ten on APD).4 More recent studies have also shown similar results.14,38
Our study has notable strengths. The creation of unique gender-specific reference BIVA graphs from healthy controls is one of the highlights. This is also the only study reported in children on dialysis where the gold standard technique of ABPM was used to study the association between hypertension and OH. Interobserver bias was avoided as only a single trained researcher performed all measurements of BIVA and LU. Limitations of the study included small sample size, the nonuniform follow-up due to the pandemic phase, absence of echocardiographic assessment, and lack of analysis of other factors affecting ambulatory hypertension like salt intake and type of antihypertensive medication.
In conclusion, this prospective study in children with kidney failure on CAPD indicates that subclinical OH and UH are frequently detected. However, UH is not associated with OH-BIVA or OH-LU. Besides OH, other etiological factors like excess dietary sodium intake, vascular stiffness, and renin-angiotensin-aldosterone system overactivation for UH need to be explored in these children to ensure optimal management.
Acknowledgments
We thank all the patients for their participation in the study. We would also like to thank Navajbai Sir Ratan Tata trust, Mumbai, for providing an educational grant to undertake this study.
Conflicts of interest
There are no conflicts of interest.
References
- Hydration measurement by bioimpedance spectroscopy and blood pressure management in children on hemodialysis. Pediatr Nephrol. 2013;28:2169-77.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiovascular disease in children with chronic kidney disease. J Am Soc Nephrol. 2012;23:578-85.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The interdialytic weight gain: A simple marker of left ventricular hypertrophy in children on chronic haemodialysis. Pediatr Nephrol. 2015;30:859-63.
- [CrossRef] [PubMed] [Google Scholar]
- Assessing the hydration status of children with chronic kidney disease and on dialysis: A comparison of techniques. Nephrol Dial Transplant. 2018;33:847-55.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment and management of fluid overload in children on dialysis. Pediatr Nephrol. 2019;34:233-42.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Finding covert fluid: Methods for detecting volume overload in children on dialysis. Pediatr Nephrol. 2016;31:2327-35.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Assessment of hydration status in peritoneal dialysis patients: Validity, prognostic value, strengths, and limitations of available techniques. Am J Nephrol. 2020;51:589-612.
- [CrossRef] [PubMed] [Google Scholar]
- Bioimpedance-guided monitoring of volume status in patients with kidney disease: A systematic review and meta-Analysis. Can J Kidney Health Dis.. 2023;10
- [CrossRef] [Google Scholar]
- Combined evaluation of nutrition and hydration in dialysis patients with bioelectrical impedance vector analysis (BIVA) Clin Nutr. 2014;33:673-7.
- [CrossRef] [PubMed] [Google Scholar]
- Classification of hydration in clinical conditions: Indirect and direct approaches using bioimpedance. Nutrients. 2019;11:809.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Bio-electrical impedance vector analysis: Testing Piccoli’s model against objective body composition data in children and adolescents. Eur J Clin Nutr. 2019;73:887-95.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Chronic Kidney Disease (CKD): An observational study of etiology, severity and burden of comorbidities. Indian J Pediatr. 2017;84:822-5.
- [CrossRef] [PubMed] [Google Scholar]
- Role of twenty-four-hour ambulatory blood pressure monitoring in children on dialysis. Clin J Am Soc Nephrol. 2011;6:870-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Tracking hydration status changes by bioimpedance spectroscopy in children on peritoneal dialysis. Perit Dial Int. 2021;41:217-25.
- [CrossRef] [PubMed] [Google Scholar]
- Bioelectrical impedance analysis in body composition measurement: National Institutes of Health Technology Assessment Conference Statement. Am J Clin Nutr. 1996;64:524S-532S.
- [CrossRef] [PubMed] [Google Scholar]
- Bioelectrical impedance vector analysis to evaluate relative hydration status. Pediatr Nephrol. 2010;25:329-34.
- [CrossRef] [PubMed] [Google Scholar]
- Estimation of fluid volumes in hemodialysis patients: Comparing bioimpedance with isotopic and dilution methods. Kidney Int. 2014;85:738-41.
- [CrossRef] [PubMed] [Google Scholar]
- Lung ultrasound: A novel technique for detecting fluid overload in children on dialysis. Nephrol Dial Transplant. 2017;32:541-7.
- [CrossRef] [PubMed] [Google Scholar]
- B-lines on pediatric lung sonography: comparison with computed tomography. J Ultrasound Med. 2016;35:153-7.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140:e20171904.
- [CrossRef] [PubMed] [Google Scholar]
- Ambulatory blood pressure monitoring in children and adolescents: 2022 update: A scientific statement from the American Heart Association. Hypertension. 2022;79:e114-24.
- [CrossRef] [PubMed] [Google Scholar]
- Dialysis: Bioimpedance spectroscopy for assessment of fluid overload. Nat Rev Nephrol. 2013;9:252-4.
- [CrossRef] [PubMed] [Google Scholar]
- Bioimpedance indices of fluid overload and cardiorenal outcomes in heart failure and chronic kidney disease: A systematic review. J Card Fail. 2022;28:1628-41.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Baseline hydration status in incident peritoneal dialysis patients: The initiative of patient outcomes in dialysis (IPOD-PD study)†. Nephrol Dial Transplant. 2015;30:849-58.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Lung ultrasound as a tool to evaluate fluid accumulation in dialysis patients. Kidney Blood Press Res. 2022;47:163-76.
- [CrossRef] [PubMed] [Google Scholar]
- A randomized multicenter trial on a lung ultrasound-guided treatment strategy in patients on chronic hemodialysis with high cardiovascular risk. Kidney Int. 2021;100:1325-33.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of lung ultrasound and other volumetric methods in peritoneal dialysis patients. Medicine (Baltimore). 2021;100:e23856.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Fluid balance assessment in pediatric hemodialysis patients by using whole-body bioimpedance spectroscopy (WB-BIS) Pediatr Nephrol. 2022;37:2449-56.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Application of bioelectrical impedance analysis in nutritional management of patients with chronic kidney disease. Nutrients. 2023;15:3941.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Bioelectrical impedance vector analysis in obese and overweight children. PLoS One. 2019;14:e0211148.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Bioelectrical impedance analysis measures and clinical outcomes in CKD. Am J Kidney Dis. 2018;72:662-72.
- [CrossRef] [PubMed] [Google Scholar]
- Body composition analysis with bioelectric impedance in adult Indians with ESRD: Comparison with healthy population. Kidney Int. 2006;69:1649-53.
- [CrossRef] [PubMed] [Google Scholar]
- Targetting dry weight of children on maintenance dialysis by bio-impedance analysis. Asian J Pediatr Nephrol.. 2019;2:54-55.
- [Google Scholar]
- Assessment of overhydration in children on continuous ambulatory peritoneal dialysis by Bioimpedance Vector Analysis-A longitudinal observational study. Kidney Int Rep.. 2021;6:S286.
- [Google Scholar]
- Bioimpedance in CKD: An untapped resource? Nephrol Dial Transplant. 2023;38:583-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Blood pressure management in children on dialysis. Pediatr Nephrol.. 2018;33(2)::239--50.
- [CrossRef] [PubMed] [Google Scholar]
- Fluid status in peritoneal dialysis patients: The European body composition monitoring (EuroBCM) study cohort. PLoS One. 2011;6:e17148.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The value of bioimpedance analysis in the assessment of hydration and nutritional status in children on chronic peritoneal dialysis. Ren Fail. 2024;46:2301531.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







