Translate this page into:
Schistosoma hematobium-associated glomerulopathy
Address for correspondence: Dr. Sidy Mohamed Seck, Department of Nephrology, University Hospital Aristide Le Dantec, 30 Avenue Pasteur, BP 3001, Dakar, Senegal. E-mail: sidymseck@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Schistosomiasis is the second most devastating tropical parasitic disease worldwide and is responsible for many urological complications. However, glomerular injury is a rare complication mainly described with Schistosoma mansoni. We report a case of membranoproliferative glomerulonephritis (MPGN) associated with Schistosoma hematobium infection in a young Senegalese boy living in a rural area. Clinical presentation was with steroid-resistant with nephrotic syndrome. Renal biopsy showed type 1 MPGN with the presence of S. hematobium eggs surrounded by a gigantocellular granuloma. Despite therapy with antihelminthic and immunosuppressive drugs, evolution was characterized by progression to end-stage renal disease over 1 year. More efforts should be made on the prevention and early detection of schistosomiasis among at-risk populations.
Keywords
Membranoproliferative glomerulonephritis
Schistosomia hematobium
nephrotic syndrome
Introduction
Schistosomiasis or bilharzia is a tropical parasitic disease caused by the larvae of one or more of five types of blood flukes called schistosomes. It counts as the second most devastating tropical parasitic disease worldwide after malaria with more than 200 millions of cases mainly in rural agricultural and periurban areas of developing countries[12] and is responsible for many uronephrological complications.[3] In Senegal, schistosomiasis is very frequent in northern and eastern regions but renal complications have been rarely reported.[23] Glomerular diseases had been well described in association with Schistosoma mansoni but exceptionally with other species.[45] We report the first case of Schistosoma hematobium infection associated with membranoproliferative glomerulonephritis (MPGN) in a Senegalese boy.
Case Report
A 10-year-old boy had been admitted at a nephrology clinic for generalized edema, hypertension, and fatigue that appeared 3 weeks before. His medical past was unremarkable and immunization status was complete. His mother reported baths in stagnant water 5 years ago in their village. But, there was neither personal nor familial history of hematuria or edema. Physical examination showed height 130 cm, weight 30 kg, temperature 37°C, high blood pressure (150/90 mmHg), tachycardia (100 beats/min), and edema over face, back, limbs, and mild ascites. Cardiac and pulmonary auscultation was normal and there was neither arthritis, nor skin abnormality.
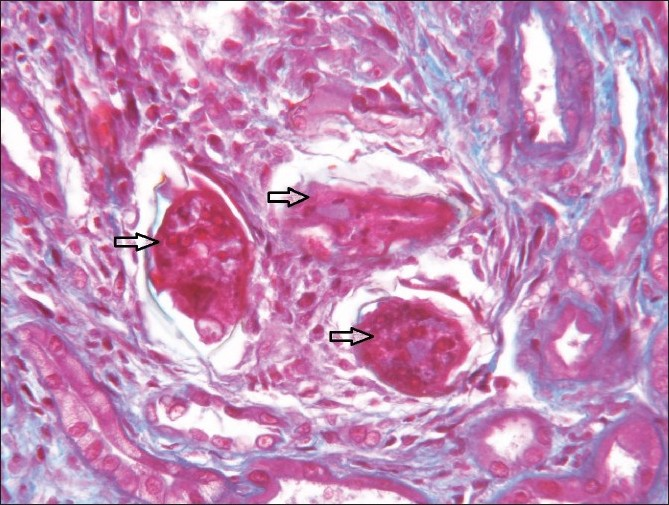
Laboratory findings are represented in Table 1. Serologies for hepatitis B, C, and HIV were negative and serum complement (CH50) was slightly low. Cryoglobulins, and anti-DNA and anti-streptococcal antibodies were not found. Ultrasound examination of kidneys and the lower urinary tract was strictly normal.
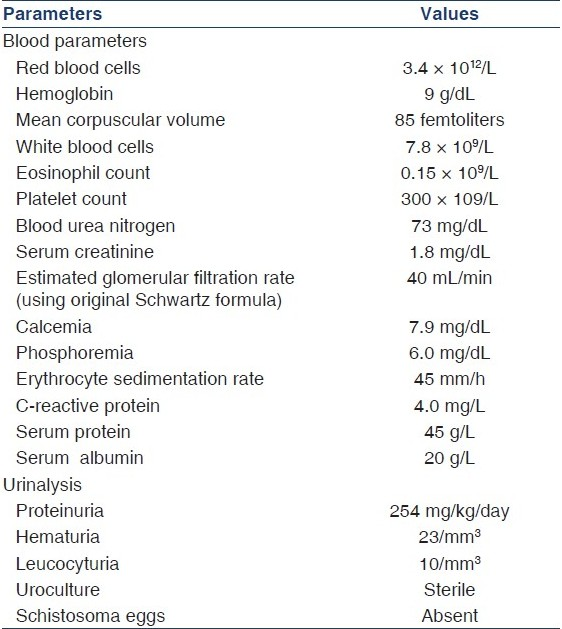
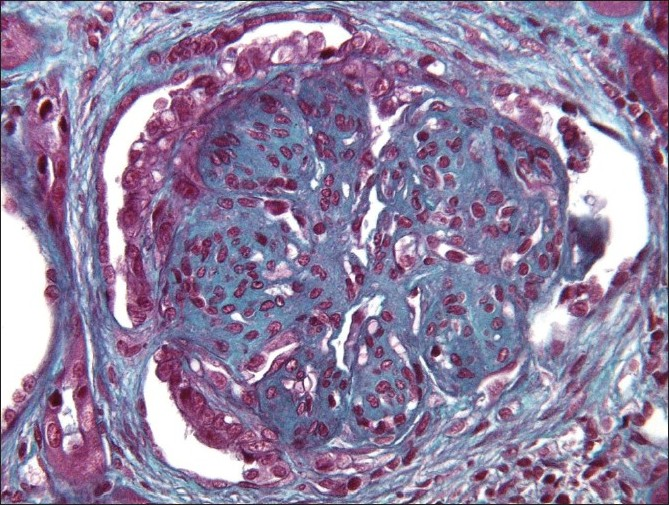
Diagnosis of nephrotic syndrome was made and the patient was treated with oral prednisolone (2 mg/kg/day) combined with captopril (50 mg/day), salt-free diet, furosemide (60 mg/day), and oral supplementation with potassium, calcium, and vitamin D3. Four weeks later, edema decreased slightly and urine albumin excretion slowed down at 187 mg/kg/day. Urine sediment was still unremarkable. A second 4-week period of oral prednisolone was started after three daily IV pulses of methylprednisolone (10 mg/kg/day). However, clinical and biological findings did not improve at the end of this cure. Then, renal biopsy was performed and showed type 1 membranoproliferative glomerulonephritis (MPGN) [Figure 1] with mild tubulointerstitial fibrosis and a granuloma made of histiocytes and giant cells surrounding an egg of S. hematobium [Figure 2]. Congo red staining was negative and immunofluorescence did not find any deposition. Circulating IgG antibodies against schistosomal antigens were high (1/250). A final diagnosis of type 1 MPGN secondary to S. hematobium was made. The histological findings corresponded to class III–IV of the African Association of Nephrology (AFRAN) classification.[67] Despite the absence of adult worms in urine and renal parenchyma, treatment with praziquantel was given (single 40 mg/kg dose per os) to ensure complete cure. After 1 month, there was no improvement in renal function. Then, oral cyclophosphamide (2 mg/kg/day) was added to corticosteroids with supportive therapy (salt-free diet, captopril, furosemide, calcium, and vitamin D3) for 6 months. Nevertheless, the patient reached end-stage renal disease (ESRD) 1 year later and had to start hemodialysis.
- Renal biopsy showing type 1 membranoproliferative glomerulonephritis with mild tubulointerstitial fibrosis (optical microscopy hematoxillin–eosin staining)
- Granuloma made by histocytes and giant cells surrounding three Schistosoma hematobium eggs (black arrows) PAS staining magnification ×400
Discucssion
This is the first case report of S. hematobium-associated MPGN in Senegal. However, in relation to the high prevalence of schistosomiasis in endemic areas, it might be underdiagnosed due to the absence of systematic screening. In fact, MPGN is very rare among Senegalese patients.[8] In this case, other causes of MPGN such as hepatitis C virus and lupus were excluded. Glomerular disease secondary to schistosomiasis had been reported in 10–15% of patients mainly with S. mansoni infection and MPGN is the most common histological pattern[79–11] Glomerular injury is generally due to direct deposition of schistosomal antigens (GASP, gut-associated schistosomal proteoglycan). Chronic hepatosplenic infection plays an important role in the subsequent disease progression.[69] S. hematobium has a greater tropism for lower urinary tract (ureter, urethra, bladder). This case of MPGN associated with S. hematobium infection is unusual but the mechanism of glomerular injury might be similar to S. mansoni infection. However, there was not any glomerular deposition at immunofluorescence in contrast with MPGN due to S. mansoni where glomerular and peritubular IgA deposits are frequent.[7912]
Clinical presentation in our case was with steroid-resistant nephrotic syndrome with increased serum creatinine level. In glomerular disease associated with S. mansoni, renal manifestations can vary from asymptomatic albuminuria and normal renal function to ESRD.[7] However, most patients present with nephrotic syndrome, hypertension, and a plasma creatinine concentration between 1 and 2 mg/dL (88 and 176 μmol/L).[10] The absence of hematuria and leucocyturia in our patient was compatible with low disease activity even if total serum complement was slightly consumed. In fact, the presence of mild fibrosis and some sclerotic glomeruli in renal biopsy suggested an advanced injury. It is not known if blacks preferentially develop focal segmental glomerulosclerosis in this setting. Progression to ESRD occurred rapidly in our patient despite aggressive therapy. This observation confirmed bad prognosis of classes III–V in which treatment with both antihelmintic drugs and immunosuppressive agents (prednisone and cyclophosphamide) is usually not effective in progression to ESRD.[57] Conversely, in the two first classes, complete recovery can occur spontaneously or after therapy.[710] To reduce morbidity, public health policy should concentrate on prevention by snail control, improved sanitation and health education, and implementation and sustaining of chemotherapy-based control strategies.[1513]
To conclude, MPGN is a rare complication during S. hematobium infection but with potentially poor prognosis. It can lead rapidly to ESRD. Antihelminthic and immunosuppressive treatments are not effective at advanced stages and efforts might focus on the prevention, early detection, and treatment of schistosoma infections among at-risk groups.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Fact sheet on Shistosomiasis. World Health Organisation, Geneva (2010) Fact sheet 115. Available from: http://www.who.int/mediacentre/factsheets/fs115/en/index.html
- [Google Scholar]
- Prevalence of urinary schistosomiasis in the school population in Senegal in 2002. Dakar Med. 2005;50:198-201.
- [Google Scholar]
- Schistosomiasis in school children in the Bandafassi region of East Senegal. Med Trop. 2008;68:267-71.
- [Google Scholar]
- Urinary tract pathology in Schistosoma haematobium infected rural Nigerians. Southeast Asian J Trop Med Public Health. 2007;38:32-7.
- [Google Scholar]
- Histopathological profiles of nephropathies in Senegal. Saudi J Kidney Dis Transpl. 2003;14:212-4.
- [Google Scholar]
- Schistosoma mansoni-induced mesangiocapillary glomerulonephritis: Influence of therapy. Kidney Int. 1989;35:1227-33.
- [Google Scholar]
- Human Schistosoma mansoni-associated glomerulopathy in Brazil. Nephrol Dial Transplant. 2002;17:4-7.
- [Google Scholar]
- Immunoglobulin-A and the pathogenesis of schistosomal glomerulopathy. Kidney Int. 1996;50:920-8.
- [Google Scholar]
- WHO Expert Committee, Prevention and control of schistosomiasis and soil-transmitted helminthiasis. In: Technical report series. Vol 912. Geneva: World Health Organisation; 2002. p. :57.
- [Google Scholar]







