Translate this page into:
Successful Renal Transplant in End-Stage Renal Disease with Chronic Immune Thrombocytopenia using Thrombopoietin Receptor Agonists and Intravenous Immunoglobulin
Corresponding author: Dr. Vineet Behera, INHS Asvini, Near RC Church, Colaba, Mumbai - 400 005, Maharashtra, India. E-mail: beheravineet@gmail.cm
-
Received: ,
Accepted: ,
How to cite this article: Behera V, Rohith KP, Chauhan P, Meshram A, Dhawan V, Ananthakrishnan R, et al. Successful Renal Transplant in End-Stage Renal Disease with Chronic Immune Thrombocytopenia using Thrombopoietin Receptor Agonists and Intravenous Immunoglobulin. Indian J Nephrol. 2024;34:185–8. doi: 10.4103/ijn.ijn_232_22
Abstract
Chronic kidney disease in immune thrombocytopenia (ITP) is uncommon, and renal transplant in this setting is rare. We discuss the successful renal transplant of a 29-year-old male with chronic ITP. During transplant, he was managed with thrombopoietin receptor agonist eltrombopag, intravenous methylprednisone, and intravenous immunoglobulin to maintain adequate platelet level. He recovered well with no major complications and good graft function and has been stable during the follow-up period. The case report highlights that renal transplantation is a feasible option in patients with ITP, even in the presence of low platelet counts.
Keywords
Eltrombopag
immune thrombocytopenia
renal transplant
thrombopoietin receptor agonists
Introduction
Immune thrombocytopenia (ITP) is an autoimmune disorder characterized by a low platelet count (<100,000/mm3).1 The occurrence of chronic kidney disease (CKD) in the setting of ITP is uncommon, and both conditions predispose each other to bleeding complications.2,3 Kidney transplantation in a patient with ITP is especially challenging as deranged platelet function, in the setting of uremia, multiplies the risk of bleeding.3 Therefore, renal transplantation in this setting is rarely done, with only a few case reports.2,4-6 We report a successful kidney transplantation in a patient with ITP and discuss the various aspects of management and complications in this scenario.
Case Report
A 29-year-old male had ITP since 5 years with a platelet count between 40,000 and 60,000/mm3 and no major bleeds. The patient received oral steroids and cyclosporine 3 years back, with partial response. During regular follow-up, the patient was detected to have azotemia (serum creatinine 3.02 mg/dL) and subnephrotic proteinuria (1600 mg/day). Renal biopsy done under the cover of platelet transfusion showed IgA nephropathy (M0E0S2T1-C0) with high chronicity (interstitial fibrosis and tubular atrophy >50%) The disease progressed to end-stage renal disease (ESRD) within 1 year, and the patient was initiated on thrice-weekly hemodialysis.
There was history of recurrent episodes of epistaxis and prolonged ooze from the AVF puncture site during dialysis, needing prolonged compression by tourniquet. Evaluation showed hemoglobin 10.4 g/dL, total leukocyte count 10,400/mm3 and platelet count 68,000/mm3, serum creatinine 8.2 mg/dL, subnephrotic proteinuria, and bilaterally shrunken kidneys. Detailed evaluation for other thrombocytopenia showed a negative workup for autoimmune causes (antinuclear antibody, anti-ds DNA, anti-neutrophil cytoplasmic antibody, and anti-phospholipid antibodies, C3 and C4 levels), infectious workup (serological tests for hepatitis B, hepatitis C, human immunodeficiency virus, cytomegalovirus [CMV], Epstein–Barr virus [EBV], parvovirus B19), Helicobacter pylori on endoscopic biopsy, vitamin B12 and folate levels, lactate dehydrogenase, and direct/indirect Coombs test were normal. Bone marrow studies showed normal cellular bone marrow with increased thrombopoiesis. During the 6-month period, the platelet count ranged between 30,000 and 100,000/mm3.
The individual was worked up for renal transplant with mother as the prospective donor. The platelet count was 50,000/mm3 before transplant. The patient was initiated on thrombopoietin receptor agonists (TPO-RA) and tab eltrombopag (50 mg/day) 4 weeks before the transplant, The platelet count started improving, as shown in Figure 1. Two weeks later, a course of intravenous immunoglobulin (IVIg) (400 mg/kg once a day post-dialysis on alternate days for 5 days) was also given. The platelet count improved to 100,000/mm3.
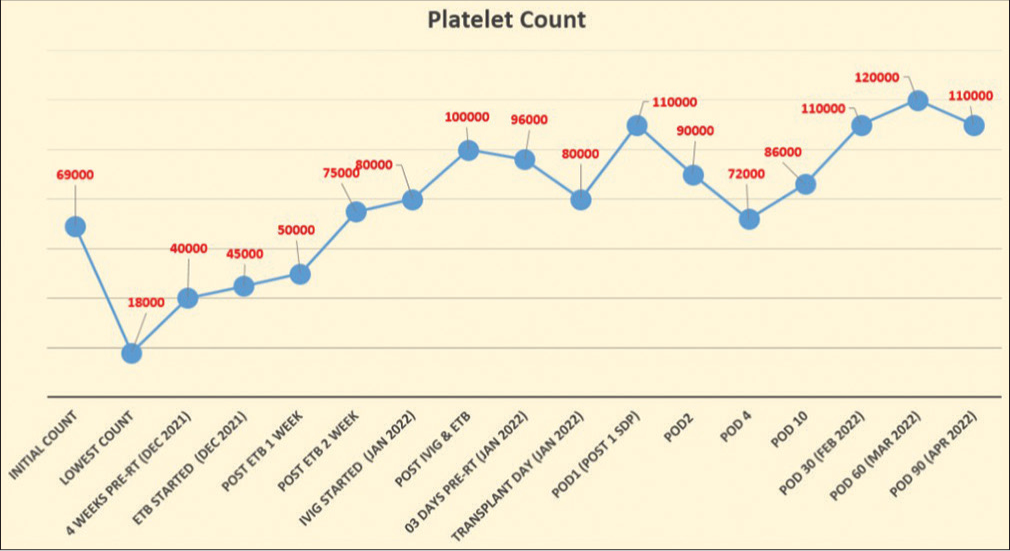
- Platelet count chart. The figure shows a line chart with platelet count charted on y axis and the time lines charted on x axis, starting from 3 months before and after transplant. ETB = eltrombopag, IVIG = intravenous immunoglobulin, POD = postoperative day, RT = renal transplant, SDP = single donor platelet.
As part of pretransplant protocol, the recipient was started on immunosuppressants (mycophenolate and tacrolimus) 2 days pretransplant, given injection methyl prednisone 500 mg on the pre-op day, day of transplant, and postoperative day (POD) 1; and given injection basiliximab 20 mg on day 0 and POD4. His platelet count was 70,000/mm3 on the day of transplant, and hence was given one unit single donor platelet (SDP) transfusion during surgery to maintain a platelet count of 80,000–100,000/mm3. The perioperative period was uneventful with no bleeding complications. The graft functioned well and the creatinine level declined gradually. His platelet count started to improve from POD3 and remained stable. He was continued on oral steroids and other immunosuppression/antibiotic prophylaxis. He had high tacrolimus (CO) level, which was managed with dose reduction. He was discharged after 3 weeks with a stable creatinine of 1.0 mg/dL and a platelet count of 120,000/mm3. Eltrombopag was continued for 4 months and stopped thereafter. He is being continued on prednisone 7.5 mg/day with mycophenolate 500 mg twice a day and tacrolimus. The platelet count remained stable at greater than 60,000 with a count of 75,000/mm3 at 6 months posttransplant, as shown in Figure 1.
Discussion
Successful renal transplant in a case of CKD with ITP is rare.2,4-7 The presentation of ITP may range from asymptomatic with mild thrombocytopenia, mild bruising or petechiae, mucosal bleeding or bleeding from orifices like epistaxis, hematochezia, and hematuria to severe life-threatening bleeds like intracranial bleed or upper gastrointestinal bleed.1 Even asymptomatic ITP patients with low platelets are prone to have increased bleeding during trauma or surgery.1 During transplant surgery, they are especially prone to have excess intraoperative blood loss, anastomotic site leak, hematomas, need of packed red cell transfusions (causing risk of sensitization), and other related complications.4
CKD and ITP may potentiate the bleeding risk and complications of each other. Uremic toxins in CKD interfere with the release of platelet alpha granules and affect platelet adhesion, aggregation, and its interaction with vessel wall, all leading to functional platelet dysfunction.3,4 During dialysis, presence of coexisting B12 deficiency, platelet destruction during dialysis, drug-mediated platelet destruction, heparin-induced thrombocytopenia, and infections like CMV or dengue fever may further compromise platelet count.3 In post-renal transplant state, immunosuppressants and other drugs (like mycophenolate, azathioprine, valganciclovir) and infections (CMV, EBV, parvovirus, dengue) may predispose to thrombocytopenia.5,8 The treatment options for ITP include steroids immunosuppressive drugs (like azathioprine, mycophenolate, cyclosporine, rituximab), and other drugs like danazol, anti-D immunoglobulin, IVIg, with variable responses.1,9 In case of life-threatening thrombocytopenia, pulse steroids and IVIg may be used. Splenectomy is also useful, but it is not frequently done in view of requirement of a major surgery and its lifelong infection risk.1
There are few reported cases of renal transplant in a setting of ITP, as presented in Table 1. Hwang et al.5 and Kanodia et al.4 used preoperative steroids (1 mg/kg dose), pretransplant IVIg, splenectomy, and cyclosporine-based immunosuppression and successfully conducted transplant with no major bleeding and stable graft function. Kanodia et al.4 also used donor-specific leukocyte transfusions, peripheral blood stem cell transfusions, rituximab, and injection methyl prednisone for 7 days in a previously splenectomized patient of chronic ITP.
| Author | Age Sex | NKD | Least Plt (pre-RT) (/mm3) | Initial therapy | RT drugs | Peri-RT therapy for ITP | POD 0 Plt (/mm3) | Complication | Discharge Plt (/mm3), creatinine | Follow-up duration, Plt (/mm3), creatinine (mg/dL) |
|---|---|---|---|---|---|---|---|---|---|---|
| Hwang et al.5 |
35 years Male |
IgAN (CGN) |
12,000 | Steroids 1 mg/kg for 1 month |
Csa MMF Pred |
IVIg POD 1, splenectomy during transplant |
89,000 | Intra-abdominal bleed on POD 1 | 124,000, 1.2 mg/dL |
2 years, stable, stable |
| Kanodia et al.4 |
27 years Female |
-- | 35,000 | Steroids IVIg Splenectomy (3 years back) |
Csa Pred |
PBSC infusion×2, rituximab 600 mg, IVIg 10 g×5 days IV methyl prednisone×7 days |
117,000 | Nil | 97,000, 1.1 mg/dL |
2 years, 40,000, 1.2 mg/dL |
| Agarwal et al.7 |
27 years Female |
CGN | 49,000 | Steroids 1mg/kg, IVIg 1g/kg×2 days, eltrombopag 50 mg/day |
Tac MMF Pred |
IV methyl prednisone, eltrombopag 50 mg/day |
130,000 | Nil | 97,000, 1.4 mg/dL |
1 year, 47,000, 1.3 mg/dL |
| Present case (2022) |
29 years Male |
CGN | 50,000 | Steroids 1mg/kg, eltrombopag 50 mg/day |
Tac MMF Pred |
IV methyl prednisone×5 days, IVIg 400 mg/kg×5 days (pre-RT), eltrombopag 50 mg/day, 1 SDP transfusion |
100,000 | Perinephric collection (self- resolving) | 120,000, 1.2 mg/dL |
6 months, 80,000, 1.2 mg/dL |
CGN=chronic glomerulonephritis, Csa=cyclosporine, IgAN=IgA nephropathy, ITP=immune thrombocytopenia, IV=intravenous, IVIg=intravenous immunoglobulin, MMF=mycophenolate, NKD=native kidney disease, PBSC=peripheral blood stem cells, Plt=platelet count, POD=postoperative day, Pred=prednisone, RT=renal transplant, SDP=single donor platelet concentrates, Tac=Tacrolimus.
Eltrombopag, an oral TPO-RA, binds to the transmembrane and juxta membrane domain of TPOR, resulting in the activation of Janus kinase–signal transducer and mitogen-activated protein kinase pathways, stimulating megakaryocytopoiesis.10 TPO-RA increase the platelet counts and reduce bleeding episodes, and are being increasingly used in ITP as the second-line therapy.10 Eltrombopag is usually initiated at a dose of 50 mg/day with gradual increase in dose if needed. It is well tolerated with common side effects being headache, nasopharyngitis, fatigue, diarrhea, and elevated liver enzymes. Other TPO-RA agonists like romiplostim, which are given subcutaneously and are costlier, may also benefit, but have not been used in previous cases.10 There have been few reports of thrombosis in patients on long-term use of eltrombopag, which needs to be monitored in post-transplant setting.9 To our knowledge, this is the second case report of renal transplantation in a patient with ITP treated with eltrombopag. Agarwal et al.7 have reported a similar case of successful renal transplant in a female patient (refractory to steroids and IVIg) managed with eltrombopag 50 mg OD, with a stable platelet count in the posttransplant period with no bleeding complications. Our case had an uneventful course at 6 months of follow-up with no episode of graft dysfunction or infection. His eltrombopag was stopped after 4 months of transplant in view of thrombotic risk. In case of worsening thrombocytopenia or in cases of tacrolimus-induced thrombotic microangiopathy in the post-transplant period, where tacrolimus needs to be stopped, changing tacrolimus to cyclosporine will be considered, as cyclosporine is more effective in improving the platelet count in ITP.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Updated international consensus report on the investigation and management of primary immune thrombocytopenia. Blood Adv. 2019;3:3780-817.
- [CrossRef] [PubMed] [Google Scholar]
- Renal transplantation and idiopathic thrombocytopenic purpura. Clin Transpl 1986:133.
- [Google Scholar]
- Haemostasis in chronic kidney disease. Nephrol Dial Transplant. 2014;29:29-40.
- [CrossRef] [PubMed] [Google Scholar]
- Renal transplantation in idiopathic thrombocytopenic purpura. Saudi J Kidney Dis Transplant. 2013;24:793-4.
- [CrossRef] [PubMed] [Google Scholar]
- Renal transplantation in a patient with idiopathic thrombocytopenic purpura. Korean J Intern Med. 2005;20:92-5.
- [CrossRef] [PubMed] [Google Scholar]
- Renal transplantation and idiopathic thrombocytopenic purpura: Two case reports. Transplant Proc. 2009;41:2923.
- [CrossRef] [PubMed] [Google Scholar]
- Renal transplant in a patient with idiopathic thrombocytopenic purpura refractory to steroid and intravenous immunoglobulin. Indian J Transplant. 2019;13:228.
- [CrossRef] [Google Scholar]
- Impact of immunosuppressive strategies on post-kidney transplantation thrombocytopenia. Transplant Proc. 2021;53:941-9.
- [CrossRef] [PubMed] [Google Scholar]
- Thrombotic risk in patients with primary immune thrombocytopenia is only mildly increased and explained by personal and treatment-related risk factors. J Thromb Haemost. 2014;12:1266-73.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and safety of eltrombopag in persistent and newly diagnosed ITP in clinical practice. Int J Hematol. 2017;106:508-16.
- [CrossRef] [PubMed] [Google Scholar]







