Translate this page into:
Straight versus Coiled Catheters in Peritoneal Dialysis in a Tertiary Care Center in Malaysia
Address for correspondence: Dr. Christopher T. S. Lim, Department of Medicine, Level 3, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia - 43400, Serdang, Selangor, Malaysia. E-mail: drchrislim@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Despite improvements in insertion techniques and catheter designs, catheter malfunction and infection pose a great source of morbidity and limitation to adequate dialysis. The two most used peritoneal dialysis (PD) catheters are the coiled and straight PD catheters. Existing studies show conflicting results.
Methods:
This study aims to look at the clinical outcomes and mortality between the two catheter types. This study was designed as an ambidirectional cohort study. A total of 126 patients undergoing PD, with 75 receiving the straight PD catheter and 51 receiving the coiled PD catheter, participated in the study. The primary outcome was catheter survival, and the secondary outcomes included PD failure, catheter-related infections, and all-cause mortality.
Results:
In the coiled catheter group, 30 (40%) patients had catheter malfunction, whereas the straight catheter group had 15 (29.4%) patients catheter malfunction. However, the survival functions represented by the Kaplan–Meier survival curve did not show any statistical significance (P = 0.659). In the coiled PD catheter group, 13 (17.3%) had PD failure, which was comparable with the straight PD catheter group of nine (17.6%) cases (P = 1.000). The catheter-related infections are similar in both groups. The mortality between two groups was also similar (P = 0.777).
Conclusions:
There is no difference in outcomes between the coiled and straight PD catheters.
Keywords
Catheter malfunction
coiled catheter
mortality
peritoneal dialysis
straight catheter
Introduction
In Malaysia, there has been a steady rise in new end-stage renal failure (ESRF) patients requiring dialysis every year, and the rate is increasing by more than 1.8-fold from 2009 to 2016.[1] The government remains the biggest source of funding for hemodialysis (HD) patients with total provisions spent for dialysis reaching USD 100 million, and this cost is predicted to increase by 10-fold in the year 2040.[234] Despite studies showing better cost-effectiveness of peritoneal dialysis (PD), this method of renal replacement therapy (RRT) is still underutilized.[5] The success of the PD program is largely dependent on PD access; however, catheter malfunction and infection continue to limit adequate RRT and remain a great cause of mortality. Two most commonly used PD catheters are the coiled and straight catheters, although international and local guidelines do not recommend the use of one over the other.[678]
Materials and Methods
Study design
This ambidirectional cohort study was conducted in a tertiary care center in Malaysia over 124 months. We recruited patients from August 2008 until December 2010 and included all patients above the age of 18 years with a diagnosis of ESRF who opted for PD (continuous ambulatory peritoneal dialysis and automated peritoneal dialysis). Patients who had a PD catheter for intermittent PD while awaiting vascular access, those who were referred from another center, and those who had a concurrent illness that hinders patient compliance with our study were excluded. This study was reviewed and approved by the Medical Research and Ethics Committee of the Health Ministry of Malaysia on 12th July 2018 (NMRR-18-865-41205).
All PD catheters were inserted by a single interventional nephrologist using the peritoneoscopic method (Y-Tec© system, Medigroup with a 2.2-mm scope and VP210 STD set). The catheters utilized were doubled-cuffed coiled (57.5 cm) and straight (47 cm) PD catheters. Prior to insertion, standard catheter care with mupirocin and povidone-iodine was employed, and intravenous cefazolin was given as prophylactic antibiotics. Ambulatory PD was delayed for at least 2 weeks after insertion. If immediate dialysis was required, a lower volume (750–1,000 mL) of dialysate was used.
We utilized a standardized data collection sheet to record the patient details, comorbidities, as well as the occurrence of infection, catheter malfunction and their respective dates, mortality, and the cause of death. These data were retrieved from our computerized system by trained medical personnel.
Outcomes
The primary outcome was catheter survival, which is defined as time to primary catheter dysfunction from the time of insertion that may or may not require surgical intervention. The secondary outcomes included all-cause PD failure (defined by the necessity to change to another modality of RRT), catheter-related infections (peritonitis, exit-site infection, and tunnel tract infection), and all-cause mortality. All patients were followed up until death or until completion of the study in December 2017.
Statistical analysis
Data were analyzed on an intention-to-treat basis, using SPSS Version 20. Numerical variables (primary outcomes) were checked for normality distribution, and appropriate measures of central dispersion were used to describe the data. Thus, catheter survival was presented as mean (standard deviation [SD]), and an independent t test was used to compare the means of two groups. The categorical variables were presented as frequencies and percentages. Chi-square test was used to examine the associations. A P value of < 0.05 was considered significant. The survival outcomes for catheter dysfunction and all-cause mortality were presented using the Kaplan–Meier survival curves.
Results
Demographic data
In all, 200 patients were assessed for eligibility, and 126 patients were enrolled, of which 75 patients received the coiled PD catheter and 51 patients' straight PD catheter [Figure 1]. Baseline demographic characteristics [Table 1] between both groups were comparable regarding age, anthropometric data (weight, height, body mass index), and the primary cause of ESRF. Diabetes as primary cause of ESRF accounted for 78.7% and 92.2% in the coiled and straight PD catheter groups, respectively. Most of the patients were dialysis-naïve patients who embarked on RRT with PD, 54 (72%) in the coiled group and 42 (82.4%) in the straight group. The time required to insert both types of catheters did not differ with a mean of 33 minutes and 34 minutes in the coiled and straight catheter groups, respectively.

- Study flow diagram
| Coiled (n=75) | Straight (n=51) | P | |
|---|---|---|---|
| Age, years | 49.4 (16.79) | 53.4 (14.67) | 0.173 |
| Male sex | 40 (53.3%) | 29 (56.9%) | 0.696 |
| Race | |||
| Malay | 42 (56%) | 31 (60.8%) | 0.034 |
| Chinese | 21 (28%) | 19 (37.3%) | |
| Indian | 12 (16%) | 1 (2%) | |
| Height, cm | 157.2 (10.88) | 158.6 (9.5) | 0.438 |
| Weight, kg | 58.0 (14.10) | 60.4 (12.49) | 0.349 |
| Body mass index, kg/m2 | 23.18 (5.32) | 23.1 (4.02) | 0.946 |
| Cause of ESRF | |||
| Diabetes mellitus | 59 (78.7%) | 47 (92.2%) | 0.049 |
| Hypertension | 3 (4%) | 2 (3.9%) | 1.000 |
| Glomerulonephritis | 10 (13.3%) | 0 | 0.006 |
| Obstructive uropathy | 1 (2.7%) | 1 (2%) | 1.000 |
| Unknown | 1 (1.3%) | 1 (2%) | 1.000 |
| First method of RRT | |||
| A. Peritoneal dialysis | 54 (72%) | 42 (82.4%) | 0.180 |
| B. Hemodialysis | 21 (28%) | 9 (17.6%) | |
| Time to insert catheter, minutes | 33.01 (12.30) | 34.72 (14.8) | 0.482 |
ESRF=End-stage renal failure, RRT=Renal replacement therapy
Catheter survival
Catheter survival was the time to catheter malfunction regardless of reason, from the time of insertion. The mean time to malfunction is longer in the coiled PD catheter group, 3.64 ± 11.08 months as opposed to 3.29 ± 8.78 months in the straight PD catheter group (P = 0.852). However, the survival functions [Figure 2] did not show any statistical significance.

- Kaplan–Meier survival curves for catheter survival between coiled (straight line) and straight (dotted line) PD catheter groups
In the coiled catheter group, 30 (40%) patients had catheter malfunction, with 10 (13.3%) patients having catheter leakages and 9 (12%) having tip migrations. Six (8%) patients had flow problems, 3 (4%) patients had omental wrappings, and 2 (2.7%) had pleura-peritoneal fistulas. In comparison, the straight catheter group had 15 (29.4%) patients suffering from catheter malfunctions with 7 (13.7%) suffering from catheter leakages and 5 (9.8%) patients having flow problems. When assessing the flow problems in both the straight and coiled catheter groups, we excluded patients whose cause of inflow and outflow were reversible, such as those with fecal-loaded abdomen and those who responded to the use of regular laxatives. Our center does not advocate the use of fibrinolytic therapy for PD patients. The number of patients having omental wrapping and tip migration was lower in the coiled PD catheter group (1 [2%] and 2 [3.9%], respectively), and there was no pleura-peritoneal fistula observed in the straight PD catheter group. However, the P value was not significant [Table 2].
| Reason malfunction | Coiled n (%) | Straight n (%) | P |
|---|---|---|---|
| Omental wrapping | 3 (4) | 1 (2) | 0.647 |
| Flow problems | 6 (8) | 5 (9.8) | 0.756 |
| Catheter leakage | 10 (13.3) | 7 (13.7) | 1.000 |
| Tip migration | 9 (12) | 2 (3.9) | 0.197 |
| Pleuro-peritoneal fistula | 2 (2.7) | 0 (0) | 0.514 |
| Total events | 30 (40) | 15 (29.4) | 0.259 |
PD failure
In the coiled PD catheter group, 13 (17.3%) had PD failures, which required the patients to be switched to HD or dropped out from the PD program. The number of PD failures in the straight PD catheter group was comparable, accounting for 9 (17.6%) cases (P = 1.000). The most common cause of PD failure in both groups was an infection, 7 (53.8%) in the coiled PD catheter group and 5 (55.6%) in the straight PD catheter group (P = 0.647). However, these data were not statistically significant.
Catheter-associated infections
We evaluated peritonitis rate, exit-site infection rate, and tunnel tract infection rate, which was expressed in episodes per patient-year. The catheter-related infections were similar between both groups [Table 3].
| Coiled | Straight | P | |
|---|---|---|---|
| Peritonitis rate | 0.29 | 0.31 | 0.909 |
| Exit-site infection rate | 0.31 | 0.37 | 0.730 |
| Tunnel infection rate | 0.02 | 0.02 | 0.430 |
Mortality
There were 22 deaths in the coiled PD catheter group (29.3%) and 14 deaths in the straight PD catheter group (27.5%). The most common cause of death in both groups was sepsis, with 10 (13.3%) in the coiled PD catheter group and 6 (11.8%) in the straight PD catheter group. Of the 6 patients with sepsis in the straight PD catheter group, 3 deaths were contributed by peritonitis. Interestingly, there was no peritonitis reported in the coiled PD catheter group. Cardiac-related issues were the second most common cause of death in both groups, accounting for 9 (12%) patients in coiled PD catheter group and 5 (9.8%) in the straight PD catheter group. The two most common cardiac causes were acute coronary syndrome (6.7% vs. 2%) and sudden cardiac deaths (4% vs. 7.8%). One patient in the coiled PD catheter group (1.3%) died of acute pulmonary edema, whereas one patient in the straight PD catheter group (2%) died of acute respiratory distress syndrome. There were two patients in both groups that suffered from intracranial bleed (2.7% vs. 3.9%). The Kaplan–Meier survival curve between coiled PD catheter and straight PD catheter groups [Figure 3] did not show any statistical significance regarding all-cause mortality and catheter type (P = 0.777).
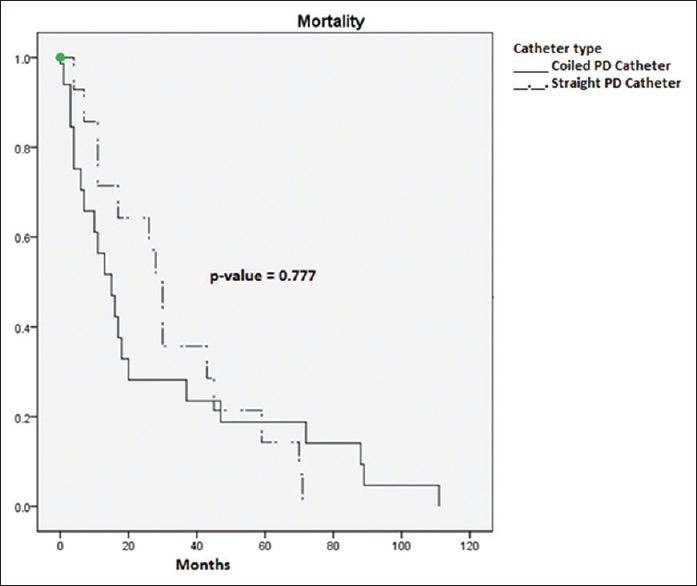
- Kaplan–Meier survival curves for all-cause mortality between coiled (straight line) and straight (dotted line) PD catheter groups
Discussion
PD therapy is becoming a popular choice as the initial RRT modality, as it gives patients independence, freedom, as well as the flexibility to function in society. Despite improvements in insertion techniques and catheter designs, catheter malfunction and infection continue to be a great source of morbidity and limitation to adequate dialysis.
Two most used PD catheters are the coiled and straight PD catheters. However, existing studies show conflicting results.[9101112] Although there have been many international data comparing outcomes of the different catheters with heterogeneous and variable results, Malaysia still lacks local evidence to guide best practices for peritoneal access.[6791011121314] In keeping with the international guidelines, meta-analyses, and studies, we hypothesized that there is no difference in the outcome between the coiled and straight PD catheter groups.
The results of our study demonstrate a trend of higher catheter malfunction in the coiled PD catheter group as compared with the straight PD catheter group; however, there was no statistical significance.[101314] The main cause of catheter malfunction was catheter leakage that is attributable to several reasons. Despite effective RRT counseling and patient education, our patients embark on RRT later in the course of their disease for many logistic reasons. Therefore, they are more prone to suffer complications of ESRF such as fluid overload, contributing to the higher catheter leakage in our patients. Another contributor is the fact that although our center advocates 10 to 14 days of wound healing prior to starting PD, some patients had to be started earlier, albeit with a lower dialysate volume.
Flow problems that include inflow and outflow issues, omental wrapping, and tip migration were also more prevalent in the coiled PD catheter group. Patients with the reversible cause of flow obstruction were excluded; that is, those who responded to laxatives. As our center does not advocate the use of fibrinolytics for blocked catheters, our findings are likely to represent the true causes of flow obstruction. This is likely because as compared with the straight PD catheter that is implanted deep into the peritoneal cavity, the coiled PD catheter has a larger surface area in contact with the peritoneum, eliciting local inflammation, and causing more problems with dialysate flow, omental wrapping, and causing tip migration.
Furthermore, we encountered two cases of pleuro-peritoneal fistulas occurring in our coiled PD catheter group, whereas there was none in the straight PD catheter group. This trend is alarming, as pleuro-peritoneal fistulas are a challenge to treat. A possible explanation to this finding is the fact that the coiled PD catheters are longer and thus, in theory, can cause diaphragm irritation and contribute to fistula formation.
In these instances, interruption of PD with conversion to HD is often necessary, while many others required surgical intervention.[15] However, our patients were switched from HD to PD due to vascular access problems, thus converting them to HD proved an impossible task. Therefore, we opted for normal volume daytime exchanges (DAPD) as an alternative regime, and the patients had complete resolution of the fistula.[16] We postulate that by resuming PD, the dialysate acts as a natural sealant for the epithelial layers and the use of the DAPD regime reduces the pressure gradient thus promoting healing of the fistula.
In assessing the secondary endpoints, which included PD failure, catheter-related infections and mortality were similar between both groups, with no statistical significance. Despite our center's experience and expertise in managing PD patients, infection remains the biggest threat to a successful PD program. Our patients come from many tiers of economic status, but the majority were from middle- to working-class patients. Therefore, poor personal hygiene and a breach in the sterile procedure were common problems in our patients.
The strength of this study lies in the long duration in which the patients were followed up to 124 months. We also acknowledge the limitations of our study. First, as this is a single-center study, we were not able to conduct a proper randomized controlled trial. Second, this study was not designed to look at cost-effectiveness. However, since our comparison of outcomes study shows similar outcomes despite the type of PD catheter, it is best to carry out an economic evaluation to look at the burden of ESRF treatment on the local health care system.
Conclusion
There was no statistical significance between the coiled and the straight PD catheters regarding outcome and mortality. Our data suggest that there is a trend toward more malfunctions in the coiled PD catheter as opposed to the straight PD catheter.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank the Head of Department of Nephrology, Serdang Hospital, for supporting our research activities.
References
- Twenty Fourth Report of the Malaysian Dialysis and Transplant 2016, Kuala Lumpur 2018. Available from: https://www.msn.org.my/nrr/mdtr2016.jsp
- Dialysis provision and implications of health economics on peritoneal dialysis utilization: A review from a Malaysian perspective. Int J Nephrol. 2017;2017:1-7. doi: 10.1155/2017/5819629
- [Google Scholar]
- How public and private reforms dramatically improved access to dialysis therapy in Malaysia. Health Affairs. 2010;29:2214-22.
- [Google Scholar]
- Forecasting the incidence and prevalence of patients with end-stage renal disease in Malaysia up to the year 2040? Hindawi Int J Nephrol. 2017;2017:1-5. doi: 10.1155/2017/2735296
- [Google Scholar]
- Economic evaluation of centre haemodialysis and continuous ambulatory peritoneal dialysis in Ministry of Health hospitals, Malaysia. Nephrology. 2005;10:25-32.
- [Google Scholar]
- Caring for Australasians with renal impairment (CARI) Type of peritoneal Dialysis Catheter 2014:1-9.
- [Google Scholar]
- Risk predictors and causes of technique failure within the first year of peritoneal dialysis: An australia and New Zealand dialysis and transplant registry (ANZDATA) study? Am J Kidney Dis. 2018;72:188-97. doi: 10.1053/j.ajkd. 2017.10.019
- [Google Scholar]
- Clinical Practice Guidelines for Renal Replacement Therapy 2017:393.
- A randomized controlled trial of coiled versus straight swan-neck tenckhoff catheters in peritoneal dialysis patients. Am J Kidney Dis. 2006;48:812-21.
- [Google Scholar]
- A randomized clinical trial comparing the function of straight and coiled Tenckhoff catheters for peritoneal dialysis. Perit Dial Int. 2005;25:85-8.
- [Google Scholar]
- Catheter-related interventions to prevent peritonitis in peritoneal dialysis: A systematic review of randomized, controlled trials. J Am Soc Nephrol. 2004;15:2735-46.
- [Google Scholar]
- A comparative study on using coiled versus straight swan-neck tenckhoff catheters in patients undergoing peritoneal dialysis. Iran J Med Sci. 2008;33:169-72.
- [Google Scholar]
- A prospective randomized study on three different peritoneal dialysis catheters. Perit Dial Int. 2003;23:127-31.
- [Google Scholar]
- Comparing the incidence of catheter-related complications with straight and coiled tenckhoff catheters in peritoneal dialysis patients-a single-centre prospective randomized trial. Perit Dial Int. 2013;35:443-9.
- [Google Scholar]
- Management options for hydrothorax complicating peritoneal dialysis. Semin Dial. 2003;16:389-94.
- [Google Scholar]
- Resolution of pleura-peritoneal fistula via transient daytime ambulatory peritoneal dialysisregime (DAPD) – 8 years follow up. Pak J Med Sci. 2016;32:1302-4.
- [Google Scholar]







