Translate this page into:
Rare Cause of Bright Red Gross Hematuria in a Child
Address for correspondence: Dr. G. Kumar, Division of Pediatric Nephrology, Sheikh Khalifa Medical City, Abu Dhabi, UAE. E-mail: kumargurinder@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Dear Sir,
A 12-year-old male child, product of nonconsanguineous marriage was referred to us with complaints of red colored urine with fresh clots and generalized body aches of 3 days duration. There was no history of drug use, trauma, or bleeding from any other site.
A significant history included Burkitt Lymphoma, which was diagnosed at the age of 2 years elsewhere, and he was treated with chemotherapy (details not available). Subsequently, he developed ataxic gait and tremors from the age of 3 years. This was attributed to side effects of chemotherapy and not investigated further. He was bed ridden after that. There was a history of chronic redness of eyes and non-purulent discharge on and off. His clinical examination revealed a malnourished child with severe pallor. He was normotensive and had normal renal functions and electrolytes. Complement levels were normal. He had severe anemia with reticulocytosis, and glucose-6-phosphate dehydrogenase enzyme was deficient. Coagulation profile was normal. Urine culture was sterile. There was no significant proteinuria. Hemoglobin electrophoresis was normal. Hypercalciuria was ruled out. He was transfused a unit of packed red blood cell. His gross hematuria with the passage of fresh clots of urine persisted. Renal ultrasound showed normal renal sizes and there was echogenic debris in the bladder.
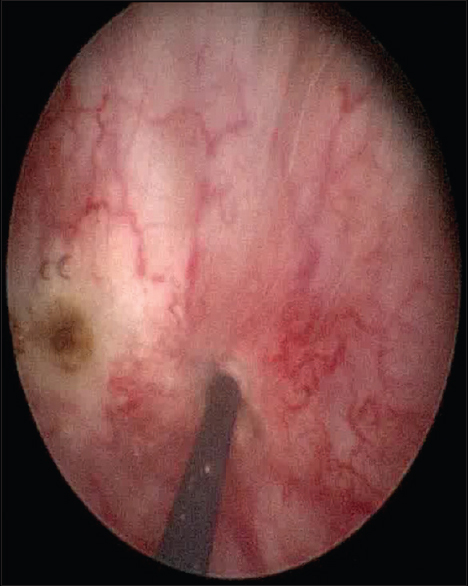
As there was fresh blood with clots, a possibility of an extra glomerular cause of bleeding was considered. Magnetic resonance imaging (MRI) abdomen ruled out Wilms tumor. Since he had a history of inability to walk with non-purulent eye discharge and redness of eyes, a differential diagnosis of ataxia telangiectasia was kept. Alpha-fetoprotein was sent and found to be high. His immunoglobulin profile showed low IgG. MRI of the brain showed cerebellar atrophy. The gross hematuria with clots persisted for 2 weeks requiring another blood transfusion. Cystoscopy was done and it showed a telangiectatic vessels in bladder mucosa [Figure 1], and diathermy was done after which the bleeding stopped [Figure 2]. On subsequent follow-ups, the child continues to have gross hematuria and has undergone 3 sessions of diathermy.

- Cystoscopic view of the bladder showing dilated vesical varices
- Diathermy procedure for bleeding vesical varices
Ataxia telangiectasia is a complex syndrome with immunologic, neurologic, endocrinologic, hepatic, and cutaneous abnormalities. Renal problems such as gross hematuria due to telangiectasias are infrequently reported. The mutated gene responsible is ataxia telangiectasia mutated gene. The most prominent clinical features are progressive cerebellar ataxia, oculocutaneous telangiectasias, chronic sinopulmonary disease, high incidence of malignancy, and variable humoral and cellular immunodeficiency. Ataxia typically becomes evident soon after these children begin to walk and progresses until they are confined to a wheel chair, usually by the age of 10–12 years, the telangiectasias develop between 3 and 6 years of age.
Gross hematuria is a common recognized event after use of antineoplastic drugs such as busulfan and cyclophosphamide therapy. It can also occur secondary to malignancy of the bladder. The patient developed severe gross hematuria requiring blood transfusion secondary to the telangiectatic blood vessels in the bladder. Suzuki et al.[1] reported a Japanese boy with hyper IgM syndrome associated with autoimmune thrombocytopenia who developed gross hematuria caused by vesical varices and telangiectasias and eventually required a surgical cystotomy. Cohen et al.[2] reported two cases of life-threatening hemorrhage from bladder telangiectasia in children with ataxia-telangiectasia who had been treated for lymphoma earlier in life, similar to our index child. Lall et al.[3] had also reported an 11-year-old girl who presented with recurrent macroscopic hematuria secondary to bladder vascular abnormalities. Literature is scarce about telangiectasias in bladder secondary to ataxia telangiectasia.
The possibility of rare conditions should be kept in mind in children with gross hematuria especially with neurologic or cutaneous abnormalities.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Vesical varices and telangiectasias in a patient with ataxia telangiectasia. Pediatr Nephrol. 2008;23:1005-8.
- [Google Scholar]
- Bladder wall telangiectasis causing life-threatening haematuria in ataxia-telangiectasia: A new observation. Acta Paediatr. 2008;97:667-9.
- [Google Scholar]
- Episodic painless hematuria of unusual etiology – A case report and review of literature. J Pediatr Surg. 2007;42:1460-2.
- [Google Scholar]






