Translate this page into:
Tacrolimus-Associated Cerebral Vasculopathy Presenting with Recurrent Intracerebral Hemorrhage
Address for correspondence: Dr. Praveen Kumar Etta, Department of Nephrology and Kidney Transplantation, TX Hospitals, Hyderabad, Telangana, India. E-mail: drpraveen85@gmail.com
-
Received: ,
Accepted: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor,
Recurrent intracerebral hemorrhage (ICH) is usually a result of uncontrolled hypertension. It can sometimes coexistwith posterior reversible encephalopathy syndrome (PRES). Herein, we present a kidney transplant recipient (KTR) diagnosed with tacrolimus-associated cerebral vasculopathy leading to recurrent ICH, associated with neither uncontrolled hypertension nor PRES, necessitating drug withdrawal.
A 47-year-old deceased donor KTR presented with sudden-onset headache, altered behavior, and focal seizures 2 years post-transplant. Her native kidney disease was presumed to be chronic interstitial nephritis. She was on peritoneal dialysis for 4 years before transplant. She had received induction with equine antithymocyte globulin and was taking the standard triple-drug immunosuppression. Her posttransplant clinical course was uneventful, except for development of posttransplant diabetes mellitus at 3 months following transplant, which was under control with metformin monotherapy. Her blood pressure was always under control. She had no other comorbid illnesses. She was having stable graft function (serum creatinine 0.8 mg/dL). Tacrolimus trough level was 4.6 ng/mL. Computed tomography (CT) of the brain showed ICH with large hematoma (50 × 40 mm) in the left parieto-occipital region with perifocal edema. Past history was significant with two similar episodes of ICH 7 and 15 months ago, affecting the right frontal lobe (30 × 20 mm) and the right temporoparietal lobe (40 × 20 mm) [Figure 1].
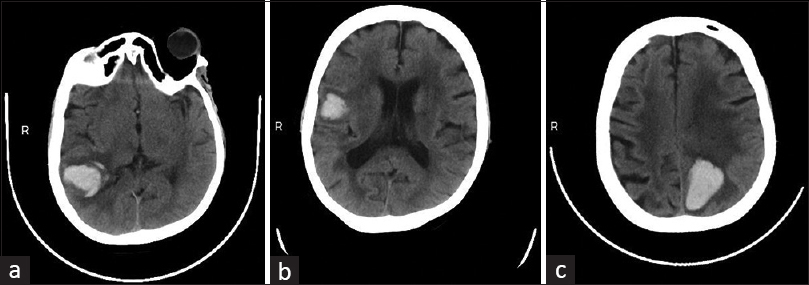
- Computed tomography axial images of the brain showing ICHs at three different time points in the same patient. (a) First episode of ICH affecting the right temporoparietal lobe at 9 months posttransplant (40 × 20 mm). (b) Second episode affecting the right frontal lobe at 17 months posttransplant (30 × 20 mm). (c) Third episode affecting the left parieto-occipital region at 24 months posttransplant (50 × 40 mm). ICH = intracerebral hemorrhage
Recurrent ICH can result from uncontrolled hypertension, coagulopathies, arteriovenous malformations, aneurysms, neoplasms, vasculitis, infections (especially, herpes simplex virus encephalitis), PRES syndrome, and amyloid angiopathy. All the three episodes of ICH were associated with neither severe hypertension nor trauma. She was extensively evaluated with CT angiogram, magnetic resonance angiography, and venography. As there was no apparent predisposing cause, drug-induced toxicity was suspected. Tacrolimus was stopped, and she was shifted to low-dose cyclosporine. Cyclosporine trough whole blood level was targeted between 75 and 100 ng/mL. At 12 months follow-up, she is doing well with no further neurological events.
Neurotoxicity is one of the common complications of calcineurin inhibitors (CNIs). The severity of symptoms varies from mild and self-limiting to severe and life-threatening. These include tremors, ataxia, agitation, confusion, nightmares, headache, visual disturbances, focal neurological deficits, cortical blindness, altered mental status, encephalopathy, seizures, and coma. These are generally more common with tacrolimus than cyclosporine. Several cases of ICH after solid organ transplantation have been reported, but mostly in the setting of PRES and rarely due to cerebral venous sinus thrombosis. Tacrolimus is well known to precipitate PRES, and ICH is known to occur in PRES.[1] Tacrolimus is also known to induce reversible cerebral vasoconstriction syndrome, thereby precipitating ICH. However, in our patient, the three episodes of ICH were not associated with clinical or imaging evidence of PRES. Blood pressure was moderately elevated in all the three episodes. Neither there was an evidence of coagulopathy, nor she was on coagulation altering medication. After excluding all the common possible causes of ICH, we concluded it as tacrolimus-associated cerebral vasculopathy presenting with recurrent ICH.
Stereotactic brain biopsy-proven tacrolimus-associated cerebral vasculitis with distinct microglia activation was initially described in a liver transplant recipient.[2] Later, it was identified that tacrolimus-induced ICH was significantly more common after allogeneic bone marrow transplantation than after solid organ transplantation. Various pathophysiological mechanisms have been proposed. Calcineurin is expressed in several areas of the brain such as cerebral cortex, striatum, substantia nigra, cerebellum, and hippocampus. CNIs, especially tacrolimus, can cause direct endothelial cell injury and alteration of the blood–brain barrier (BBB). Experimental studies conducted in vitro on mouse brain capillary endothelial cells have shown a direct cytotoxic effect of tacrolimus on endothelial cells.[3] It was also confirmed in autopsies.[4] It is also known to induce vasoconstriction through endothelial cell production and release of endothelin, systemic sympathetic stimulation, and reduced nitric oxide production. Systemic and/or renal vasoconstriction with resultant hypertension could lead to reduced cerebral blood flow due to autoregulatory vasoconstriction. In addition, these drugs could reduce cerebral blood flow directly, secondary to cerebral vasoconstriction. The combined effects might lead to increased but complex cerebral vascular instability, with an increased risk of ICH. Disruption of the BBB and the cytotoxic effects on the vascular endothelium result in leakage of fluid into the interstitium, which leads to vasogenic edema. This, in turn, may progress to ICH. Tacrolimus-induced cerebral microbleeds may predispose to symptomatic ICH.
Tacrolimus causing ICH secondary to cerebral vasculopathy seems to be a rare event. Only one similar case has been reported in a KTR till date.[5] However, recurrent ICH was never reported in the past. ICH may be a marker of tacrolimus-associated vasculopathy. High index of suspicion and early intervention in the form of drug withdrawal may prevent its recurrence. Although the exact pathogenesis of ICH remains unknown, tacrolimus could play a direct role in the occurrence of this process regardless of the drug levels as it may remain within the therapeutic range. It remains a diagnosis of exclusion after ruling out the common predisposing causes for ICH. This case illustrates that tacrolimus-associated vasculopathy can occur even at the therapeutic level of tacrolimus in the blood and it can predispose to ICH, which can be recurrent.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Posterior reversible encephalopathy syndrome and hemorrhage associated with tacrolimus in a pediatric heart transplantation recipient. Pediatr Transplant. 2013;17:E67-70.
- [Google Scholar]
- Cerebral vasculitis during FK 506 treatment in a liver transplant patient. Neurology. 1998;50:1154-7.
- [Google Scholar]
- Induction of apoptosis in mouse brain capillary endothelial cells by cyclosporin A and tacrolimus. Life Sci. 2000;66:2255-60.
- [Google Scholar]
- Tacrolimus leukoencephalopathy: A neuropathologic confirmation. Neurology. 2004;63:1132-3.
- [Google Scholar]
- Therapeutic drug level of tacrolimus causing intracranial hemorrhage in a patient with renal transplant. Clin Case Rep. 2022;10:e05788.
- [Google Scholar]






