Translate this page into:
Serious Infectious Complications Related to Atopic Dermatitis in a Peritoneal Dialysis Patient
Address for correspondence: Dr. Y. K. Wen, Department of Internal Medicine, Division of Nephrology, Changhua Christian Hospital, 135 Nanhsiao Street, Changhua 500, Taiwan, Republic of China. E-mail: wenyaoko@yahoo.com.tw
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
A 39-year-old female with end-stage renal disease had been maintained on peritoneal dialysis (PD) for 5 years uneventfully. The patient was admitted because of cloudy peritoneal effluent accompanied by abdominal pain that began just few hours before admission. Furthermore, she had been afflicted with low back pain and intermittent fever for 1 week. On physical examination, body temperature of 38.5°C, diffuse abdominal tenderness, and lower spinal tenderness were noted. A diastolic murmur was audible along the left sternal border. There was scaling erythema with lichenification and excoriation over bilateral hands. The PD catheter exit site was clean, and there were no signs of tunnel infection. Neurologic assessment revealed decreased muscle power of the left lower limb. Laboratory tests were remarkable for peripheral white blood cell (WBC) count of 28,000/mm3 and the WBC count in the peritoneal effluent of 3925/mm3. A Gram-stain of the centrifuged dialysis effluent revealed Gram-positive microorganism. Antibiotic treatment with intraperitoneal vancomycin was initiated and then changed into parenteral oxacillin when the cultures of PD effluent and blood both reported to grow oxacillin-sensitive Staphylococcus aureus (OSSA). A culture sample from the skin lesions of atopic dermatitis also grew OSSA, showing the same antimicrobial susceptibilities as the blood culture isolated. Due to lower back pain accompanied by neurologic deficits, MRI of the lumbar spine was arranged and vertebral osteomyelitis affecting S1 joint was disclosed with abscess in the left lower iliacus muscle. Echocardiography showed vegetation (2.33 cm × 0.83 cm) over the aortic valve with severe aortic regurgitation [Figure 1]. The patient had dyspnea and shock on the third hospital day. Stabilization was achieved in the intensive care unit using inotropic agents. Although abdominal pain improved and PD effluent became clear soon after antibiotic treatment, other infectious signs including fever, leukocytosis, and OSSA bacteremia continued to be noted over 10 days after admission. Aortic valve replacement surgery was performed. After antibiotic treatment with oxacillin 2 g intravenously every 4 h for 8 weeks, the patient was discharged in a stable condition. Mild left leg weakness remained. Eventually, her neurologic deficit almost completely recovered after approximately 2-month rehabilitation.
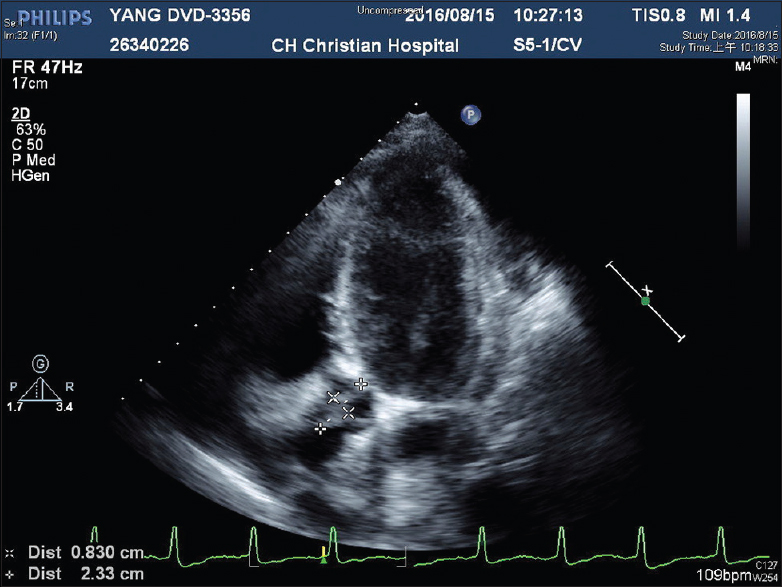
- Vegetation (2.33 cm × 0.83 cm) over aortic valve revealed by echocardiography (cross mark)
In our patient, the present illness suggested that vertebral osteomyelitis preceded the appearance of peritonitis. Vertebral osteomyelitis most often occurs as a result of hematogenous spread from a distant focus and is a well-recognized complication of infective endocarditis (IE).[1] It is probable that the subsequent development of peritonitis in our patient was also associated with systemic bacteremia. Furthermore, uncontrolled infection continued to be noted after PD effluent became clear, indicating that persistent bacteremia was caused by other infection focus rather than by unresolved peritonitis. Therefore, we believe that the primary infection focus was IE in this PD patient. She had no past history of rheumatic heart disease and her previous cardiac evaluation was normal. She also had no recent dental procedures. However, she had long-standing atopic dermatitis, which recently worsened over bilateral hands. Since colonization of S. aureus is commonly observed in skin lesions of atopic dermatitis patients, and scratching of the pruritic lesions may lead to bacterial invasion into the bloodstream and subsequent systemic infections, we suspect her atopic dermatitis lesions as a source for IE. The increasing reports have raised awareness of the relationship between IE and atopic dermatitis.[23] Literature reviewed showed only two case reports of PD peritonitis and IE. In the first case, mitral valve vegetation were noted at autopsy 1 month after an episode of Streptococcus faecalis peritonitis with bacteremia.[4] The second case documented IE giving rise to peritonitis in a PD patient, in which persistent Streptococcus equinus bacteremia prompted further search for infection source, and finally vegetation on aortic valve was detected by transesophageal echocardiography.[5] In conclusion, this case suggests that hematogenous source of peritonitis should be considered in PD patients presenting with extra-abdominal manifestations accompanied by persistent bacteremia. Furthermore, atopic dermatitis lesions should be recognized as a potential bacterial source for IE.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Atopic dermatitis as a risk factor for acute native valve endocarditis. J Heart Valve Dis. 2000;9:469-71.
- [Google Scholar]
- Pay attention to valvular disease in the presence of atopic dermatitis. Circ J. 2013;77:1862-6.
- [Google Scholar]
- Bacterial endocarditis due to an infected peritoneal dialysis catheter. A case report. S Afr Med J. 1983;64:718-9.
- [Google Scholar]
- Infective endocarditis giving rise to peritonitis in a patient on peritoneal dialysis. Perit Dial Int. 2013;33:462-3.
- [Google Scholar]






