Translate this page into:
Spontaneous pneumomediastinum and subcutaneous emphysema in continuous ambulatory peritoneal dialysis patient
Address for correspondence: Dr. Quaid Nadri, Department of Medicine, King Faisal Specialist Hospital and Research Centre, Riyadh 1121, Kingdom of Saudi Arabia. E-mail: qnadri@kfshrc.edu.sa
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Peritoneal dialysis (PD) has been a successful modality in patients with end-stage renal disease (ESRD). Besides its usual complications such as infection, hernias, genital edema and Tenchoff catheter related mechanical problems, rare complications such as pneumoperitoneum, subcutaneous emphysema (SE) and pneumomediastinum in continuous ambulatory peritoneal dialysis (CAPD) and automated peritoneal dialysis (APD) patients have been reported.[123]
A 29-year-old female patient with ESRD from systemic lupus erythematous on CAPD for 1½ year presented to emergency with 2 days history of fatigue, Shortness of breath, chest pain radiating to back and vomiting. Denied fever and abdominal pain. Patient was hypotensive, dyspneic and dehydrated. Subcutaneous crepitation felt over upper chest and neck. Chest exam revealed decreased breath sound and scattered crackles all over the chest on auscultation. Abdomen was soft non-tender. Chest X-ray showed SE, bilateral pneumothorax and pnemomediastinum [Figure 1]. This was confirmed by computed tomography (CT) chest. With a history of vomiting, CT ruled out esophageal perforation. Gastrograffin swallow study showed no esophageal leak. There was no sign of peritonitis and PD fluid was clear. Patient was resuscitated with intravenous fluids with restoration of hemodynamic and maintained on oxygen therapy. Patient did not require mechanical ventilation and chest tube insertion. On conservative management under intensive care unit, symptoms, oxygenation and chest X-ray improved over 3 days. Patient continued on CAPD and discharged in stable condition after 6 days.
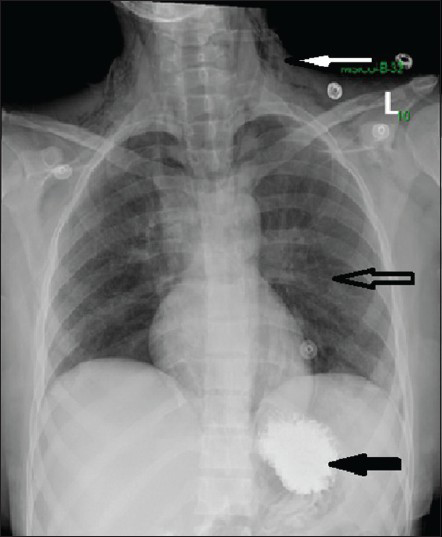
- Chest X-ray showing subcutaneous emphysema (upper arrow) pneumomediastinum and pneumothorax (middle arrow) and gastrografin in stomach (lower arrow)
In this case no peritoneal complication such as peritonitis or PD catheter related problem occurred. Previous reports[123] described in CAPD and APD patients were associated with either translocation of Tenckhoff catheter to the retroperitoneal cavity with hematoma or was associated with faulty dialysis technique. Spontaneous pneumomediastinum and SE has several etiologies; asthma, chronic obstructive pulmonary disease, forced vomiting, esophageal rupture. Spontaneous pneumomediastinum is not associated with blunt force or penetrating chest trauma, endobronchial or esophageal procedures, mechanical ventilation, chest surgery or other invasive procedures. The development of SE and pneumomediastinum in this patient may had been resulted from esophageal rupture after vomiting with spontaneous seal called Boerhaave syndrome (esophageal rupture following vomiting). Contrast CT ruled out esophageal perforation in this case. There was no pnemoperitonum which ruled out abdominal causes such as bowel perforation, nor did the patient undergo a new PD catheter insertion, as reported in previous cases. Interestingly in all cases SE and pneumomediastinum resolved within few days on conservative management and adequacy of PD was maintained without recurrence.
This case attempts to highlights the importance of awareness of such rare condition in PD patient.
References
- Pneumomediastinum and subcutaneous emphysema – Unusual complications of automated peritoneal dialysis. Perit Dial Int. 2003;23:97-8.
- [Google Scholar]
- Pneumoperitoneum and pneumomediastinum in a CAPD patient with peritonitis. Perit Dial Int. 1997;17:389-91.
- [Google Scholar]
- An unusual complication of peritoneal dialysis catheter insertion. Nephrology (Carlton). 2008;13:357-8.
- [Google Scholar]






