Translate this page into:
Spontaneous Colonic Perforation in a Patient on Peritoneal Dialysis
Corresponding author: Vinay Rathore, Department of Nephrology, All India Institute of Medical Sciences, Raipur, Chhattisgarh, India. E-mail: vinayrathoremd@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Aggarwal J, Yelavarthy YM, Rathore V, Bodhey NK, Ramchandani R. Spontaneous Colonic Perforation in a Patient on Peritoneal Dialysis. Indian J Nephrol. doi: 10.25259/IJN_108_2025
Dear Editor,
Colonic perforation in the absence of tumors, diverticulosis, or external injury is rare.1 Its diagnosis is delayed in patients on peritoneal dialysis (PD) because the dialysate often masks the signs and symptoms of PD-related peritonitis.2
A 53-year-old woman on continuous ambulatory PD (CAPD) for 10 months presented with fever, non-bilious vomiting, diffuse pain in the abdomen, and cloudy PD fluid. PD effluent had a 1200/μL white blood cell count with 81% neutrophils. She was started on intraperitoneal vancomycin and gentamycin. PD fluid culture grew Escherichia coli sensitive to gentamycin.
Dialysate total cell count showed no improvement after 3 days, and she developed abdominal distension and obstipation. Contrast-enhanced computed tomography (CECT) abdomen revealed colon perforation [Figure 1]. Laparotomy revealed perforation near the proximal two-third and distal one-third junctions of the transverse colon. Feculent peritoneal fluid was drained and end transverse colostomy was done. Despite intensive care, including mechanical ventilation, inotropic support, and continuous renal replacement therapy, she developed multiorgan failure and died on the tenth day.
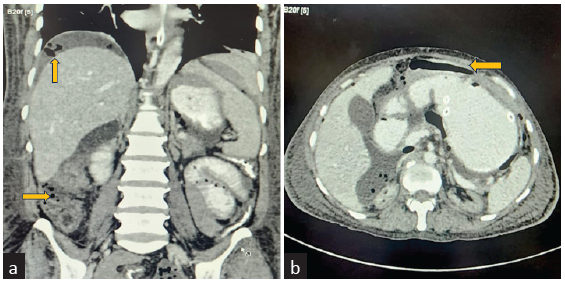
- Contrast-enhanced computed tomography images (a) coronal view and (b) axial view showing multiple extra-luminal air attenuating foci in the non-dependant portion of the intra-peritoneal compartment of the abdomen (yellow arrows).
Perforation peritonitis is a severe complication with a high mortality rate;3 however, diagnosis is often delayed due to confusion with PD-related peritonitis in CAPD patients. CECT should be considered early if peritonitis symptoms don’t improve after appropriate antibiotic initiation.2
Causes of perforation are ischemic colitis, tuberculosis, malignancy, perforated diverticulitis, inflammatory bowel disease, sclerosing peritonitis with mural bowel fibrosis, cholecystitis, and rarely chronic constipation.4 In the index case, the colonic perforation was spontaneous and could have resulted from constipation. Solid feculent mass compresses the colonic wall, diminishes the blood supply, leads to ischemia in the anti-mesenteric border, and necrosis of colonic mucosa, forming feculent ulcerative changes1 as were observed in the histopathological examination of our case.
Conflicts of interest
There are no conflicts of interest.
References
- Diagnosis and treatment of spontaneous colonic perforation: analysis of 10 cases. World J Gastroenterol. 2008;14:4569-72.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Perforative peritonitis confused with peritoneal dialysis-related peritonitis: Report of three cases. Int J Surg Case Rep. 2020;70:20-3.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Abdominal catastrophe revisited: The risk and outcome of enteric peritoneal contamination. Perit Dial Int. 2002;22:323-34.
- [CrossRef] [PubMed] [Google Scholar]
- Viscus perforation in peritoneal dialysis patients: Diagnosis and outcome. Perit Dial Int. 1994;14:371-7.
- [CrossRef] [PubMed] [Google Scholar]







