Translate this page into:
Prosthetic Hemodialysis Access-induced Distal Hand Ischemia and its Contributors in Diabetics
Address for correspondence: Dr. S. M. Alamshah, Department of Vascular Surgery and Trauma and Transplantation, Golestan Hospital, Ahvaz, Iran. E-mail: alamshah-sm@ajums.ac.ir
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Avoidance of hand ischemia in the construction of prosthetic access for hemodialysis in diabetics that have no suitable vein for arteriovenous fistula is appreciated. Taper type may be an appropriately matched conduit to prevent its occurrence. This is a prospective controlled trial of 38 selected diabetics requiring hemodialysis, who were referred to our clinic during a period of 6 months. The aim of the study was to evaluate the efficacy of tapered grafts in preventing distal hand hypoperfusion and determining its most likely contributors. In 18 intervening cases, taper 4 mm × 7 mm and in twenty cases (control group), standard 6 mm polytetrafluoroethylene as straight Brachial-Axillary access was used. Graft flow rates, artery and vein diameters, and mean arterial pressure were included for evaluation. Within the control group, 11 patients (55%) (7 cases Grade 1, 3 Grade 2, 1 Grade 3) and in intervening group, 2 cases (11%) (Grade 1, Grade 3) developed Steal syndrome. There was no significant difference in the mean flow rates (P = 0.82). Increased risk of distal hypoperfusion was observed in the control group when flow rates were more than 1000 ml/min. Arterial diameters (P = 0.011) and mean arterial pressure (P = 0.05) were found to be important contributing factors. Taper grafts causes reduced incidence of distal hand hypoperfusion. When artery diameter was <6 mm and mean arterial pressure lower than 100 mmHg and the index (brachial artery diameter × mean arterial pressure) was under 500, distal hand ischemia occurred in standard and tapper type. We therefore recommend selective usage of taper grafts in diabetics with diminished distal hand pulses, considering the contributing factors when fistula first is not feasible.
Keywords
Brachial-axillary arteriovenous graft
diabetes
hemodialysis access-induced distal hand ischemia
steal syndrome
tapered graft
Introduction
Since the recommendation of taper type of expanded polytetrafluoroethylene (ePTFE) as a new modality with crucial supporting properties on hemodynamic and flow rate of accesses for dialysis,[1] few studies investigated its efficacy in reducing the risk of hemodialysis access-inducing distal hand ischemia (HAIDI) in diabetics. Simultaneous application of standard ePTFE and its taper kind for comparison is also rare. Those that exist, neither have demonstrated the role of the taper grafts in high-risk patients notably “diabetics,” nor determined their predisposing factors implicated in access producing steal syndrome. In construction of an effective access, brief studies have obtained useful results, but they have more evidently focused on autogenous arteriovenous fistulas (AVF). Fistula first principle has to be followed as far as possible. AV grafts should be reserved only in specific cases, and these should be done by experienced surgeons. Diabetic patients occasionally cannot tolerate long hours of dialysis due to extremity pain; however, without dialysis, patients may face–hand rest pain, defective fingers movement, nail cyanosis, and further numbness. The majority of these are shown to be due to hypoperfusion, which in the existence of previous satisfactory distal hand pulses is referred to as steal phenomenon; though now, there is advocacy that the steal may be a misnomer. On the other hand, in spite of selective application of arteriovenous grafts (AVGs), sometimes, problematic extremities present with distal circulatory deficits due to the impaired arterial flow that can lead to severe pain or even irreparable ischemia. In such circumstances, the choice could either be lower extremity vascular access or utilizing long lasting cuffed catheters. Thus, it is necessary to consider the effective selection, especially in diabetics, old patients and who sustained severe peripheral vascular disease accompanied by distal circulatory deficit, arterial strictures, neuropathy, or concomitant myopathy. This study was aimed to evaluate and compare HAIDI occurrence in diabetics who had taper and standard ePTFE graft used for their accesses, considering the existence of their distal pulses and focused to determine its contributing factors.
Materials and Methods
This was a prospective controlled trial containing 38 diabetic patients with end stage renal disease (ESRD). Patients lacked suitable veins for AVF and were all candidates for construction of prosthetic AVG for hemodialysis. Patients were referred to our vascular surgery department of Golestan hospital affiliated to Ahwaz Jundishapur University of Medical Sciences, Ahwaz, Iran. The duration of the study was from January 2013 to June 2013. The aims of the trial were to evaluate the efficacy of tapered grafts in preventing HAIDI and also to identify the most likely contributing factors during their primary patency. The trial was registered in Iranian Clinical Trials, No: IRCT 2013041212993N1. The main subject of the research article as a thesis has been approved by institutional research and ethical committee of Jundishapur medical faculty No: D/552. All patients gave their written informed consent prior to the commencement of the study. Inclusion criteria were diabetic patients with clinically nonocclusive upper extremity arterial status and acceptable good radial pulses with approved motor-sensory examinations that had no suitable superficial vein bilaterally for the construction of AVF and, therefore, were the candidate for prosthetic brachial-axillary AVG. Exclusion criteria were pulseless diabetics, history of hand or forearm trauma, orthopedic surgery on forearm and wrist and candidates for placement of AVF as the first line and grafts in lower extremities. Patients were routinely selected by accurate clinical examination that was able to demonstrate good projection of dominant veins and for others who clinically were not clear, including the obese and previous thrombosed AVF, venous mapping with color Doppler was used to confirm their lack of suitable venous mapping and rejecting AVF construction. From 38 cases that were entered into the study, twenty patients were control group in whom straight standard 6 mm ePTFE were used with the mean age of 59.3 years (42–84), 13 (65%) female and 7 (35%) male. Other intervening group was 18 patients in whom short taper ePTFE 4 mm × 7 mm grafts were used with the mean age of 56.06 years (31–79), 12 (66%) female and 6 (34%) male. Straight standard 6 mm and short taper 4 mm × 7 mm AVG were constructed individually and one by one intermittently at random. Similarly, up to 7 mm arterial orifices for arterial-graft anastomosis and at least 4–5 cm length for tapering distance were considered. All the grafts were provided in their non-dominant arm in the form that grafts were over sewn to brachial artery in above the elbow crease (cubital fossa) and axillary vein in the beginning of sub axillary fossa, by a vascular surgeon. Diameters of brachial arteries and axillary veins were measured by using metallic sterile bi-side pin compass and a concomitant metallic sterile ruler before any releasing to avoid vessel spasm. The mean arterial pressure was checked during the operation and recorded. In recovery room, the flow rate in proximal and distal side of grafts were measured and recorded by portable digital color Doppler ultrasound, SonoScape S6 machine and by the same operator in all patients. The next day and then on daily basis, all the patients were re-examined for any symptom or sign of distal hand hypoperfusion until they were discharged. We have used arterial site compression test clinically for determining any steal producing pulselessness for hand ischemia, if it was presented by the patients. The mild to moderate ischemic presentation was followed until recovery along with finger exercise or any further requiring open surgical (drill procedure) or percutaneous interfering repair up to primary patency period. In the 2nd week post-construction, patients started hemodialysis from grafts with permission. The recorded data and results were statistically analyzed and interpreted by SPSS version 20.0 (IBM, Armonk, NY, USA).
Results
All patients had diabetic kidney disease as the cause of ESRD and had good radial pulses. Some had history of ischemic heart disease, hypertension, stroke, intermittent claudication and neuropathy, and a few cases had distal hand muscle atrophy. Results of comparing the two groups are depicted in Table 1.

Eleven patients (55%) from control group (standard graft) eventually developed HAIDI. Seven cases (35%) were mild form (Grade 1), 3 (15%) moderate (Grade 2), and 1 (5%) severe (Grade 3) that warranted intervention for limb salvage by DRIL procedure. Within the 18 cases of trial group (tapered graft), only two cases (11%) developed steal, one of them in the Grade 1, and the other in Grade 3 who also was repaired by DRIL operation. No percutaneous intervention was performed.
The mean outgoing blood flow rate of graft circulation was 973.25 ml/min (560–1550) in control standard group and 992.35 ml/min (550–1600) in taper graft group, respectively. There was also an increased risk of hand ischemia in flow rates higher than 1000 ml/min in control group, which was not observed in the taper group; however, this effect did not reach statistical significance (P = 0.82) [Figure 1]. Although similar, high flow rates are associated with increased risks of cardiac complications, the observed high flow rate did not cause any such effects. Of note, cardiac complications are not usually produced in flow rates <1500–1700 cc/min in normo-cardiac uremic patients unless in previously cardiac myopathic involvement or severe uremic lungs and hearts and elongates years for new dialysis patients to present.
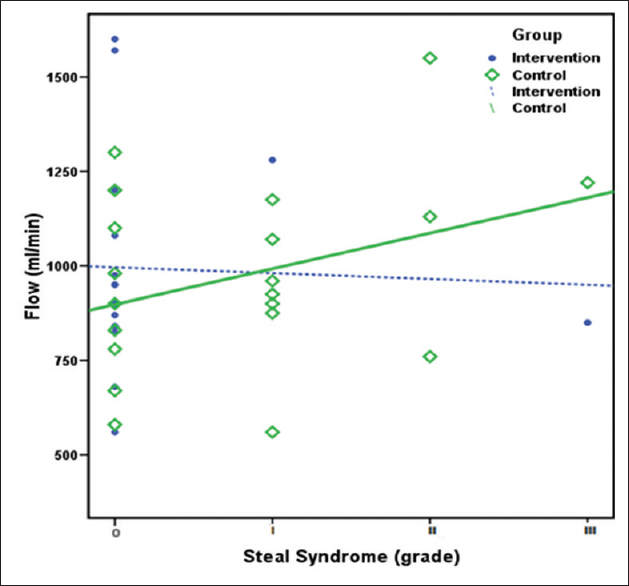
- Correlation between flow rate and hemodialysis access-inducing distal hand ischemia risk. Has shown that in standard 6 mm graft and in parallel to flow rate of 1000 ml/min and above, hemodialysis access-inducing distal hand ischemia by access is highly probable depending on the incidence of steal category (P = 0.82). Taper grafts did not correlate this range in the chart. Correlation between intervention group (n = 18) and controlled group (n = 20)
According to the measurements of brachial arteries and axillary veins, the mean diameter of brachial arteries was 5.35 mm (4–8) and 4.55 mm (3–6) in the control and taper groups, respectively. Interestingly, statistically significant increased risk of HAIDI was found in arterial diameter <6 mm in standard control group (P = 0.011). However, this was not observed in intervening taper group [Figure 2].
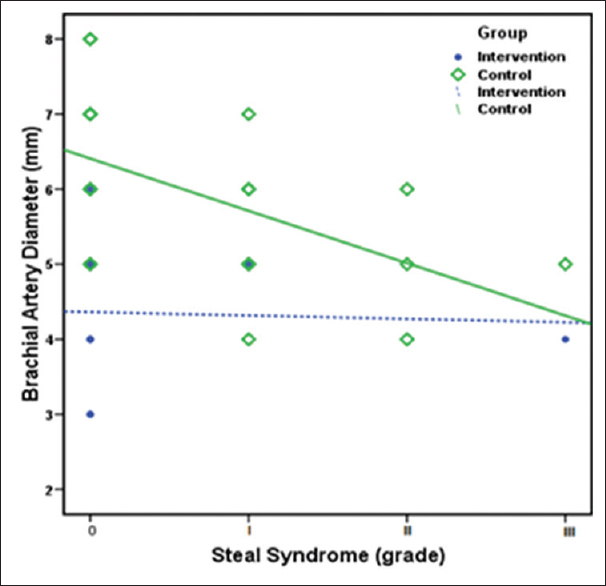
- Correlation between brachial artery diameters and hemodialysis access-inducing distal hand ischemia occurrence. Hemodialysis access-inducing distal hand ischemia is shown to produce in relation to the diameter of brachial artery above 4.4 mm, but is more prevalent in control group about 5 mm and under 6 mm (P = 0.011), Taper group did not show Steal-induced hemodialysis access-inducing distal hand ischemia. Intervention group (n = 18) control group (n = 20)
The mean diameter of axillary vein before and after the venous valve was 7.40 mm in control group and 6.76 mm in the taper group. There was no correlation between the aforementioned diameters and HAIDI.
The mean arterial pressure was 101.60 mmHg (70–140) for control patients and 112.76 mmHg (78–133) for constructed taper grafts. Analysis has shown a significant increase in risk of HAIDI (P = 0.050) with mean arterial pressure lower than 100 mmHg in both groups [Figure 3].

- Correlation between mean arterial pressures and hemodialysis access-inducing distal hand ischemia occurrence. The beginning of hemodialysis access-inducing distal hand ischemia is shown to be about 110 mmHg and hemodialysis access-inducing distal hand ischemia is more producing under it. According to the chart, statistically significant increase in hemodialysis access-inducing distal hand ischemia is seen below 100 mmHg (P = 0.050)
Since both brachial artery diameters and mean arterial pressure have reverse correlation with the risk of hand ischemia, we used multiplication of these two parameters as a new suggested index and found that this index predicted statistically significant correlation with the risk of HAIDI occurrence (P = 0.05). If millimeters were used for the diameter and mmHg for the pressure, the threshold of significant HAIDI will be approximately “600” for standard 6 mm diameter and “500” for tapered 4 × 7 grafts, [Figure 4].

- Correlation of hemodialysis access-inducing distal hand ischemia with the produced index. Index = (brachial artery diameter) × (mean arterial pressure). The produced index explains the existence of hemodialysis access inducing distal hand ischemia that was ranged 300–800. Most prevalent <600 for control group and <500 for taper intervening group. In the presence of indexes lower than 500, hemodialysis access-inducing distal hand ischemia is shown to be certain depending on the incidence of Steal category (mild, moderate, severe) (P = 0.05)
There were no correlations between other demographic parameters such as sex, age, radial pulse existence, severity or the duration of involving diabetes, hypertension, ischemic heart disease, previous stroke, and intermittent claudication with developing HAIDI in the study. Long-term patency and risk of thrombosis were not evaluated in this study.
Discussion
HAIDI is caused by multi-factorial complex phenomena. Some of its causes have been recognized in literature. Utilizing synthetic grafts;[2] old age patients, especially those with large bores graft access;[34] autogenous upper arm brachial-based AVFs in late chronic phase;[45] diabetes ground;[23] reduction in forearm arterial blood and bed pressure by high outflow exhaust through the graft or physically, turbulent flow at the arteriovenous anastomosis site;[678] side venous branches in AVFs;[8] severe peripheral arterial disease;[589] preoperative high digital-brachial index (DBI <0.45–1.0),[5610] and iatrogenic occurrence [11] are all previously known contributing factors for Steal development. The incidence of symptomatic Steal with hand ischemia ranges from 0.5% up to 28%.[3479] Based on geometry and physiologic causes, mean access flow, mean arterial pressure, and digital-brachial index may also be implicated in Steal syndrome. On the other hand, multiple native interfering parameters may accelerate Steal producing with hand ischemia and fix it as a progressive syndrome. Accordingly, loss of propagating circulatory stream, overwhelming thrombosis induced by hypercoagulable state, and low arterial pressures due to severity of atherosclerosis in diabetic patients have been accounted. Diabetics, who suffer from ESRD and require vascular access for hemodialysis, characteristically, possess these susceptibilities. To handle these propensities, close clinical management and practical procedure individualization are required. Presumably now, presence of hand ischemia in patients is correctly being handled by selecting the procedure, and the technique besides predicting its probability that provoke less complications and succeeding in more efficient access constructions. Clinical selection and physical examination are enough for the risk prediction in all patients; since, competent studies have shown minor contradictions in their findings. Nonsignificant and similar geometric results in comparisons,[1213] wide range of DBI with lack of definite threshold even for inevitability [5610] and overall, inexistence of certain acceptable index for accurate case selection, are the examples.
According to our findings, in diabetic group with taper access, the flow rates were identical in comparison with control standard grafts, similar to attained results of Van Tricht et al., expressing that the taper distance did not affect the flow. Furthermore, acquired significant efficacy of taper graft to prevent Steal complication (11%, compared to 55% overall incidence in standard type) demonstrates its preference to standard type in our cases. In conformity to literature, presumably, “tapered distance” possesses a considerable physical property to block the establishment of turbulent flow in proximal anastomosis compared to standard type. Moreover, it has been postulated that appropriate tapering of graft diameter in constructing an access is able to reduce higher pressure at the narrow segment of arterial side anastomosis and abolish the turbulent anastomotic vortex which is responsible for both high pressure arterial flow outgoing and low pressure distal circulation defined as Steal syndrome.[112] Having considered this issue, Van Tricht et al. have also shown that the pressure drop at the arterial anastomosis site of tapered 4 mm × 7 mm graft, is three times higher than in 6 mm straight graft model in spite of no statistically significant differences between geometries. Concomitantly, Krueger et al. have shown a statistically significant reduction in flow rate up to 28% in 4 mm and up to 55% in 3 mm of narrow segments. Upon these facts, the acceptance of taper graft efficiency for controlling the Steal syndrome and producing HAIDI, have been confirmed.
Nevertheless, according to statistical analysis, we believe that all the above-mentioned explanations are not purely denoting on tapered zone as demonstrated by further correlations between Steal and the diameters of brachial arteries and the mean arterial pressure that were achieved within control group. These findings can be interpreted as Steal contributing factors that with the existence of narrow artery of <6 mm, arterial pressure <100 mmHg, and flow rate more than 1000 ml/min, the steal concomitant with distal hand ischemia would be mostly possible. Hence, based on correlations, the achieved mean brachial artery diameter (5.35 mm) in control group of standard grafts might account a relevant contributor for the high rate of 55% steal occurrence with 35% Grade 1, and the two other cases of Grade 3 in both groups in spite of identical arterial orifice for anastomosis. Of note, in taper group, there was no such statistical difference. However, we believe one exception exist against the low diameter effect on producing Steal syndrome. That is the anatomically bifurcated brachial artery in upper arm. Although in patients with divided artery in upper arm diameter of branches may be < 5–6 mm, to have confidence that both distal arteries are palpable or their circulation are being confirmed by Allen's test, HAIDI will not be expected to occur.
Totally, although we believe that taper type graft was useful in preventing HAIDI occurrence in our selected diabetic cases, we do not advocate free usage of this type of grafts in all nondiabetic population demanding prosthetic dialysis access or other diabetics who have normal distal hand arteries and pulses, since the early outcomes of two kinds of grafts in our study and also secondary late outcome in others were similar.[1213] On the other hand, most of nondiabetic or diabetic patients with normal pulse do not develop hand ischemia or may experience mild form (Grade 1), which resolves spontaneously.
Consequently, based on our observations, we recommend that tapered grafts could be an ideal access in selected diabetic patients who have diminished distal pulses or narrow brachial artery, otherwise standard grafts may be utilized. Generally, we warn if in diabetic patients brachial artery is narrower than 6 mm, mean arterial pressure is lower than 100 mmHg and if the index: “the multiply of diameter to pressure” is below than 500; then, utilizing any type of grafts may produce mild to perhaps more severe HAIDI. Whereas in patients with index value >500, the risk of threatening or significant ischemia is low and any kind of standard grafts may be safely used. Available Doppler is the accepted method and a complement for the evaluation of population with renal insufficiency, especially diabetics before any access construction.
Our studies offer alternative strategy in treating diabetics with secondary vascular complications. Diabetes is a major cause of death worldwide that is associated with secondary health complications. The incidents of diabetes are rapidly increasing worldwide, and the rates are particularly high in the Middle East and South Asia. Our observations were made within a cohort of Iranian patients population. However, this research outcome can directly be implemented in existing Indian patient population suffering from complications associated with diabetes and provide alternative strategies in clinical care in patients with specific vascular implications. Without any limitation, further investigations with larger populations and long-term follow-up are recommended to support our findings and find the new correlations.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank M. Mousavi MD, general surgeon, the fellow of our vascular department and also Ms. M. Seyedtabib, specialist in statistics, for her kind cooperation and support.
References
- Effect of tapered grafts on hemodynamics and flow rate in dialysis access grafts. Artif Organs. 2004;28:623-8.
- [Google Scholar]
- Time of onset in haemodialysis access-induced distal ischaemia (HAIDI) is related to the access type. Nephrol Dial Transplant. 2009;24:3198-204.
- [Google Scholar]
- Upper arm polytetrafluoroethylene grafts for dialysis access. Analysis of two different graft sizes: 6 mm and 6-8 mm. Vasc Endovascular Surg. 2003;37:335-43.
- [Google Scholar]
- Prospective evaluation of ischemia in brachial-basilic and forearm prosthetic arteriovenous fistulas for hemodialysis. Eur J Vasc Endovasc Surg. 2008;35:619-24.
- [Google Scholar]
- Steal in hemodialysis patients depends on type of vascular access. Eur J Vasc Endovasc Surg. 2006;32:710-7.
- [Google Scholar]
- Blood flow dynamics in patients with hemodialysis access-induced hand ischemia. J Vasc Surg. 2013;58:446-51.e1.
- [Google Scholar]
- Management of steal syndrome resulting from dialysis access. Semin Vasc Surg. 2004;17:45-9.
- [Google Scholar]
- Haemodialysis access-induced distal ischaemia (HAIDI) is caused by loco-regional hypotension but not by steal. Eur J Vasc Endovasc Surg. 2012;43:218-23.
- [Google Scholar]
- Incidence and characteristics of patients with hand ischemia after a hemodialysis access procedure. J Surg Res. 1998;74:8-10.
- [Google Scholar]
- Strategies for predicting and treating access induced ischemic steal syndrome. Eur J Vasc Endovasc Surg. 2006;32:309-15.
- [Google Scholar]
- Hemodynamics in a compliant hydraulic in vitro model of straight versus tapered PTFE arteriovenous graft. J Surg Res. 2004;116:297-304.
- [Google Scholar]
- Evaluation of 4-mm to 7-mm versus 6-mm prosthetic brachial-antecubital forearm loop access for hemodialysis: Results of a randomized multicenter clinical trial. J Vasc Surg. 2003;37:143-8.
- [Google Scholar]







