Translate this page into:
Successful Treatment of Anti-Factor H Antibody-Associated Atypical Hemolytic Uremic Syndrome
Address for correspondence: Dr. Tomoo Kise, Division of Pediatric Nephrology, Okinawa Prefectural Nanbu Medical Center, Children's Medical Center, Arakawa 118-1, Haebaru, Okinawa 901-1193, Japan. E-mail: kitomoo@yahoo.co.jp
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Anti-complement factor H (CFH) autoantibody (Ab)-associated atypical hemolytic uremic syndrome (aHUS) has a poor prognosis in terms of frequent relapses. Although eculizumab is an effective treatment for this type of aHUS, the method of eculizumab discontinuation is not yet established. Herein, we report a case of anti-CFH Ab-associated aHUS in a 6-year-old boy. Eculizumab induction therapy following plasma exchange improved his condition. After 14 months, eculizumab was discontinued because of meningococcal bacteremia. After 6 months of eculizumab cessation, prednisolone (20 mg/alternate days) and mycophenolate mofetil (500 mg/day) were initiated. There were no relapses or increases in anti-CFH Ab titers for 26 months after treatment initiation. We believe that eculizumab induction therapy, following plasma exchange and maintenance therapy with immunosuppressants after eculizumab discontinuation are effective treatments for anti-CFH Ab-related aHUS.
Keywords
Anti-CFH antibody
aHUS
child
eculizumab
Introduction
Atypical hemolytic uremic syndrome (aHUS) is a rare form of thrombotic microangiopathy (TMA) defined by microangiopathic hemolytic anemia, acute renal failure, and thrombocytopenia. Anti-complement factor H (CFH) autoantibody (Ab)-associated aHUS accounts for up to 6%–10% of all aHUS cases, and it has a poor prognosis in terms of frequent relapses.[1] Although eculizumab is an effective treatment for this type of aHUS,[2] some cases require eculizumab cessation because of its side effects. However, the method of eculizumab discontinuation is not yet established.
Herein, we report the case of a 6-year-old boy with anti-CFH Ab-associated aHUS, in which a good clinical course was achieved under plasma exchange (PE) and eculizumab as induction therapy, followed by glucocorticoids and mycophenolate mofetil (MMF) as maintenance therapy. After eculizumab was discontinued because of meningococcal bacteremia, continuous antibody reduction was achieved.
Case Report
A 6-year-old boy with no notable past medical history was admitted to our hospital with a diagnosis of HUS. He had vomiting and abdominal pain for 5 days and had consulted another doctor. He was diagnosed as having HUS on the basis of the presence of anemia, thrombocytopenia, and renal dysfunction. On admission, laboratory data showed hemolytic anemia [hemoglobin, 4.4 g/dL; lactate dehydrogenase (LDH), 4060 U/L; haptoglobin, <10 g/L], thrombocytopenia (platelets, 110,000/μL, which decreased to 20,000/μL, on the fourth day of admission), renal dysfunction (blood urea nitrogen, 62 mg/dL; serum creatinine, 0.96 mg/dL; estimated glomerular filtration rate, 48 mL/min/1.73 m 2 by the modified Schwartz formula), and hypocomplementemia (C3, 38 mg/dL; normal range, 73–138 mg/dL). Schistocytes were present in the peripheral blood smear. The results of direct Coombs test were negative. We were concerned that if we performed blood transfusion without dialysis, the patient would develop hypervolemia and hyperkalemia. Because the white blood cell count was as high as 24,000/μL, we were worried that the severity of the case would increase and renal failure would worsen.[3] For these two reasons, we started hemodialysis.
When we diagnosed HUS and started hemodialysis, we thought that the diagnosis may be aHUS because the levels of complement C3 were low and the patient had no diarrhea. Although PE or eculizumab is effective for the treatment of aHUS, in this case, we believed that PE in combination with hemodialysis would be easier to start than PE alone. Therefore, the initial therapy consisted of continuous hemodiafiltration for 3 days and PE (75 mL/kg, fresh-frozen plasma; three sessions). Upon diagnosing aHUS, after excluding typical HUS and thrombotic thrombocytopenic purpura (TTP), we planned to discontinue PE and start eculizumab. The platelet count increased to 82,000/μL 3 days after PE and to 280,000/μL 7 days after PE. Blood and stool cultures were negative, serum antibody tests against O157 lipopolysaccharides were negative, and ADAMTS13 protease activity was normal (70%). At this time, our diagnosis was definite aHUS. We initiated eculizumab weekly for 2 weeks and thereafter biweekly (loading dose, 600 mg; maintenance dose, 300 mg) after vaccination with a meningococcal conjugate (serogroups A, C, Y, and W135). Two months later, we detected anti-CFH Abs [plasma titer 2882.4 AU/mL (normal range + 3 standard deviation (SD): 5.2 + 4.7 AU/mL)], and there was no genetic abnormality in CFH, CFI, CFB, C3, CFHR1/3, membrane cofactor protein, and thrombomodulin causing aHUS. As we could not measure antibody titer at our facility, we asked the Division of Nephrology and Endocrinology of the University of Tokyo and the Japanese Association for Complement Research to measure the antibody titers. The two laboratories used Abnova's CFH-IgG enzyme-linked immunosorbent assay kit for antibody titer measurement. The levels of autoantibodies in the control population from the region according to measurements using the assay kits were 3.89–10.6 AU/mL (serum) and 3.89–11.7 AU/mL (plasma) per the Japanese Association for Complement Research and 5.2 + 4.7 AU/mL per the Division of Nephrology and Endocrinology of the University of Tokyo. The Division of Nephrology and Endocrinology of the University of Tokyo used the Sanger method for measurement, whereas the Japanese Association for Complement Research used the next-generation method for measurement. The Japanese Association for Complement Research conducted examinations for the deletion of CFHR1/3, and there was no abnormality.
As the patient's parents did not consent to the addition of prednisolone and immunosuppressant to eculizumab, we could not administer those medications.
Ten months later, he was admitted to our hospital because of fever and vomiting. Blood data showed no recurrence of aHUS (hemoglobin, 14.1 g/dL; platelets, 277,000/μL; blood urea nitrogen, 18 mg/dL; serum creatinine, 0.38 mg/dL). Neisseria meningitidis was detected in the blood culture at hospitalization. Cerebrospinal fluid culture was negative. He was then diagnosed with meningococcal bacteremia. He was discharged 10 days after cefotaxime administration. Eculizumab was discontinued 14 months after initiation of the therapy because there was no recurrence of aHUS for 14 months, and low anti-CFH Ab titers after PE and meningococcal bacteremia associated with eculizumab were detected. After 6 months of eculizumab cessation, we initiated prednisolone (20 mg/alternate days) and MMF (500 mg/day) because the patient's parents agreed to this therapy. The patient's parents wanted to continue the treatment with eculizumab until they had moved near the hospital, which was 4 months later. They were instructed to perform home-based urine dipstick test three times a week. Moreover, they were instructed to visit the hospital if the patient developed fever, nausea, and vomiting or appeared sick.
According to Loirat's report, we planned to discontinue eculizumab first, when the anti-CFH Ab titer was <1000 AU/mL, followed by the discontinuation of prednisolone and MMF, when the anti-factor H antibody titer remained <1000 AU/mL; there was no symptom relapse, and normal C3 levels were maintained for more than 1 year. We decided to use these two medications according to the reports by Loirat et al. and Hackl et al.[45]
After 9 months of maintenance therapy with prednisolone and MMF, the patient's condition showed improvement. No recurrence of aHUS and no side effects of prednisolone and MMF have been found. The anti-CFH Ab titer, serum creatinine level, and LDH level remained stable during 26 months [Figure 1]. The anti-CFH Ab titer at 26 months since initiating treatment was 15.3 AU/mL (normal range + 3 SD: 7.8 + 9.6 AU/mL). In this case, the binding site of the anti-CFH antibody to factor H was not the C-terminus end of the protein.
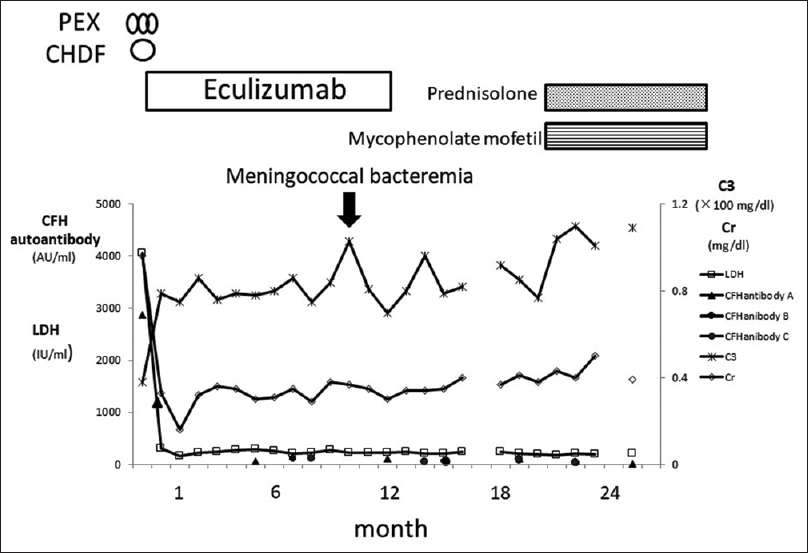
- Change in anti-complement factor H antibody titers, lactate dehydrogenase, and complement C3 and serum creatinine levels during the follow-up time, CFH, complement factor H; CHDF, continuous hemodiafiltration; PEX, plasma exchange; Cr, serum creatinine; LDH, lactate dehydrogenase; C3, complement C3; CFH autoantibody A, antibody titer measured by Division of Nephrology and Endocrinology, The University of Tokyo; CFH autoantibody B, antibody titer measured in plasma by The Japanese Association for Complement Research; CFH autoantibody C, antibody titer measured in serum by The Japanese Association for Complement Research. Since the lot number of the enzyme-linked immunosorbent assay used for the analysis is different, it is impossible to strictly compare the past result with the current result
Discussion
Eculizumab therapy, following PE, and maintenance therapy with prednisolone and MMF after eculizumab cessation are effective treatments for anti-CFH Ab-related aHUS relapses. Dragon-Durey et al. reported that relapses occurred in 58% of patients and that the relapses occurred in 68% of patients during the first 6 months after onset.[1] Loirat et al. proposed a treatment algorithm for anti-CFH Ab-related aHUS. The initial therapy is either eculizumab or PE. The secondary therapy is to add corticosteroids and MMF while continuing eculizumab. Subsequently, eculizumab is discontinued when the anti-CFH Ab titer falls below 1000 AU/mL, and corticosteroids and MMF are continued.[4] Our patient has not had a relapse even once in 26 months. The regimen was effective in lowering anti-CFH Ab titers by PE. The cause of the absence of elevated antibody titer and disease relapse in 6 months from eculizumab discontinuation to initiation of immunosuppressant was unknown. After the initiation of immunosuppressant therapy, maintenance of low antibody titer and prevention of disease relapse were expected. As the results based on anti-CFH Ab titer take a few months to obtain, initial therapy with eculizumab is necessary to prevent severe injury of vital organs until anti-CFH Ab-related aHUS is diagnosed. The efficacy of eculizumab has been reported for this form of aHUS.[26] Immunosuppressive therapy, including corticosteroids, cyclophosphamide, and MMF, suppresses anti-CFH Ab production.[7] The use of eculizumab in combination with steroids and immunosuppressive drugs and its discontinuation upon confirmation of a reduction in the anti-factor H antibody levels are recommended.[8] Although the initiation of immunosuppressants was delayed in this case, we aim for its early initiation in the future.
Eculizumab is an effective treatment for aHUS. However, there are limitations to its use, such as the risk of meningococcal infection, high cost, and uncertainty in its safety on long-term use. Discontinuation of eculizumab has two problems: there are no discontinuation criteria and detecting relapse after discontinuation is difficult. First, as there are no discontinuation criteria, the standard maintenance therapy of aHUS is life-long eculizumab administration. In childhood-onset aHUS, drug cessation is not recommended.[46] The exception is anti-CFH Ab-related aHUS. In anti-CFH Ab-related aHUS, discontinuation is suggested when the antibody titer is low and the patient's condition is stable. Regarding the antibody titer for drug discontinuation, Loirat et al. recommend less than 1000 AU/mL and Ardissino et al. recommend less than 2.5 times the upper limit of normal.[49] However, with differences in measurement kits used, simple comparison of antibody titers is difficult. A consensus assay using a standard arbitrary unit scale is required. Second, to detect relapse after eculizumab cessation, Ardissino et al. recommended monitoring urine dipstick test three times a week at home for early detection of relapse of aHUS after eculizumab cessation.[10] In the presented case, normal urinalysis result was a relief for the patient's family. In anti-CFH antibody-related aHUS, the risk of relapse depends on the antibody titer. Hackl et al. reported that monthly monitoring of the titer led to therapeutic intervention before the appearance of clinical symptoms.[8] If we can measure antibody titer monthly at our own facility, we can detect relapse before the appearance of clinical symptoms. We expect that antibody titers can be measured on a commercial basis.
CFHR1 deficiency is strongly associated with anti-H antibody production. Hofer et al. reported that 82% of CFHR1-deficient aHUS patients had anti-H antibodies.[11] CFHR1 deficiency was not noted in our case. Hofer et al. also reported that 6% of patients without CFHR1 deficiency had anti-H antibodies.[11] The mechanism of anti-H factor production in cases without CFHR1 deficiency is not known. Nozal and Lopez-Trascasa reported that anti-CFH antibodies in aHUS can recognize the C-terminus end of factor H, prevent factor H from binding to endothelial cells, and help in the regulation of the alternative pathway.[12] According to the report of Shiga Medical University, the binding site of anti-CFH antibody to factor H in our case was not the C-terminus end of the protein. This may be related to the absence of relapse.
In conclusion, we believe that eculizumab induction therapy, following PE and maintenance therapy with immunosuppressants after eculizumab discontinuation are effective treatments strategy for anti-CFH Ab-related aHUS. Accumulation of additional cases and long-term follow-up are required.
We obtained informed consent for the publication of this case from the parents of this patient.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors thank Dr. Yoshida and Dr. Kato at the University of Tokyo for measuring anti-complement factor H antibody and genetic testing; and Dr. Inoue of The Japanese Association for Complement Research for measuring anti-complement factor H antibody, complement, and genetic testing, and Dr. Sawai of Shiga University of Medical Science for examining the binding site of the anti-complement factor H antibody to factor H. We would like to thank Editage (www. editage.jp) for English language editing.
References
- Clinical features of anti-factor H autoantibody-associated hemolytic uremic syndrome. J Am Soc Nephrol. 2010;21:2180-7.
- [Google Scholar]
- Eculizumab in anti-factor H antibodies associated with atypical hemolytic uremic syndrome. Pediatrics. 2014;133:e1764-8.
- [Google Scholar]
- Risk factors for the development of Escherichia coli O157:H7 associated with hemolytic uremic syndrome. Pediatr Int. 1999;41:218-22.
- [Google Scholar]
- An international consensus approach to the management of atypical hemolytic uremic syndrome in children. Pediatr Nephrol. 2016;31:15-39.
- [Google Scholar]
- Successful discontinuation of eculizumab under immnosuppressive therapy in DEAP-HUS. Pediatr Nephrol. 2017;32:1081-7.
- [Google Scholar]
- Belgian consensus statement on the diagnosis and management of patients with atypical hemolytic uremic syndrome. Acta Clinica Belgica. 2018;73:80-9.
- [Google Scholar]
- Long-term remission of atypical HUS with anti-factor H antibodies after cyclophosphamide pulses. Pediatr Nephrol. 2014;29:75-83.
- [Google Scholar]
- Anticomplement treatment in atypical and typical hemolytic uremic syndrome. Semin Hematol. 2018;55:150-8.
- [Google Scholar]
- Discontinuation of eculizumab treatment in atypical hemolytic uremic syndrome: An update. AJKD. 2015;66:170-1.
- [Google Scholar]
- Discontinuation of eculizumab maintenance treatment for atypical hemolytic uremic syndrome: A report of 10 cases. Am J Kidney. 2014;64:633-7.
- [Google Scholar]
- for the German-Austrian HUS study Group. Complement factor H-related protein 1 deficiency and factor H antibodies in pediatric patients with atypical hemolytic uremic syndrome. Clin J Am Soc Nephrol. 2013;8:407-15.
- [Google Scholar]
- Autoantibodies against alternative complement pathway proteins in renal pathologies. Nefrologia. 2016;36:489-95.
- [Google Scholar]







