Translate this page into:
Reduction of microalbuminuria in type-2 diabetes mellitus with angiotensin-converting enzyme inhibitor alone and with cilnidipine
Address for correspondence: Dr. Varun Kumar Singh, Department of Medicine, King George Medical University, Lucknow, Uttar Pradesh, India. E-mail: mailurvarun@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The aim of our study was to find out the antiproteinuric effect of enalapril angiotensin-converting enzyme (ACE inhibitor) alone or in combination with cilnidipine in patients with type-2 diabetes mellitus. The study was conducted on 71 patients with type-2 diabetes mellitus patients with hypertension and microalbuminuria. They were divided into two groups randomly as follows: Group I (enalaprilalone, n = 36) and Group II (enalapril with cilnidipine, n = 35). In both the groups, baseline 24 h urinary albumin was estimated and was repeated every 3 months upto 1-year. After 1-year follow-up, reduction in microalbuminuria was found to be greater in Group II. In Group I microalbuminuria came down by 25.68 ± 21.40 while in Group II it reduced by 54.88 ± 13.84 (P < 0.001). We conclude that in diabetic population, cilnidipine has an additive effect in microalbuminuria reduction over and above the well-proven effect of ACE inhibitors.
Keywords
Angiotensin-converting enzyme inhibitors
diabetic nephropathy
microalbuminuria
Introduction
Diabetic nephropathy is characterized by the onset of microalbuminuria, which progresses to overt proteinuria. Reduction of microalbuminuria leads to reduced risk of adverse renal and cardiovascular events.[1234] Angiotensin-converting enzyme (ACE) inhibitors/angiotensin II receptor blocker (ARBs) have been established to be first-line drugs in preventing the development and retarding the progress of diabetic nephropathy by reducing microalbuminuria.
Other drugs are effective in reducing proteinuria in diabetic nephropathy. Among these, cilnidipine, a unique dihydropyridine derivative 4th generation Ca2+ channel blocker has a rational pharmacological profile of dual L/N-type Ca2+ channel blocking action. It blocks L-type calcium channels in vascular smooth muscle and N-type calcium channels in sympathetic nerve terminals that supply blood vessels. In diabetic patients, there is enhanced sympathetic nervous activity resulting in constricted efferent arterioles and elevated intraglomerular pressure.[5] Unlike L-type calcium channel blockers, which cause only afferent arteriolar dilatation and increase in the intraglomerular pressure, this drug dilates both afferent and efferent arterioles by its effect on N-type calcium channels and thusreduces urinary albumin and protein excretion to a greater extent.[567]
As ACE inhibitors and cilnidipine has different mechanism of action in reducing microalbuminuria, both may be combined to get the added benefit of the two classes of drugs.
The aim of study was to compare the reduction in microalbuminuria in diabetic patients with hypertension by dividing them into two groups and keeping them under two different regimens. Group I was given enalapril (ACE inhibitor) alone and Group II was kept on combination therapy of enalapril and cilnidipine.
Materials and Methods
Study population
The present study was a randomized prospective studyin type-2 diabetic patients attending diabetic OPD, medical OPD and admitted in indoor medical wards of King George's Medical University, Lucknow over a period of 1-year (August 2013 to July 2014). Ethical clearance from the institutional ethics committee was obtained. Informed consent was obtained from all the patients before the start of study.
The patients included in the study were subjects with type 2 diabetes mellitus (age 21–70 years, either gender) with hypertension and microalbuminuria (if two out of three 24 h urinary albumin measurements are in the range of 30–300 mg/24 h during an 8-week period before entry) and have had effective glomerular filtration rate (eGFR) >60 ml/min. Microalbuminuria was measured by chemiluminescent immunoassay.
The patients with type-1 diabetes mellitus, macroalbuminuria, normal blood pressure (BP), chronic kidney disease withe GFR<60 ml/min, chronic liver disease, coronary artery disease, urinary tract infection, and pregnant and lactating women were excluded from the study. Patients were excluded could not stay on medications and were not regular on follow up.
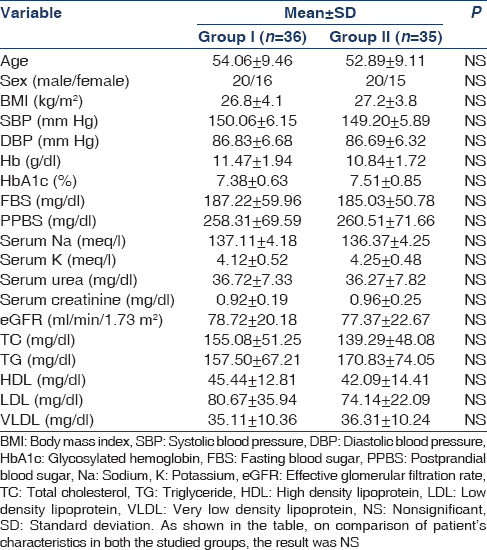
Total number of patients screened for microalbumiuria was 260. Out of these patients, 95 normoalbuminurc and 72 with overt proteinuria were excluded from the study. Out of these excluded patients, 54 patients were normotensive. Remaining 93 patients with type-2 diabetes mellitus were microalbuminuric and hypertensive. They were randomly allocated in the two groups: Group I-enalapril (n = 48) and Group II-enalapril with cilnidipine (n = 45). The baseline characteristics of the patients in the two groups are mentioned in Table 1. On comparison of characteristics in both the studied groups, the result was nonsignificant [Table 1 and Figure 1].

- Flow chart of participants through the trial
Intervention
The patients in Group I received enalapril once a day at 2.5–10 mg/day to keep the BP under 140/90. Amlodipine was needed in five patients in addition to enalaprilin Group 1 to maintain BP<140/90. In Group II, the patients were given enalapril 2.5–10 mg/day and cilnidipine 10–20 mg/day to achieve a BP below 140/90.
After the start of this trial, 12 patients withdrew from Group I and 10 patients from Group II during the course of study. The chief reason for withdrawal was noncompliance. So the total number of patients who actually went through the study was 36 in Group I and 35 in Group II. 24 h urinary albumin was repeated every 3 months upto 1-year in both the groups. At the end of 1-year, the reduction in microalbuminuria was compared in both groups. During the course of the trial, patients were observed for any adverse outcome.
Statistical analysis
The results were presented as mean ± standard deviation (SD) and percentage. Chi-square test was used to compare the dichotomous/categorical variables. The unpaired t-test was used to compare two means. One-way analysis of variance was used to detect significant differences in the mean values. P < 0.05 was considered significant. All the analysis was carried out using Statistical Package for Social Sciences version 16 (Chicago, Inc., USA).
Results
The mean 24 h urinary albumin level in Group I at the start of study was 204.69 ± 50.34 mg and in Group II was 206.74 ± 50.95 mg. At the end of 12 months, the mean microalbuminuria level was 153.17 ± 54.10 mg in Group I and 93.51 ± 36.30 mg in Group II (P < 0.001). The mean percentage reduction from baseline at the end of 12 months in Group I was −25.68 ± 21.40% while in Group II it was −54.88 ± 13.84%, (P < 0.001) [Figures 2 and 3].
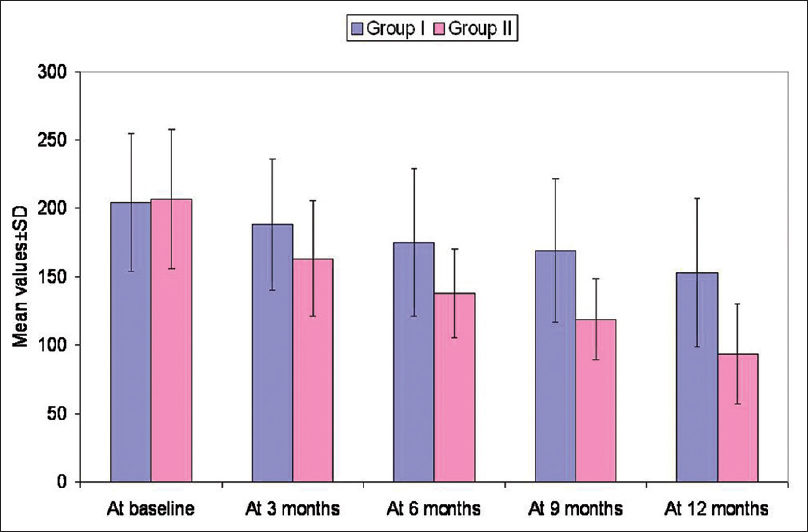
- Comparison of microalbuminuria between two groups at baseline and different follow-up intervals. Results are expressed as mean ± standard deviation. After 1-year, the level of microalbumin in Group 1 was 153.17 mm Hg while in Group 2, it was 93.51 mm Hg (P < 0.001)
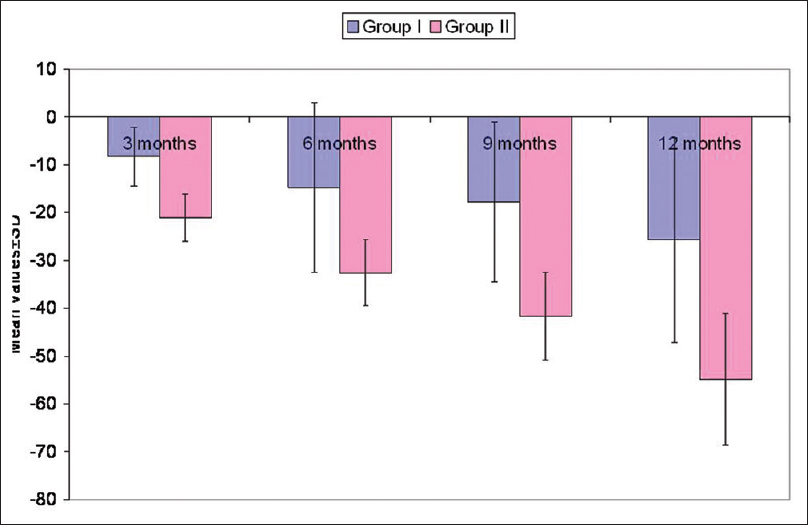
- Comparison of % change in microalbuminuria. The percentage reduction from baseline at the end of 1-year in Group II was greater than in Group I (percentage reduction of −54.88% vs. −25.68%, P < 0.001)
There was a significant reduction in systolic and diastolic B Pin both the groups from baseline to 1 year, but the difference in change of BP between Group I and Group II at different intervals was not significant. In Group I, one patient progressed to overt proteinuria while in Group II nobody progressed from microalbuminuria to overt proteinuria, although the difference was not significant. Again in Group I, only one patient became normoalbuminuric during the course of study while in Group II, it happened with three patients, although the difference was not significant. The correlation between percentage change in BP and percentage change in microalbuminuria was of random nature (P > 0.05) and showed a virtually nonexistent negligible relationship (r > 0.3) in random directions at different time intervals.
On comparison at baseline and throughout the follow-up periods, no significant difference was observed in mean systolic blood pressure levels of the two groups [Table 2].

At baseline and throughout the follow-up periods, no significant difference was observed in mean diastolic blood pressure levels of the two groups [Table 3].

There were no adverse cardiovascular events in either group [Table 4]. There were no significant changes in serum creatinine, HbA1c and serum potassium levels during the course of study between the two groups. Thedose of enalapril used in Group I was 5 ± 2.5 and 5 ± 2.1 in Group II, while thedose of cilnidipine used in Group II was 10 ± 3.

Discussion
Globally diabetes mellitus has emerged as the commonest cause of end stage renal disease. It is the etiological factor in 20–40% of all ESRD patients. Microalbuminuria (30–300 mg albumin/24 h) is a well-known predictor of poor renal outcomes in patients with type 2 diabetes.[89101112131415] Microalbuminuric patients with type 2 diabetes if left untreated, almost invariably progress to macroalbuminuria and overt diabetic nephropathy.
Although there are various classes of drugs to treat microalbuminuria, we compared monotherapy (enalapril) with combination therapy (enalapril and cilnidipine) to find out whether both are similarly effective or one is better than another in reduction of microalbuminuria. In our study, combination regimen of enalapril and cilnidipine (Group II) was more effective in reducing microalbuminuria than enalapril alone (Group I). In Group I microalbuminuria was reduced by 25.68%, while in Group II there was reduction of 54.88%, which was significant.
Katayama et al. also conducted a similar trial in patients with type II diabetes with microalbuminuria. The patients were randomized into two groups to receive either valsartan (an ARB) or valsartan plus cilnidipine for 1-year. After 1-year, microalbuminuria was found to have decreased more in the valsartan plus cilnidipine group (−44 ± 11%) than in the valsartan group (−9 ± 7%).[16]
The antiproteinuric action of ACE inhibitor and its superiority over L-type CCB is supported by a trial conducted by Remuzzi et al.[17] over hypertensive patients with type-2 diabetes and normal urinary albumin excretion rate. The study showed that diabetic nephropathy can be prevented by ACE inhibitor therapy and combination of ACE inhibitor with non-dihydropyridine calcium channel blocker (verapamil) does not provide any protective effect over kidney against the development of microalbuminuria.[17]
Our study while confirming ACE inhibitors as agents preventing diabetic nephropathy, also endorses a better improvement in proteinuria by using ACE inhibitor and cilnidipine (dihydropyridine L/N type calcium channel blocker) in combination than ACE inhibitor alone. Fujita et al. also supported the use of ACE inhibitor with cilnidipine rather than amlodipine. They conducted a trial over hypertensive patients with chronic kidney disease who were already receiving ACE inhibitor. They were randomly assigned to cilnidipine and amlodipine. Though the difference in reduction of BP between the two groups was not significant, patients treated with cilnidipine showed more decrease in proteinuria than those treated with amlodipine.[7] Hatta et al. also observed that in chronic kidney disease patients, cilnidipine has antihypertensive effects equivalent to amlodipine, but proteinuria was reduced by shifting from amlodipine to cilnidipine.[18] Kojima et al. also did a study in 28 proteinuric hypertensive patients. One group was kept on amlodipine and other on cilnidipine. The amlodipine group showed a significant increase in proteinuria, while the increase was suppressed in the cilnidipine group.[19] Tanaka conducted his trial in over 25 diabetic patients with hypertension who were on treatment with CCB other than cilnidipine. Medication was changed to cilnidipine, and there was a significant decrease in urinary albumin/creatinine ratio after 3 months of the new treatment.[20] Zaman and Kumari also compared the effects of cilnidipine and amlodipine over BP, heart rate, proteinuria and lipid profile in hypertensive patients. They found that both drugs significantly reduced BP. There was decrease in pulse rate, urinary protein excretion and serum triglyceride in diabetic patients in cilnidipine group.[21]
It is interesting to note that while scores of studies mentioned above including ours and many others have utilized the level of albuminuria as a determinant for progression of diabetic kidney disease and different group of drugs having antiproteinuric effect are widely studied to observe reduction in albuminuria as mark of improvement, some recent studies, including VA Nephron D and subgroup analysis of ALTITUDE trial and bardoxelone trials have shown that albuminuria is not a good surrogate marker for diabetic kidney disease.[222324] eGFR instead is suggested as a better alternative. However, these observations need large multicentric trials and their meta-analysis before questioning and writing off albuminuria, which is so far an established surrogate marker widely used presently in determining the state of progression of diabetic kidney disease in clinical practice and research.
Whether these recent developments may have some impact or not, which might be apparent in the time to come, our study focused on microalbuminuria and its levels observed after therapeutic intervention with antiproteinuric agents as determinant for progression of diabetic kidney disease. The results of our study indicate greater reduction in level of microalbuminuria by utilizing both ACE inhibitor and cilnidipine together than ACE inhibitor alone. This combination also appear to leading to greater reduction in proteinuria as compared to a combination of ARB with cilnidipine.[16] As ACE inhibitors are established agents to reduce proteinuria in type-1 diabetics, this combination therapy of ACE inhibitor (enalapril) with cilnidipine may be equally successful in hypertensive albuminuric type-1 and type-2 diabetics together.[2526] While indicating combination therapy to be better than ACE inhibitor alone, the study prefers ACE inhibitor over an ARB in combination with cilnidipine in treatment of diabetic nephropathy.
Limitations of the study
The main drawback of our study was that it was a single center, open-labeled randomized trial conducted over a small number of patients. Duration of the study was also short to comment on its cardiovascular and renal benefits.
So a large scale, multicenter, double-blind clinical trial involving a larger number of patients for a longer duration will be needed in future to evaluate the effectiveness and superiority of combination therapy over monotherapy in reduction of microalbuminuria and cardiovascular risk.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med. 2001;345:861-9.
- [Google Scholar]
- Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med. 2001;345:851-60.
- [Google Scholar]
- Irbesartan in Patients with Type Diabetes and Microalbuminuria Study Group. The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes. N Engl J Med. 2001;345:870-8.
- [Google Scholar]
- Reduction in albuminuria translates to reduction in cardiovascular events in hypertensive patients: Losartan intervention for endpoint reduction in hypertension study. Hypertension. 2005;45:198-202.
- [Google Scholar]
- Impact of type 2 diabetes mellitus on sympathetic neural mechanisms in hypertension. Circulation. 2003;108:3097-101.
- [Google Scholar]
- Renal and vascular protective effects of cilnidipine in patients with essential hypertension. J Hypertens. 2007;25:2178-83.
- [Google Scholar]
- Antiproteinuric effect of the calcium channel blocker cilnidipine added to renin-angiotensin inhibition in hypertensive patients with chronic renal disease. Kidney Int. 2007;72:1543-9.
- [Google Scholar]
- Microalbuminuria predicts clinical proteinuria and early mortality in maturity-onset diabetes. N Engl J Med. 1984;310:356-60.
- [Google Scholar]
- Microalbuminuria as a predictor of a drop in glomerular filtration rate in subjects with non-insulin-dependent diabetes mellitus and hypertension. Clin Nephrol. 1997;48:92-7.
- [Google Scholar]
- The risk of developing end-stage renal disease in patients with type 2 diabetes and nephropathy: The RENAAL study. Kidney Int. 2003;63:1499-507.
- [Google Scholar]
- Urinary albumin excretion is associated with renal functional abnormalities in a nondiabetic population. J Am Soc Nephrol. 2000;11:1882-8.
- [Google Scholar]
- Predictors of cardiovascular events in patients with type 2 diabetic nephropathy and hypertension: A case for albuminuria. Kidney Int Suppl. 2004;92:S50-5.
- [Google Scholar]
- Albuminuria and risk of cardiovascular events, death, and heart failure in diabetic and nondiabetic individuals. JAMA. 2001;286:421-6.
- [Google Scholar]
- Albuminuria, a therapeutic target for cardiovascular protection in type 2 diabetic patients with nephropathy. Circulation. 2004;110:921-7.
- [Google Scholar]
- Does albuminuria predict cardiovascular outcome on treatment with losartan versus atenolol in hypertension with left ventricular hypertrophy. A LIFE substudy? J Hypertens. 2004;22:1805-11.
- [Google Scholar]
- Comparison between valsartan and valsartan plus cilnidipine in type II diabetics with normo- and microalbuminuria. Kidney Int. 2006;70:151-6.
- [Google Scholar]
- Prevention and treatment of diabetic renal disease in type 2 diabetes: The BENEDICT study. J Am Soc Nephrol. 2006;17:S90-7.
- [Google Scholar]
- Switching to an L/N-type calcium channel blocker shows renoprotective effects in patients with chronic kidney disease: The Kyoto Cilnidipine Study. J Int Med Res. 2012;40:1417-28.
- [Google Scholar]
- Comparison between cilnidipine and amlodipine besilate with respect to proteinuria in hypertensive patients with renal diseases. Hypertens Res. 2004;27:379-85.
- [Google Scholar]
- The L/N-type calcium channel blocker, Cilnidipine, reduces heart rate and albuminuria in patients with type 2 diabetes. J Int Med Res. 2010;38:602-10.
- [Google Scholar]
- Comparison of the effects of amlodipine and cilnidipine on blood pressure, heart rate, proteinuria and lipid profile in hypertensive patients. Int J Basic Clin Pharmacol. 2013;2:160-4.
- [Google Scholar]
- Combined angiotensin inhibition for the treatment of diabetic nephropathy. N Engl J Med. 2013;369:1892-903.
- [Google Scholar]
- Rationale and trial design of Bardoxolone Methyl evaluation in patients with Chronic kidney disease and type 2 diabetes: The occurrence of renal events (BEACON) Am J Nephrol. 2013;37:212-22.
- [Google Scholar]
- Bardoxolone methyl in type 2 diabetes and stage 4 chronic kidney disease. N Engl J Med. 2013;369:2492-503.
- [Google Scholar]
- ACE Inhibitors in Diabetic Nephropathy Trialist Group. Should all patients with type 1 diabetes mellitus and microalbuminuria receive angiotensin-converting enzyme inhibitors. A meta-analysis of individual patient data? Ann Intern Med. 2001;134:370-9.
- [Google Scholar]
- Randomised controlled trial of long term efficacy of captopril on preservation of kidney function in normotensive patients with insulin dependent diabetes and microalbuminuria. BMJ. 1999;319:24-5.
- [Google Scholar]







