Translate this page into:
Risk Factors for Urinary Tract Infections in Renal Allograft Recipients: Experience of a Tertiary Care Center in Hyderabad, South India
Address for correspondence: Dr. V. Lakshmi, Department of Microbiology, Nizam's Institute of Medical Sciences, Punjagutta, Hyderabad - 500 082, Telangana, India. E-mail: lakshmi57vemu@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Renal transplantation is an effective and commonly performed procedure for end-stage renal disease. Urinary tract infections are a major cause of morbidity and mortality in renal transplant patients. As data on postrenal transplant urinary tract infections from the Indian subcontinent are limited, the present study was conducted to estimate the burden of urinary tract infections in this vulnerable group of patients. This was a prospective study on patients undergoing renal transplantation in 2014 at our tertiary hospital in South India with a follow-up of 2 years to evaluate the risk factors for urinary tract infections. The prevalence of urinary tract infections was 41.9% with a male preponderance of 76.9%. Mean age of the 31 patients was 32.4 ± 10.2 years (range: 16–55 years). Gram-negative bacilli were the most common isolates with Escherichia coli being the predominant pathogen (53.3%). All the infections occurred within 1 year of transplantation with delayed graft function (P < 0.001; confidence interval [CI]: 29.0–96.3) and prolonged hospital stay (P = 0.0281; CI: 42.1–99.6) being the significant risk factors for acquiring urinary tract infections. Carbapenemase production was noted in 33.3% of isolates and all the Gram-negative organisms isolated in the 1st month of transplantation were carbapenem-resistant (CR) E. coli. The high rate of carbapenem-resistant organisms in the early posttransplant period is a point of concern, especially with cadaver transplants. Infection control practices and catheter care need to be strictly monitored to minimize the risk for UTI in the immediate posttransplant period.
Keywords
Renal transplantation
risk factors
urinary tract infections
Introduction
Renal transplantation is an effective and commonly performed procedure for end-stage renal disease (ESRD). However, infections are a major cause for morbidity and mortality in the kidney transplant recipient. The risk of infection is influenced by net state of immunosuppression. Time to regain renal function, rejection episodes, and source of the donor kidney are other important factors.
The infection may be nosocomial or arise de novo in the recipient, reactivated latent infection or graft contamination. Among all, urinary tract infection (UTI) is the most common and accounts for 40%–50% of all infectious complications in renal transplant recipients.[12345] Around 20% of the untreated UTIs end up in pyelonephritis, carrying a subsequent risk of life-threatening urosepsis and graft loss.[67] Hence, early diagnosis and appropriate treatment of UTI are critical in renal transplant recipient. The present study seeks to determine the current burden and the various risk factors contributing to UTIs in this vulnerable group of renal transplant patients at a tertiary referral center in Southern India.
Methods
This was a prospective study on 31 patients who underwent renal transplantation in the year 2014 at Nizam's Institute of Medical Sciences. All the patients were clinically followed for the next 2 years in the Transplant Outpatient Clinic, thrice weekly for first 3 months, twice weekly for the next 3 months, once a month from 6th month to 1 year, and once in 3 months thereafter. Essentially, the study period was between January 2014 and December 2015. All the patients were on triple immunosuppression with tacrolimus, mycophenolate mofetil, and prednisolone. Cadaver transplant patients received an additional induction regimen with basiliximab on postoperative day 0 and day 4. Foley catheter was removed on the 4th postoperative day, and for patients on doubleJ stent, it was removed after 1 month.
Urine samples from patients with symptoms of fever, dysuria, urgency/frequency, and flank pain or suprapubic tenderness were sent to the Microbiology Laboratory for culture and sensitivity. Samples were inoculated on CHROMagar plates (CPS ID, bioMerieux, Marcy l'Etoile-France) and incubated overnight at 37°C. Pure growth of ≤2 organisms with a colony count ≥10,000 CFU/ml was processed further. Identification and antibiotic susceptibility testing of the bacterial isolates were performed by Automated Vitek 2 system (bioMerieux, Marcy-l'Etoile, France).
Recurrent UTI was defined as the occurrence of at least three episodes of symptomatic UTI in a 12-month period or two consecutive episodes within 6 months. Recurrent infection with the same microorganism was considered as a relapse. Reinfection is infection with a different microorganism, same microorganism in more than 1 month after treatment, or a sterile intervening culture.[8]
The statistical analysis was performed to evaluate the risk factors for UTI and the incidence of early infections using Fisher's exact test. P < 0.05 was considered statistically significant.
Results
Live donor transplants were performed in twenty patients and cadaver transplants in 11 patients. The median follow-up was 538 days (366–716). The mean age of the allograft recipients was 32.4 ± 10.2 years (range: 16–55 years), and 23 patients were male. Hypertension was documented in 30/31 (96.7%) patients. In all, 13/31 (41.9%) patients had UTI (10/23 [43.5%] males and 3/8 [37.5%] females). A single episode of UTI was recorded in 7/13 (53.8%) patients, while repeated episodes were documented in 6/13 (46.2%) patients. Of the latter, 4/6 (66.7%) patients were male with six episodes, and 2/6 (33.3%) were female with two episodes among them.
Recurrent UTI was observed in 4/13 patients; one patient had recurrent UTI with carbapenem-resistant (CR) Escherichia coli infection in the first 3 months followed by a recurrence in the 11th month, 2 patients had recurrent UTI with extended-spectrum beta-lactamase (ESBL) E. coli in the 5th, 6th and 11th, 12th months, respectively, while the other patient had recurrent UTI with ESBL Klebsiella pneumoniae in the 2nd and 5th months [Table 1]. Three patients with recurrent UTI were transplanted with cadaver kidneys, and 2/4 (50%) had delayed graft function.

Reinfection followed by a relapse was observed in two patients; both were males, transplanted with cadaver kidneys and had delayed graft function.
All the UTI episodes occurred within 1 year of transplantation with the majority of them occurring in the first 3 months (09/15; 60%) [Figure 1].
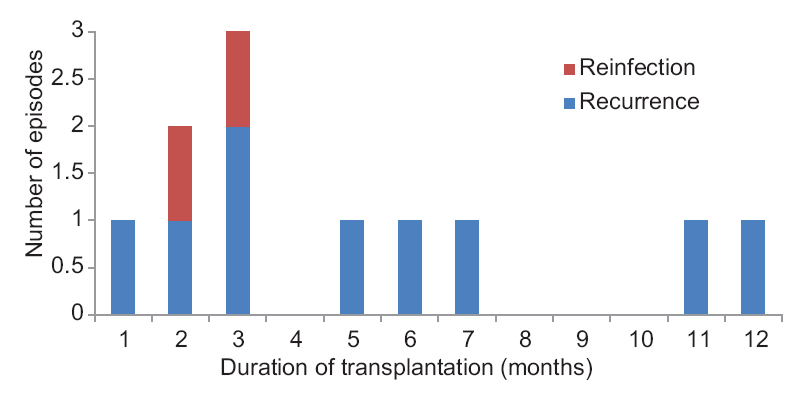
- Timeline of recurrent urinary tract infections in renal transplant patients
Gram-negative bacilli (GNB) were the most common isolates (14/15; 93.3%). ESBL production was documented in 7/15 isolates (46.6%) and carbapenem resistance in 5/15 isolates (33.3%).
E. coli was the predominant pathogen in 8/15 (53.3%) patients, of which 5/8 (62.5%) were CR and all the CR E. coli were isolated in the 1st month of transplantation (P = 0.0020; 95% CI: 1.0 [47.8–1.0]). Recurrences were recorded more in patients presenting with E. coli UTI (4/6; 66.6%).
Infections in the immediate post transplant period adversely affect graft survival, an attempt to document the likely risk factors for UTI in the first 3 months was made. Patients with UTI in the first 3 months were placed in Group I (seven patients) while rest of the 24 patients were placed in Group II [Table 2]. Delayed graft function (P < 0.001) and prolonged hospital stay (P = 0.0281) emerged as significant risk factors for UTI in the first 3 months. However, female gender and prolonged duration of dialysis before transplantation did not increase the risk of UTI. Biopsy-proven rejection was documented among all the three patients with recurrent UTI within the first 3 months.
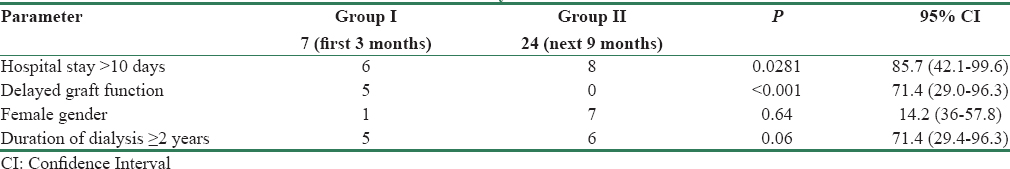
All the patients with delayed graft function (6/6; 100%) were transplanted with cadaver kidneys, with an increased risk of UTI in the first 3 months - 5/13 (71.4%). Rejection episodes were observed in 8/13 (61.5%) patients with UTI (P = 0.0209; 95% CI: 61.5 [31.5–86.1]).
Mortality rate was 4/31 (12.9%); 2 patients had a UTI, and 3 had a biopsy-proven rejection episode. Graft pyelonephritis secondary to UTI with CR E. coli was observed in one patient in the study group.
Discussion
Renal transplantation is a valuable modality of treatment for patients with ESRD. Infections remain a major setback despite significant advances in the surgical techniques and immunosuppressive drugs. UTI is the most common infection after renal transplantation and is likely to interfere with the graft function if not adequately treated.[9] Bacteria are the most common cause of postrenal transplant UTIs; fungi and viruses are less common;[1011] Gram-negative organisms were the predominant pathogens in the early posttransplant period.[1213141516]
The incidence of UTI in the present study was 41.9% and within the rates (35%–79%) reported from other centers.[11217] An earlier study from our institute reported a rate of 23.6%[2] while another Indian study documented a rate of 53%.[4] All the 15 UTI episodes occurred within one year of transplantation, as was seen in other studies[181920] and 60% of these (9/15) occurred within the first 3 months.
Documented risk factors for UTI in renal transplant patients across the world are female sex,[1213172122] old age,[1516] acute rejection,[23] cadaver donor kidney,[124] and prolonged hospital stay.[2526]
In the present study, delayed graft function was seen only in cadaver transplants and was a significant risk factor (P < 0.001) for UTI as was hospital stay of more than 10 days (P = 0.0281); similar observations were made in other studies.[25262728] Patients with rejection episodes (8/13) were more likely to have UTI (P = 0.0209; 95% CI: 61.5 [31.5–86.1]), which was similar to the observation made by Golebiewska et al., 2014. This could be due to the increased immunosuppression given to these patients predisposing to infection.
The most common organism causing UTI was E. coli (53.3%, 8/15) as in other studies.[121415] Recurrences were more common in patients presenting with E. coli UTI (4/6;66.6%) probably due to the persistence of uropathogenic E. coli by the formation of intracellular bacterial communities, which later enter a dormant state within host epithelial cells.[29] The intracellular localization of these bacteria renders them resistant to most antibiotics and inaccessible to infiltrating neutrophils and other host defenses. The resurgence of the organisms from these reservoirs can initiate recrudescent infections.
The incidence of recurrent UTI in the present study was 46.2% (6/13); similar rates of 42% and 44% were reported in other studies.[1630] Relapses/recurrences occur due to the persistence of the organism in the urinary tract and are associated with renal scars, stones, prostatitis, or the primary immunosuppressive regimen which might itself contribute to relapse.[31]
Factors contributing to reinfection in these patients could be the same as those for community-acquired UTI; frequent voiding, hydration, and voiding after sexual intercourse in women could be advised to reduce the reinfections.
Carbapenem resistance was observed only among the E. coli isolates (62.5%;5/8) whereas K. pneumoniae was the major multidrug-resistant (MDR) pathogen in other studies.[133233]
About 46.6% of the isolates were ESBL producers and were uniformly distributed in the 1st year of transplantation whereas the CR isolates were significantly more common in the 1st month of transplantation (P = 0.0020). Origuen et al. compared a cohort of patients between 2002 and 2004 with another cohort between 2011 and 2013 and observed the progressive increase in MDR pathogens, ESBL producers from 43.9% to 67.8% and 6.6% to 26.1%, respectively.
In the present study, all the Gram-negative organisms isolated within 1 month of transplantation were CR E. coli, sensitive to colistin. Combination antibiotic therapy with colistin as the most active agent along with high-dose carbapenems, aminoglycosides, or fosfomycin has been tried in most CR infections.[3435] Strict hand hygiene, decontamination of environmental surfaces and cohorting of patient care staff have been shown to reduce the CR infection rate and should be meticulously practiced in all the centers.[363738] However, screening for bowel colonization with ESBL, ampC beta-lactamase, or carbapenemase-producing Gram-negative bacteria in patients awaiting solid organ transplantation is not recommended except in outbreak situations.[39]
Conclusion
UTI is the common infectious complication in renal transplant patients. The high rate of carbapenem-resistant Enterobacteriaceae in the early posttransplant period is a point of concern, especially with cadaver transplants. Infection control practices and catheter care need to be strictly monitored to minimize the risk for UTI.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Bacterial urinary tract infection in renal transplant recipients and their antibiotic resistance pattern: A four-year study. Iran J Microbiol. 2014;6:74-8.
- [Google Scholar]
- Time table of infections after renal transplantation – South Indian experience. Indian J Nephrol. 2005;15(Suppl 2):S14-21.
- [Google Scholar]
- Prevalence of infections in renal transplant recipients of North India. Indian J Pathol Microbiol. 2007;50:453-7.
- [Google Scholar]
- Risk and outcome of pyelonephritis among renal transplant recipients. BMC Infect Dis. 2016;16:264.
- [Google Scholar]
- Can a silent kidney infection or genetic predisposition underlie recurrent UTIs? Medscape Womens Health. 1996;1:6.
- [Google Scholar]
- Infectious complications after kidney transplantation: Current epidemiology and associated risk factors. Clin Transplant. 2006;20:401-9.
- [Google Scholar]
- Urinary tract infection in the renal transplant patient. Nat Clin Pract Nephrol. 2008;4:252-64.
- [Google Scholar]
- Post-transplant infections: An ounce of prevention. Indian J Nephrol. 2010;20:171-8.
- [Google Scholar]
- Predisposing factors to the development of urinary tract infections in renal transplant recipients and the impact on the long-term graft function. Ren Fail. 2011;33:405-10.
- [Google Scholar]
- Study of the risk factors related to acquisition of urinary tract infections in patients submitted to renal transplant. Rev Soc Bras Med Trop. 2015;48:285-90.
- [Google Scholar]
- Risk factors for recurrent urinary tract infection in kidney transplant recipients. Transplant Proc. 2013;45:1584-9.
- [Google Scholar]
- Urinary tract infection among renal transplant recipients in Yemen. PLoS One. 2015;10:e0144266.
- [Google Scholar]
- Urinary tract infection in renal transplant recipients: Incidence, risk factors, and impact on graft function. Transplant Proc. 2014;46:1757-9.
- [Google Scholar]
- The prevalence and predictive factors of urinary tract infection in patients undergoing renal transplantation: A meta-analysis. Am J Infect Control. 2016;44:1261-8.
- [Google Scholar]
- Infectious complications and antibiotic use in renal transplant recipients during a 1-year follow-up. Clin Microbiol Infect. 2001;7:619-25.
- [Google Scholar]
- Bacterial and fungal infections after kidney transplantation. Curr Opin Urol. 1999;9:45-9.
- [Google Scholar]
- Urinary tract infection in renal transplant recipients. Eur J Clin Invest. 2008;38(Suppl 2):58-65.
- [Google Scholar]
- Analysis of risk factors associated with urinary tract infection in renal transplant recipients. In: 52nd ERA-EDTA Congress. London: Nephrology Dialysis Transplantation; 2015. p. :634-61. doi: 10.1093/ndt/gfv202.7
- [Google Scholar]
- Urinary tract infection in renal transplant recipients. Arab J Nephrol Transplant. 2010;3:53-5.
- [Google Scholar]
- Urinary tract infections during the first year after renal transplantation: One center's experience and a review of the literature. Clin Transplant. 2014;28:1263-70.
- [Google Scholar]
- Infectious complications in kidney transplant recipients: Review of the literature. Saudi J Kidney Dis Transpl. 2005;16:453-97.
- [Google Scholar]
- Frequency of urinary tract infection in renal transplant recipients and effect on graft function. J Pak Med Assoc. 2010;60:826-9.
- [Google Scholar]
- Predictive factors of infection in the first year after kidney transplantation. Transplant Proc. 2013;45:3620-3.
- [Google Scholar]
- Dialysis modality and delayed graft function after cadaveric renal transplantation. J Am Soc Nephrol. 1999;10:154-9.
- [Google Scholar]
- Urinary tract infection in patients after renal transplantation: Evaluation of risk factors. MEDtube Sci. 2014;2:22-9.
- [Google Scholar]
- Urinary tract infections: Current and emerging management strategies. Clin Infect Dis. 2013;57:719-24.
- [Google Scholar]
- Clinical, epidemiologic, and microbiologic study of urinary infection in patients with renal transplant at a specialized center in Argentina. Arch Esp Urol. 1993;46:473-7.
- [Google Scholar]
- The localization urinary tract infection and its relationship to relapse, reinfection and treatment. In: Brumfitt W, Asscher AW, eds. Urinary Tract Infection. London: Oxford University Press; 1973. p. :206-14.
- [Google Scholar]
- Recurrent urinary tract infections in kidney transplant recipients. Transplant Proc. 2013;45:1092-5.
- [Google Scholar]
- Progressive increase of resistance in Enterobacteriaceae urinary isolates from kidney transplant recipients over the past decade: Narrowing of the therapeutic options. Transpl Infect Dis. 2016;18:575-84.
- [Google Scholar]
- Epidemiology and molecular characterization of bacteremia due to carbapenem-resistant Klebsiella pneumoniae in transplant recipients. Am J Transplant. 2013;13:2619-33.
- [Google Scholar]
- Infection with Klebsiella pneumoniae carbapenemase (KPC)-producing K. pneumoniae in solid organ transplantation. Transpl Infect Dis. 2012;14:198-205.
- [Google Scholar]
- Successful control of an outbreak of Klebsiella pneumoniae carbapenemase-producing K. pneumoniae at a long-term acute care hospital. Infect Control Hosp Epidemiol. 2010;31:341-7.
- [Google Scholar]
- Success of an infection control program to reduce the spread of carbapenem-resistant Klebsiella pneumoniae. Infect Control Hosp Epidemiol. 2009;30:447-52.
- [Google Scholar]
- Containment of a country-wide outbreak of carbapenem-resistant Klebsiella pneumoniae in Israeli hospitals via a nationally implemented intervention. Clin Infect Dis. 2011;52:848-55.
- [Google Scholar]
- ESCMID Study Group for Infections in Compromised Hosts. Multidrug-resistant bacteria in solid organ transplant recipients. Clin Microbiol Infect. 2014;20(Suppl 7):49-73.
- [Google Scholar]







